What is myocardial infarction
Myocardial infarction also called acute myocardial infarction, is a medical term for a “heart attack” that happens when the flow of blood to your heart suddenly becomes blocked. The blockage is most often a buildup of fat, cholesterol and other substances, which form a plaque in the arteries that feed the heart (coronary arteries). The plaque eventually breaks away and forms a clot. The interrupted blood flow can damage or destroy part of the heart muscle. If not treated quickly, the heart muscle begins to die. But if you do get quick treatment, you may be able to prevent or limit damage to the heart muscle. That’s why it’s important to know the symptoms of a myocardial infarction and call your local emergency services number if you or someone else is having them. You should call your local emergency services number, even if you are not sure that it is a myocardial infarction. The current 2018 clinical definition of myocardial infarction requires the confirmation of the myocardial ischemic injury with abnormal cardiac biomarkers 1. Myocardial infarction is a clinical syndrome involving myocardial ischemia, ECG changes and chest pain 2.
Myocardial infarction may be “silent” and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death 3. Most myocardial infarctions are due to underlying coronary artery disease, the leading cause of death in the United States. With coronary artery occlusion, the myocardium is deprived of oxygen. Prolonged deprivation of oxygen supply to the myocardium can lead to myocardial cell death and necrosis 4. Patients can present with chest discomfort or pressure that can radiate to the neck, jaw, shoulder, or arm. In addition to the history and physical exam, myocardial ischemia may be associated with ECG changes and elevated biochemical markers such as cardiac troponins 5.
Each year over 1 million Americans have a myocardial infarction. Myocardial infarction can be fatal, but treatment has improved dramatically over the years. It’s crucial to call your local emergency number for emergency medical help if you think you might be having a heart attack.
The most common cause of death and disability in the western world and worldwide is coronary artery disease 6. Based on 2015 mortality data from the National Health Interview Survey, myocardial infarction mortality was 114,023, and myocardial infarction any-mention mortality (i.e., myocardial infarction is mentioned as a contributing factor in the death certificate) was 151,863 7.
As per the National Health and Nutrition Examination Survey (NHANES)-CDC data from 2011 to 2014 an estimated 16.5 million Americans older than 20 years of age have coronary artery disease, and the prevalence was higher in males than females for all ages. As per the NHANES 2011 through 2014, the overall prevalence of myocardial infarction is 3.0% in US adults older than 20 years of age.
Prevalence of myocardial infarction in the US Sub-Populations
Non-Hispanic Whites
- 4.0% (Male)
- 2.4% (Female)
Non-Hispanic Blacks
- 3.3% (Male)
- 2.2% (Female)
Hispanics
- 2.9% (Male)
- 2.1% (Female)
Non-Hispanic Asians
- 2.6% (Male)
- 0.7% (Female)
Based on the Atherosclerosis Risk in Communities Study performed by National Heart, Lung and Blood Institute collected between 2005 and 2014, the estimated annual incidence is 605,000 new myocardial infarctions and 200,000 recurrent myocardial infarctions 8.
The Atherosclerosis Risk in Communities Study study also found that the average age at first myocardial infarction is 65.6 years for males and 72.0 years for females. In the past decades, several studies have shown a declining incidence of myocardial infarction in the United States 8.
The most common myocardial infarction symptoms in men and women are:
- Chest discomfort. It is often in center or left side of the chest. It usually lasts more than a few minutes. It may go away and come back. It can feel like pressure, squeezing, fullness, or pain. It also can feel like heartburn or indigestion.
- Shortness of breath. Sometimes this is your only symptom. You may get it before or during the chest discomfort. It can happen when you are resting or doing a little bit of physical activity.
- Discomfort in the upper body. You may feel pain or discomfort in one or both arms, the back, shoulders, neck, jaw, or upper part of the stomach.
You may also have other symptoms, such as nausea, vomiting, dizziness, and lightheadedness. You may break out in a cold sweat. Sometimes women will have different symptoms then men. For example, they are more likely to feel tired for no reason.
The most common cause of myocardial infarctions is coronary artery disease (coronary heart disease). With coronary artery disease, there is a buildup of cholesterol and other material, called plaque, on their inner walls or the arteries. This is atherosclerosis. It can build up for years. Eventually an area of plaque can rupture (break open). A blood clot can form around the plaque and block the artery.
A less common cause of myocardial infarction is a severe spasm (tightening) of a coronary artery. The spasm cuts off blood flow through the artery.
At the hospital, your doctor make a diagnosis based on your symptoms, blood tests, and different heart health tests. Treatments may include medicines and medical procedures such as coronary angioplasty. After a myocardial infarction, cardiac rehabilitation and lifestyle changes can help you recover.
Act immediately. Some people wait too long because they don’t recognize the important signs and symptoms. Take these steps:
- Call for emergency medical help. If you suspect you’re having a myocardial infarction, don’t hesitate. Immediately call your local emergency number. If you don’t have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only if there are no other options. Because your condition can worsen, driving yourself puts you and others at risk.
- Take nitroglycerin, if prescribed to you by a doctor. Take it as instructed while awaiting emergency help.
- Take aspirin, if recommended. Taking aspirin during a myocardial infarction could reduce heart damage by helping to keep your blood from clotting. Aspirin can interact with other medications, however, so don’t take an aspirin unless your doctor or emergency medical personnel recommend it. Don’t delay calling your local emergency number to take an aspirin. Call for emergency help first.
What is recurrent myocardial infarction?
Incident myocardial infarction is defined as the individual’s first myocardial infarction. When features of myocardial infarction occur in the first 28 days after the first myocardial infarction, the second event is not counted as a new myocardial infarction for epidemiological purposes. If characteristics of myocardial infarction occur after 28 days following the first myocardial infarction, it is considered to be a recurrent myocardial infarction 9.
What does re-infarction mean?
The term re-infarction is used clinically for an acute myocardial infarction that occurs within 28 days of an incident or recurrent myocardial infarction 9. The ECG diagnosis of suspected re-infarction following the initial myocardial infarction may be confounded by the initial evolutionary ECG changes. Re-infarction should be considered when ST-elevation ≥ 1 mm recurs or new pathognomonic Q waves appear in at least two contiguous leads, particularly when associated with ischaemic symptoms. However, re-elevation of the ST-segment can also be seen in threatened myocardial rupture or in cases of pericarditis, and should lead to additional diagnostic evaluation.
In patients where re-infarction is suspected from clinical signs or symptoms following the initial myocardial infarction, an immediate measurement of cardiac troponin is recommended. A second sample should be obtained 3–6 hours later or earlier with more sensitive cardiac troponin assays. If the cardiac troponin concentration is elevated, but stable or decreasing at the time of suspected re-infarction, the diagnosis of re-infarction requires a > 20% increase of the cardiac troponin value in the second sample 10. If the initial cardiac troponin concentration is normal, the criteria for new acute myocardial infarction apply 11.
Types of myocardial infarction
Myocardial infarction in general can be classified from Type 1 to Type 5 myocardial infarction based on the cause and pathogenesis 12. Type 1 myocardial infarction is due to acute coronary atherothrombotic myocardial injury with plaque rupture. Most patients with ST-segment elevation myocardial infarction (STEMI) and many with non-ST-segment elevation myocardial infarction (NSTEMI) comprise this category. Type 2 myocardial infarction is the most common type of myocardial infarction encountered in clinical settings in which is there is demand-supply mismatch resulting in myocardial ischemia. This demand supply mismatch can be due to multiple reasons including but not limited to presence of a fixed stable coronary obstruction, tachycardia, hypoxia or stress. However, the presence of fixed coronary obstruction is not necessary. Other potential etiologies include coronary asospasm, coronary embolus, and spontaneous coronary artery dissection (SCAD). Sudden cardiac death patients who succumb before any troponin elevation comprise Type 3 myocardial infarction. Types 4 and 5 myocardial infarctions are related to coronary revascularization procedures like Percutaneous Coronry Intervention (PCI) or Coronary artery Bypass Grfting (CABG).
For the sake of immediate treatment strategies such as reperfusion therapy, it is usual practice to designate myocardial infarction in patients with chest discomfort or other ischemic symptoms, who develop new ST-segment elevations in two contiguous leads or new bundle branch blocks with ischemic repolarization patterns as an ST-elevation myocardial infarction (STEMI). In contrast, patients without ST-segment elevation at presentation are usually designated non-ST-elevation myocardial infarction (NSTEMI). The categories of patients with STEMI, NSTEMI, or unstable angina are customarily included in the concept of acute coronary syndrome (ACS) 13. Unstable angina is similar to NSTEMI. However, cardiac markers are not elevated 14. In addition to these categories, myocardial infarction may be classified into various types based on pathological, clinical, and prognostic differences, along with different treatment strategies.
There is no universal consensus on the cardiac troponin (cTn) or high-sensitivity cardiac troponin (hs-cTn) cut-off points that clearly distinguish cardiac procedural myocardial injury from myocardial infarction 15. The distinction is made on the basis of an injury created by a flow-limiting complication during the procedure that results in sufficient myocardial ischemia to generate a procedure-related myocardial infarction. The size of the insult will determine the magnitude of the cardiac troponin release. Various groups have used multiples of the 99th percentile upper reference limit and set thresholds to diagnose periprocedural myocardial infarctions for clinical trials 16. Unless a standard assay is used for all analyses, given the heterogeneity of cardiac troponin assays, this approach could lead to very different values depending on the assay used locally. The Academic Research Consortium-2 (ARC-2) suggests a post-procedural cardiac troponin value ≥ 35 times the 99th percentile upper reference limit for both PCI and CABG in patients that have a normal baseline cardiac troponin value or in patients with elevated pre-procedure cardiac troponin values in whom the cardiac troponin levels are stable or falling. ARC-2 proposes that one ancillary criterion be required in addition to the ≥ 35 cardiac troponin rise to fulfill the definition of periprocedural myocardial infarction. The ancillary criteria are one or more of the following: new significant Q waves (or equivalent), flow-limiting angiographic complications in a major epicardial vessel or > 1.5 mm diameter branch, or a substantial new loss of viable myocardium on echocardiography related to the procedure 16. Furthermore, the Academic Research Consortium-2 (ARC-2) has defined stand-alone criteria for significant procedural myocardial injury if the rise in cardiac troponin is ≥ 70 times the 99th percentile upper reference limit (where the baseline is lower than the upper reference limit, elevated and stable, or falling) 16.
Non-ST-segment elevation myocardial infarction (NSTEMI)
Acute coronary syndrome (ACS) is simply a mismatch in the myocardial oxygen demand and myocardial oxygen consumption 13. While the cause of this mismatch in ST-elevation myocardial infarction (STEMI) is nearly always coronary plaque rupture resulting in thrombosis formation occluding a coronary artery, there are several potential causes of this mismatch in non-ST-elevation myocardial infarction (NSTEMI). There may be a flow-limiting condition such as a stable plaque, vasospasm as in Prinzmetal angina, coronary embolism, or coronary arteritis. Non-coronary injury to the heart such as cardiac contusion, myocarditis, or presence of cardiotoxic substances can also produce NSTEMI 13. Finally, conditions relatively unrelated to the coronary arteries or myocardium itself such as hypotension, hypertension, tachycardia, aortic stenosis, and pulmonary embolism lead to NSTEMI because the increased oxygen demand cannot be met 17, 18. NSTEMI is diagnosed in patients determined to have symptoms consistent with ACS and troponin elevation but without ECG changes consistent with STEMI. Unstable angina and NSTEMI differ primarily in the presence or absence of detectable troponin leak.
The “typical” presentation of NSTEMI is a pressure-like substernal pain, occurring at rest or with minimal exertion. The pain generally lasts more than 10 minutes and may radiate to either arm, the neck, or the jaw 13. The pain may be associated with shortness of breath (dyspnea), nausea or vomiting, syncope (fainting), fatigue, or excess sweatiness (diaphoresis). Sudden onset of unexplained shortness of breath (dyspnea) with or without associated symptoms is also a common presentation. Risk factors for acute coronary syndrome (ACS) include male sex, older age, family history of coronary artery disease, diabetes, personal history of coronary artery disease, and renal insufficiency. Atypical symptoms may include a stabbing or pleuritic pain, epigastric or abdominal pain, indigestion, and isolated dyspnea. While all patients presenting with acute coronary syndrome (ACS) are more likely to present with typical symptoms than atypical symptoms, the likelihood of atypical presentations increases with age over 75, women and those with diabetes, renal insufficiency, and dementia.
Physical exam for acute coronary syndrome (ACS) and NSTEMI is often nonspecific. Clues such as back pain with aortic dissection or pericardial friction rub with pericarditis may point to an alternative diagnosis for a patient’s chest pain, but no such exam finding exists that indicates acute coronary syndrome (ACS) as the most likely diagnosis. Signs of heart failure should increase concern for acute coronary syndrome (ACS) but are, again, nonspecific findings 19, 20.
ST-segment elevation myocardial infarction (STEMI)
ST-segment elevation myocardial infarction (STEMI) also known as acute ST-elevation myocardial infarction occurs due to occlusion of one or more coronary arteries, causing transmural myocardial ischemia (full thickness heart muscle ischemia) which in turn results in myocardial injury or necrosis 21. An ST-elevation myocardial infarction (STEMI) occurs from occlusion of one or more of the coronary arteries that supply your heart with blood. The cause of this abrupt disruption of blood flow is usually plaque rupture, erosion, fissuring or dissection of coronary arteries that results in an obstructing thrombus. The major risk factors for ST-elevation myocardial infarction (STEMI) are dyslipidemia, diabetes mellitus, hypertension, smoking, and family history of coronary artery disease 22.
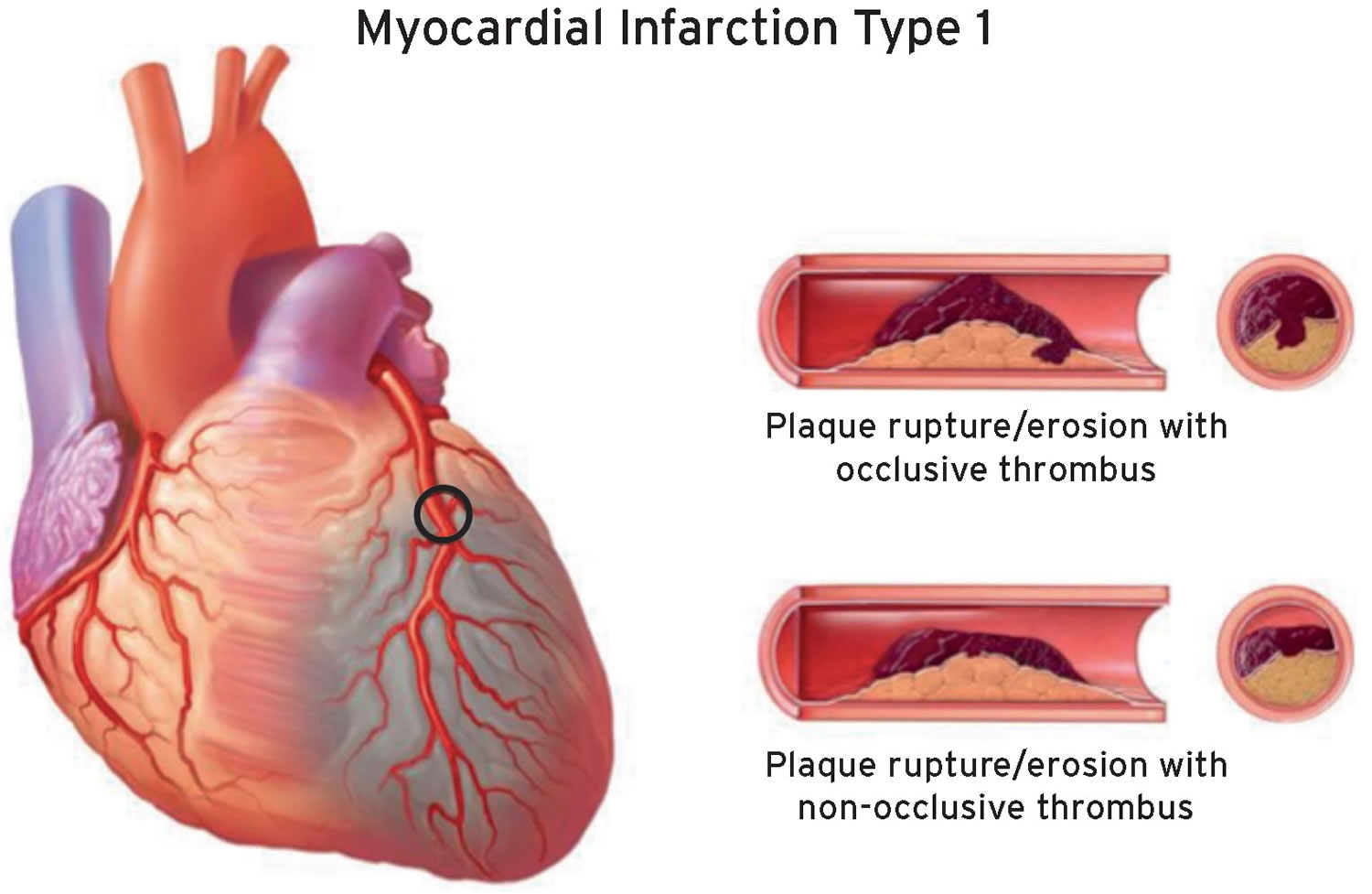
Type 1 myocardial infarction
Myocardial infarction caused by atherothrombotic coronary artery disease (coronary heart disease) and usually precipitated by atherosclerotic plaque disruption (rupture or erosion) is designated as a type 1 myocardial infarction 15. The relative burden of atherosclerosis and thrombosis in the culprit lesion varies greatly and the dynamic thrombotic component may lead to distal coronary embolization resulting in myocyte necrosis 23. Plaque rupture may not only be complicated by intraluminal thrombosis but also by hemorrhage into the plaque through the disrupted surface (Figure 1).
Criteria for type 1 myocardial infarction 15:
- Detection of a rise and/or fall of cardiac troponin values with at least one value above the 99th percentile upper reference limit and with at least one of the following:
- Symptoms of acute myocardial ischemia;
- New ischemic ECG changes;
- Development of pathological Q waves;
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischemic atiology;
- Identification of a coronary thrombus by angiography including intracoronary imaging or by autopsy.
- Post-mortem demonstration of an atherothrombus in the artery supplying the infarcted myocardium, or a macroscopically large circumscribed area of necrosis with or without intramyocardial hemorrhage, meets the type 1 myocardial infarction criteria regardless of cardiac troponin values.
It is essential to integrate the ECG findings with the aim of classifying type 1 myocardial infarction into STEMI or NSTEMI in order to establish the appropriate treatment according to current Guidelines 24.
Figure 1. Myocardial infarction type 1
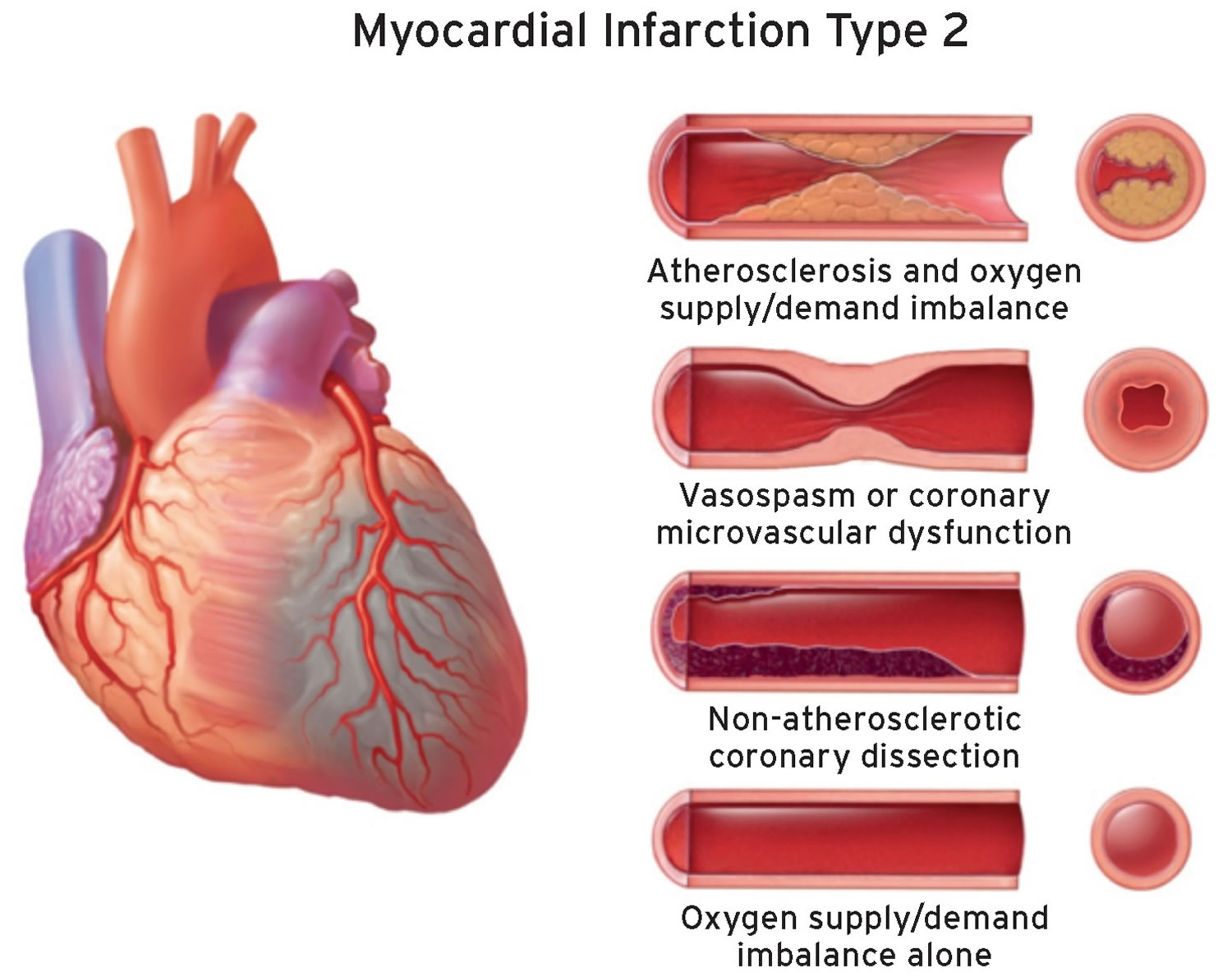
[Source 15 ]Type 2 myocardial infarction
The pathophysiological mechanism leading to ischemic myocardial injury in the context of a mismatch between oxygen supply and demand has been classified as type 2 myocardial infarction 11. By definition, acute atherothrombotic plaque disruption is not a feature of type 2 myocardial infarction. In patients with stable known or presumed coronary artery disease (coronary heart disease), an acute stressor such as an acute gastrointestinal bleed with a precipitous drop in hemoglobin, or a sustained tachyarrhythmia with clinical manifestations of myocardial ischemia, may result in myocardial injury and a type 2 myocardial infarction 15. These effects are due to insufficient blood flow to the ischemic myocardium to meet the increased myocardial oxygen demand of the stressor. Ischemic thresholds may vary substantially in individual patients depending on the magnitude of the stressor, the presence of non-cardiac comorbidities, and the extent of underlying coronary artery disease and cardiac structural abnormalities.
Criteria for type 2 myocardial infarction 15:
- Detection of a rise and/or fall of cardiac troponin values with at least one value above the 99th percentile upper reference limit, and evidence of an imbalance between myocardial oxygen supply and demand unrelated to acute coronary athero-thrombosis, requiring at least one of the following:
- Symptoms of acute myocardial ischaemia;
- New ischemic ECG changes;
- Development of pathological Q waves;
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischemic etiology.
All of the clinical information available should be considered in distinguishing type 1 myocardial infarction from type 2 myocardial infarction. The context and mechanisms of type 2 myocardial infarction should be considered when establishing this diagnosis. The myocardial oxygen supply/demand imbalance attributable to acute myocardial ischemia may be multifactorial, related either to: reduced myocardial perfusion due to fixed coronary atherosclerosis without plaque rupture, coronary artery spasm, coronary microvascular dysfunction (which includes endothelial dysfunction, smooth muscle cell dysfunction, and the dysregulation of sympathetic innervation), coronary embolism, coronary artery dissection with or without intramural hematoma, or other mechanisms that reduce oxygen supply such as severe bradyarrhythmia, respiratory failure with severe hypoxaemia, severe anaemia, and hypotension/shock; or to increased myocardial oxygen demand due to sustained tachyarrhythmia or severe hypertension with or without left ventricular hypertrophy. In patients who undergo timely coronary angiography, description of a ruptured plaque with thrombus in the infarct-related artery may be helpful in making the distinction between type 2 myocardial infarction vs. type 1 myocardial infarction, but angiography is not always definitive, clinically indicated, or required to establish the diagnosis of type 2 myocardial infarction.
Studies have shown variable occurrences of type 2 myocardial infarction depending on criteria used for diagnosis. Some reports rely on specific predetermined oxygen mismatch criteria 25, whereas others apply more liberal criteria. Most studies show a higher frequency of type 2 myocardial infarction in women. The short- and long-term mortality rates for patients with type 2 myocardial infarction are generally higher than for type 1 myocardial infarction patients in most but not all studies due to an increased prevalence of comorbid conditions 25, 26. Coronary atherosclerosis is a common finding in type 2 myocardial infarction patients selected for coronary angiography. In general, these patients have a worse prognosis than those without coronary artery disease 27. Prospective evaluations of the importance of coronary artery disease with type 2 myocardial infarction using consistent definitions and approaches are needed.
It has been shown that the frequency of ST-segment elevation in type 2 myocardial infarction varies from 3–24% 28. In some cases, coronary embolism caused by thrombi, calcium or vegetation from the atria or ventricles, or acute aortic dissection may result in a type 2 myocardial infarction. Spontaneous coronary artery dissection with or without intramural hematoma is another non-atherosclerotic condition that may occur, especially in young women. It is defined as spontaneous dissection of the coronary artery wall with accumulation of blood within the false lumen, which can compress the true lumen to varying degrees (Figure 2) 29.
Figure 2. Myocardial infarction type 2
[Source 15 ]Type 3 myocardial infarction
The detection of cardiac biomarkers in the blood is fundamental for establishing the diagnosis of myocardial infarction 11. However, patients can manifest a typical presentation of myocardial ischemia or myocardial infarction, including presumed new ischemic ECG changes or ventricular fibrillation, and die before it is possible to obtain blood for cardiac biomarker determination; or the patient may succumb soon after the onset of symptoms before an elevation of biomarker values has occurred. Such patients are designated as having a type 3 myocardial infarction, when suspicion for an acute myocardial ischaemic event is high, even when cardiac biomarker evidence of myocardial infarction is lacking 11. This category allows the separation of fatal myocardial infarction events from the much larger group of sudden death episodes that may be cardiac (non-ischemic) or non-cardiac in origin. When a type 3 myocardial infarction is diagnosed and a subsequent autopsy reveals recent evidence of an myocardial infarction, with a fresh or recent thrombus in the infarct-related artery, the type 3 myocardial infarction should be reclassified to a type 1 myocardial infarction. Original investigations addressing the incidence of type 3 myocardial infarction are sparse, but a study showed an annual incidence below 10/100,000 person-years and a frequency of 3–4% among all types of myocardial infarction 30.
Criteria for type 3 myocardial infarction 15:
- Patients who suffer cardiac death, with symptoms suggestive of myocardial ischemia accompanied by presumed new ischemic ECG changes or ventricular fibrillation, but die before blood samples for biomarkers can be obtained, or before increases in cardiac biomarkers can be identified, or myocardial infarction is detected by autopsy examination.
Type 4a myocardial infarction (myocardial infarction associated with percutaneous coronary intervention)
Stand-alone post-procedural increases of cardiac troponin (cTn) values are sufficient to establish a diagnosis of procedural myocardial injury but not for the diagnosis of type 4a myocardial infarction 15. Type 4a myocardial infarction requires an elevation of cardiac troponin values greater than five times the 99th percentile upper reference limit in patients with normal baseline values or, in patients with elevated pre-procedure cardiac troponin in whom the cardiac troponin levels are stable (≤ 20% variation) or falling, the post-procedure cardiac troponin must rise > 20% to an absolute value more than five times the 99th percentile upper reference limit. In addition, there should be evidence of new myocardial ischaemia, either from ECG changes, imaging evidence, or from procedure-related complications associated with reduced coronary blood flow such as coronary dissection, occlusion of a major epicardial artery or a side branch occlusion/thrombus, disruption of collateral flow, slow flow or no-reflow, or distal embolization. The use of high-sensitivity cardiac troponin (hs-cTn) assays to diagnose type 4a myocardial infarction (and type 5 myocardial infarction) is an area of active research. Many high-sensitivity cardiac troponin (hs-cTn) assays are available, which have wide dynamic ranges. Different criteria may be required for different assays. However, it has recently been shown that the optimal hs-cTnT thresholds to predict cardiovascular events at 30 days and 1 year were very close to the five-fold increase suggested by the Third Universal Definition of Myocardial infarction 31. These criteria are therefore retained because of a lack of new scientific evidence that identifies superior criteria for defining this myocardial infarction subtype. Other criteria that meet the definition of type 4a myocardial infarction, regardless of hs-cTn or cTn values, are the development of new pathological Q waves or autopsy evidence of recent procedure-related thrombus in the culprit artery.
Criteria for percutaneous coronary intervention-related myocardial infarction ≤ 48 hours after the index procedure (type 4a myocardial infarction) 15:
- Coronary intervention-related myocardial infarction is arbitrarily defined by an elevation of cardiac troponin (cTn) values more than five times the 99th percentile upper reference limit in patients with normal baseline values. In patients with elevated pre-procedure cTn in whom the cTn level are stable (≤ 20% variation) or falling, the post-procedure cTn must rise by > 20%. However, the absolute post-procedural value must still be at least five times the 99th percentile upper reference limit. In addition, one of the following elements is required:
- New ischemic ECG changes;
- Development of new pathological Q waves;
- Isolated development of new pathological Q waves meets the type 4a myocardial infarction criteria if cTn values are elevated and rising but less than five times the 99th percentile upper reference limit
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischaemic etiology;
- Angiographic findings consistent with a procedural flow-limiting complication such as coronary dissection, occlusion of a major epicardial artery or a side branch occlusion/thrombus, disruption of collateral flow, or distal embolization.
- Post-mortem demonstration of a procedure-related thrombus in the culprit artery, or a macroscopically large circumscribed area of necrosis with or without intra-myocardial hemorrhage meets the type 4a myocardial infarction criteria.
Type 4b myocardial infarction (stent/scaffold thrombosis associated with percutaneous coronary intervention)
Type 4b myocardial infarction, is a subcategory of percutaneous coronary intervention (PCI)-related myocardial infarction due to stent/scaffold thrombosis, as documented by angiography or autopsy using the same criteria utilized for type 1 myocardial infarction 15. It is important to indicate the time of the occurrence of the stent/scaffold thrombosis in relation to the timing of the percutaneous coronary intervention (PCI) procedure. The following temporal categories are suggested: acute, 0–24 hours; subacute, > 24 hours to 30 days; late, > 30 days to 1 year; and very late > 1 year after stent/scaffold implantation 16.
Type 4c myocardial infarction (restenosis associated with percutaneous coronary intervention)
Occasionally myocardial infarction occurs and—at angiography, in-stent restenosis, or restenosis following balloon angioplasty in the infarct territory—is the only angiographic explanation since no other culprit lesion or thrombus can be identified 15. This percutaneous coronary intervention (PCI)-related myocardial infarction type is designated as type 4c myocardial infarction, defined as focal or diffuse restenosis, or a complex lesion associated with a rise and/or fall of cardiac troponin values above the 99th percentile upper reference limit applying, the same criteria utilized for type 1 myocardial infarction.
Type 5 myocardial infarction (myocardial infarction associated with coronary artery bypass grafting)
Numerous factors can lead to procedural myocardial injury during a coronary artery bypass grafting (CABG) procedure. Many of them are related to the details of the cardiac preservation, the extent of the direct traumatic injury to the myocardium, as well as any potential ischemic injury. For that reason, increases in cardiac troponin values should be expected after all CABG procedures 32, which need to be taken into account when comparing the extent of procedural myocardial injury after cardiac surgery with that associated with less invasive approaches. Depending on whether it is off-pump or on-pump surgery, procedural myocardial injury is observed among 32–44% of CABG patients when quantified by late gadolinium enhancement cardiac magnetic resonance 33.
Criteria for CABG-related myocardial infarction ≤ 48 hours after the index procedure (type 5 myocardial infarction) 15:
- CABG-related myocardial infarction is arbitrarily defined as elevation of cardiac troponin values > 10 times the 99th percentile upper reference limit in patients with normal baseline cardiac troponin values. In patients with elevated pre-procedure cardiac troponin in whom cardiac troponin levels are stable (≤ 20% variation) or falling, the post-procedure cardiac troponin must rise by > 20%. However, the absolute post-procedural value still must be > 10 times the 99th percentile upper reference limit. In addition, one of the following elements is required:
- Development of new pathological Q waves;
- Isolated development of new pathological Q waves meets the type 5 myocardial infarction criteria if cardiac troponin values are elevated and rising but < 10 times the 99th percentile upper reference limit.
- Angiographic documented new graft occlusion or new native coronary artery occlusion;
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischemic etiology.
- Development of new pathological Q waves;
Marked isolated elevation of cardiac troponin values within the 48 hours post-operative period, even in the absence of ECG/angiographic or other imaging evidence of myocardial infarction, indicates prognostically significant cardiac procedural myocardial injury 34. The presence of significant procedural myocardial injury in patients with operative problems (e.g. difficulty coming off bypass, technically difficult anastomoses in a heavily calcified aorta, of perioperative evidence of myocardial ischaemia, etc.) should prompt clinical review of the procedure and/or consideration of additional diagnostic testing for possible type 5 myocardial infarction.
The area under the curve (AUC) and routine cardiac troponin sampling has demonstrated an excellent linear relationship with the mass of the new injury as defined by late gadolinium enhancement cardiac magnetic resonance. The area under the curve for creatine kinase MB isoform (CK-MB) is also good, although clearly inferior to cardiac troponin I (cTnI) 35. However, these relationships vary depending on the nature of the procedure, the nature of the cardioplegia, and the specific assay used to measure cardiac troponin. Very high cardiac troponin values are most often associated with coronary artery-related events 35. Thus, although cardiac biomarkers and especially cardiac troponin appear robust for the detection of procedural myocardial injury and also, in the presence of new myocardial ischaemia, for the detection of type 5 myocardial infarction, a specific cut-off value for all procedures and all cardiac troponin assays is difficult to define. However, in order to ensure consistency with the analogous standards of the preceding definition of type 5 myocardial infarction 11 and because of the lack of new scientific evidence that identifies superior criteria for defining this myocardial infarction subtype, it is suggested that a cardiac troponin value > 10 times the 99th percentile upper reference limit is applied as the cut-off point during the first 48 hours following CABG, occurring from a normal baseline cardiac troponin value (≤ 99th percentile upper reference limit), for diagnosing type 5 myocardial infarction. It is important that the post-procedural elevation of cardiac troponin values is accompanied by ECG, angiographic, or imaging evidence of new myocardial ischaemia/new loss of myocardial viability.71 The higher cut-off of myocardial infarction after CABG than after PCI (10 times vs. 5 times the 99th percentile upper reference limit) has been arbitrarily selected due to the occurrence of more unavoidable myocardial injury during surgery than during PCI.
It should be recognized that ST-segment deviation and T wave changes are common after CABG due to epicardial injury, and are not reliable indicators of myocardial ischaemia in this setting. However, ST-segment elevation with reciprocal ST-segment depression or other specific ECG patterns may be a more reliable finding of a potential ischemic event 15.
What is acute myocardial infarction
Acute myocardial infarction is another term for a heart attack, which is caused by decreased coronary blood flow 36. The available oxygen supply cannot meet oxygen demand, resulting in cardiac ischemia. If blood flow isn’t restored quickly, the section of heart muscle begins to die. Decreased coronary blood flow is multifactorial. Atherosclerotic plaques classically rupture and lead to thrombosis, contributing to acute decreased blood flow in the coronary. Other etiologies of decreased oxygenation/myocardial ischemia include coronary artery embolism, which accounts for 2.9% of patients, cocaine-induced ischemia, coronary dissection, and coronary vasospasm 37.
Acute myocardial infarction is one of the leading causes of death in the developed world. The prevalence of acute myocardial infarction approaches three million people worldwide with more than one million deaths in the United States, annually 36.
What causes myocardial infarction
A myocardial infarction occurs when one or more of your coronary arteries become blocked. Over time, a coronary artery can narrow from the buildup of various substances, including cholesterol (atherosclerosis). This condition, known as coronary artery disease (coronary heart disease), causes most myocardial infarctions.
Among patients suffering from acute myocardial infarction, 70% of fatal events are due to occlusion from atherosclerotic plaques. As atherosclerosis is the predominant cause of acute myocardial infarction, risk-factors for the atherosclerotic disease are often mitigated in the prevention of disease. Modifiable risk factors account for 90% (men) and 94% (female) of myocardial infarctions. Modifiable risk factors include cigarette smoking, exercise, hypertension, obesity, cholesterol, LDL, and triglyceride levels. In contrast, age, sex, and family history are non-modifiable risk factors for atherosclerosis 38.
During a myocardial infarction, one of these plaques can rupture and spill cholesterol and other substances into the bloodstream. A blood clot forms at the site of the rupture. If large enough, the clot can block the flow of blood through the coronary artery, starving the heart muscle of oxygen and nutrients (ischemia).
You might have a complete blockage or partial. A complete blockage means you’ve had an ST elevation myocardial infarction (STEMI). A partial blockage means you’ve had a non-ST elevation myocardial infarction (NSTEMI). Diagnostic steps and treatment might be different depending on which you’ve had.
Another cause of a myocardial infarction is a spasm of a coronary artery that shuts down blood flow to part of the heart muscle. Using tobacco and illicit drugs, such as cocaine, can cause a life-threatening spasm.
Myocardial infarction risk factors
Certain factors contribute to the unwanted buildup of fatty deposits (atherosclerosis) that narrows arteries throughout your body. You can improve or eliminate many of these risk factors to reduce your chances of having a first or another myocardial infarction.
Myocardial infarction risk factors include 39:
- Age. Men age 45 or older and women age 55 or older are more likely to have a myocardial infarction than are younger men and women.
- Tobacco. This includes smoking and long-term exposure to secondhand smoke.
- High blood pressure. Over time, high blood pressure can damage arteries that feed your heart. High blood pressure that occurs with other conditions, such as obesity, high cholesterol or diabetes, increases your risk even more.
- High blood cholesterol or triglyceride levels. A high level of low-density lipoprotein (LDL) cholesterol (the “bad” cholesterol) is most likely to narrow arteries. A high level of triglycerides, a type of blood fat related to your diet, also ups your risk of myocardial infarction. However, a high level of high-density lipoprotein (HDL) cholesterol (the “good” cholesterol) lowers your risk of myocardial infarction.
- Obesity. Obesity is associated with high blood cholesterol levels, high triglyceride levels, high blood pressure and diabetes. Losing just 10 percent of your body weight can lower this risk, however.
- Diabetes. Not producing enough of a hormone secreted by your pancreas (insulin) or not responding to insulin properly causes your body’s blood sugar levels to rise, increasing your risk of myocardial infarction.
- Metabolic syndrome. This occurs when you have obesity, high blood pressure and high blood sugar. Having metabolic syndrome makes you twice as likely to develop heart disease than if you don’t have it.
- Family history of myocardial infarction. If your siblings, parents or grandparents have had early myocardial infarctions (by age 55 for male relatives and by age 65 for female relatives), you might be at increased risk.
- Lack of physical activity. Being inactive contributes to high blood cholesterol levels and obesity. People who exercise regularly have better cardiovascular fitness, including lower high blood pressure.
- Stress. You might respond to stress in ways that can increase your risk of a myocardial infarction.
Illicit drug use. Using stimulant drugs, such as cocaine or amphetamines, can trigger a spasm of your coronary arteries that can cause a myocardial infarction. - A history of preeclampsia. This condition causes high blood pressure during pregnancy and increases the lifetime risk of heart disease.
- An autoimmune condition. Having a condition such as rheumatoid arthritis or lupus can increase your risk of myocardial infarction.
INTERHEART is an international multi-center case-control study which delineated the following modifiable risk factors for coronary artery disease: The INTERHEART study 40 showed that all the above risk factors were significantly associated with acute myocardial infarction except for alcohol consumption which showed a weaker association. Smoking and abnormal apolipoprotein ratio showed the strongest association with acute myocardial infarction. The increased risk associated with diabetes and hypertension were found to be higher in women, and the protective effect of exercise and alcohol were also found to be higher in women.
Other risk factors include a moderately high level of plasma homocysteine, which is an independent risk factor of myocardial infarction. Elevated plasma homocysteine is potentially modifiable and can be treated with folic acid, vitamin B6, and vitamin B12 41.
Some non-modifiable risk factors for myocardial infarction include advanced age, male gender (males tend to have myocardial infarction earlier in life), genetics (there is an increased risk of myocardial infarction if a first-degree relative has a history of cardiovascular events before the age of 50) 42. The role of genetic loci that increase the risk for in myocardial infarction is under active investigation 43.
Myocardial infarction prevention
It’s never too late to take steps to prevent a myocardial infarction — even if you’ve already had one. Here are ways to prevent a myocardial infarction.
- Medications. Taking medications can reduce your risk of a subsequent myocardial infarction and help your damaged heart function better. Continue to take what your doctor prescribes, and ask your doctor how often you need to be monitored.
- Lifestyle factors. You know the drill: Maintain a healthy weight with a heart-healthy diet, don’t smoke, exercise regularly, manage stress and control conditions that can lead to myocardial infarction, such as high blood pressure, high cholesterol and diabetes.
Lifestyle factors
Making lifestyle changes is the most effective way to prevent having a myocardial infarction (or having another myocardial infarction).
There are three main steps you can take to help prevent a myocardial infarction (as well as stroke):
- eat a healthy, balanced diet
- avoid smoking
- try to keep your blood pressure at a healthy level
Diet
Eating an unhealthy diet high in fat will make your atherosclerosis (hardening of the arteries) worse and increase your risk of myocardial infarction.
Continuing to eat high-fat foods will cause more fatty plaques to build up in your arteries. This is because fatty foods contain cholesterol.
There are two main types of cholesterol:
- Low-density lipoprotein (LDL) often referred to as “bad cholesterol” – this is mostly made up of fat plus a small amount of protein; this type of cholesterol can block your arteries.
- High-density lipoprotein (HDL) often referred to as “good cholesterol” – this is mostly made up of protein plus a small amount of fat; this type of cholesterol can reduce deposits in your arteries.
There are also two types of fat – saturated and unsaturated. Avoid foods containing high levels of saturated fat, as they increase levels of bad cholesterol in your blood.
Foods high in saturated fat include:
- meat pies
- sausages and fatty cuts of meat
- butter
- ghee (a type of butter often used in Indian cooking)
- lard
- cream
- hard cheese
- cakes and biscuits
- foods that contain coconut or palm oil
Eating a small amount of unsaturated fat will increase the level of good cholesterol and help reduce any blockage in your arteries. Foods high in unsaturated fat include:
- oily fish
- avocados
- nuts and seeds
- sunflower, rapeseed and olive oil
Smoking
Smoking is a major risk factor for myocardial infarctions, because it causes atherosclerosis and raises blood pressure.
High blood pressure
Persistent high blood pressure can put your arteries and heart under extra strain, increasing your risk of a myocardial infarction.
High blood pressure can often be reduced by a healthy diet, moderating your intake of alcohol, maintaining a healthy weight and taking regular exercise.
Diet
The dietary advice above also applies if you have high blood pressure. In addition, cut down on the amount of salt in your food and eat plenty of fruit and vegetables.
Salt raises your blood pressure. The more salt you eat, the higher your blood pressure. You should aim to eat less than 6g (0.2oz) of salt a day, which is about a teaspoonful.
Eating a low-fat diet that includes lots of fiber – such as wholegrain rice, bread and pasta – and plenty of fruit and vegetables, has been proven to help lower blood pressure. Fruit and vegetables are full of vitamins, minerals and fiber, and help keep your body in good condition.
You should aim to eat five 80g portions of fruit and vegetables every day.
Alcohol
Regularly drinking alcohol above the recommended limits can raise your blood pressure.
- men and women are advised not to regularly drink more than 14 units a week
- spread your drinking over three days or more if you drink as much as 14 units a week
Alcohol is also high in calories, so you will gain weight if you drink regularly. Being overweight will also increase your blood pressure.
Weight
Being overweight forces your heart to work harder to pump blood around your body, which can raise your blood pressure. Find out if you need to lose weight with the BMI healthy weight calculator.
If you do need to shed some weight, it is worth remembering that losing just a few pounds will make a big difference to your blood pressure and overall health. Get tips on losing weight safely.
Exercise
Being active and taking regular exercise will lower your blood pressure by keeping your heart and blood vessels in good condition. Regular exercise can also help you lose weight, which will help lower your blood pressure.
Low-impact activities such as walking, swimming and cycling are recommended. More strenuous activities, such as playing football and squash, may not be recommended. Check with the doctor in charge of your care.
Myocardial infarction signs and symptoms
Myocardial infarction symptoms vary. Common myocardial infarction signs and symptoms include:
- Pressure, tightness, pain, or a squeezing or aching sensation in your chest or arms that may spread to your neck, jaw or back
- Nausea, indigestion, heartburn or abdominal pain
- Shortness of breath
- Cold sweat
- Fatigue
- Lightheadedness or sudden dizziness
Not all people who have myocardial infarction have the same symptoms or have the same severity of symptoms. Some people have mild pain; others have more severe pain. Some people have no symptoms; for others, the first sign may be sudden cardiac arrest. However, the more signs and symptoms you have, the greater the likelihood you’re having a myocardial infarction.
Some myocardial infarctions strike suddenly, but many people have warning signs and symptoms hours, days or weeks in advance. The earliest warning might be recurrent chest pain or pressure (angina) that’s triggered by exertion and relieved by rest. Angina is caused by a temporary decrease in blood flow to the heart.
If you see someone who’s unconscious and you believe is having a heart attack, first call for emergency medical help. Then check if the person is breathing and has a pulse. If the person isn’t breathing or you don’t find a pulse, only then should you begin CPR to keep blood flowing.
Push hard and fast on the person’s chest in a fairly rapid rhythm — about 100 to 120 compressions a minute.
If you haven’t been trained in CPR, doctors recommend performing only chest compressions. If you have been trained in CPR, you can go on to opening the airway and rescue breathing.
Myocardial infarction complications
Potential complications from a myocardial infarction can vary widely, from mild to life threatening. Some people experience a “minor” myocardial infarction (although it can still be very serious) with no associated complications. This is also known as an uncomplicated myocardial infarction.
Other people experience a major myocardial infarction, which has a wide range of potential complications and may require extensive treatment.
Complications are often related to the damage done to your heart during an attack. Some common complications of a myocardial infarction are discussed in more detail below:
- Abnormal heart rhythms (arrhythmias). Electrical “short circuits” can develop, resulting in abnormal heart rhythms, some of which can be serious, even fatal.
- Heart failure. An attack might damage so much heart tissue that the remaining heart muscle can’t pump enough blood out of your heart. Heart failure can be temporary, or it can be a chronic condition resulting from extensive and permanent damage to your heart.
- Sudden cardiac arrest. Without warning, your heart stops due to an electrical disturbance that causes an arrhythmia. myocardial infarctions increase the risk of sudden cardiac arrest, which can be fatal without immediate treatment.
Arrhythmia
An arrhythmia is an abnormal heartbeat – this includes:
- beating too quickly (tachycardia)
- beating too slowly (bradycardia)
- beating irregularly (atrial fibrillation)
Arrhythmias can develop after a myocardial infarction as a result of damage to the muscles. Damaged muscles disrupt electrical signals used by the body to control the heart.
Some arrhythmias, such as tachycardia, are mild and cause symptoms such as:
- palpitations – the sensation of your heart racing in your chest or throat
- chest pain
- dizziness or lightheadedness
- fatigue (tiredness)
- breathlessness
Other arrhythmias can be life threatening, such as:
- complete heart block, where electrical signals are unable to travel from one side of your heart to the other, so your heart cannot pump blood properly
- ventricular arrhythmia, where the heart begins beating faster before going into a spasm and stops pumping altogether; this is known as sudden cardiac arrest
These life-threatening arrhythmias can be a major cause of death during the 24-48 hours after a myocardial infarction.
However, survival rates have improved significantly since the invention of the portable defibrillator – an external device that delivers an electric shock to the heart and “resets” it to the right rhythm.
Mild arrhythmias can usually be controlled with medication such as beta-blockers.
More troublesome bradycardias that cause repeated and prolonged symptoms may need to be treated with a pacemaker. This is an electric device surgically implanted in the chest, which is used to help regulate the heartbeat.
Heart failure
Heart failure happens when your heart is unable to effectively pump blood around your body. It can develop after a myocardial infarction if your heart muscle is extensively damaged. This usually occurs in the left side of the heart (the left ventricle).
Symptoms of heart failure include:
- shortness of breath
- fatigue
- swelling in your arms and legs due to a build-up of fluid
Heart failure can be treated with a combination of medications and, in some cases, surgery.
Cardiogenic shock
Cardiogenic shock is similar to heart failure, but more serious. It develops when the heart muscle has been damaged so extensively it can no longer pump enough blood to maintain many of the body’s functions.
Cardiogenic shock symptoms include:
- mental confusion
- cold hands and feet
- decreased or no urine output
- rapid heartbeat and breathing
- pale skin
- difficulty breathing
A type of medication called vasopressors (or inotropes) may be used. Vasopressors help constrict (squeeze) the blood vessels, which increases the blood pressure and improves blood circulation.
Once the initial symptoms of cardiogenic shock have been stabilised, surgery may be required to improve the functioning of the heart. This may still include PCI, alongside the insertion of a small pump, known as an intra-aortic balloon pump. This can help improve the flow of blood away from the heart.
Another option is a coronary artery bypass graft (where a blood vessel from another part of your body is used to bypass any blockage).
Heart rupture
A heart rupture is an extremely serious but relatively uncommon complication of myocardial infarctions where the heart’s muscles, walls or valves rupture (split apart).
It can occur if the heart is significantly damaged during a myocardial infarction and usually happens 1 to 5 days afterwards.
Symptoms are the same as those of cardiogenic shock. Open heart surgery is usually required to repair the damage.
The outlook for people who have a heart rupture isn’t good, and it’s estimated that half of all people die within five days of the rupture occurring.
Myocardial infarction diagnosis
Ideally, your doctor should screen you during regular physical exams for risk factors that can lead to a myocardial infarction.
If you’re in an emergency setting for symptoms of a myocardial infarction, you’ll be asked about your symptoms and have your blood pressure, pulse and temperature checked. You’ll be hooked up to a heart monitor and have tests to see if you’re having a myocardial infarction.
Tests include:
- Electrocardiogram (ECG). This first test done to diagnose a myocardial infarction records the electrical activity of your heart via electrodes attached to your skin. Impulses are recorded as waves displayed on a monitor or printed on paper. Because injured heart muscle doesn’t conduct electrical impulses normally, the ECG may show that a myocardial infarction has occurred or is in progress.
- Blood tests. Certain heart proteins slowly leak into your blood after heart damage from a myocardial infarction. Emergency room doctors will take samples of your blood to test for the presence of these enzymes.
- Cardiac troponin-I (cTnI) and cardiac troponin-T (cTnT) are components of the contractile apparatus of myocardial cells and are expressed almost exclusively in the heart 44. Increases in cardiac troponin-I (cTnI) values have not been reported to occur following injury to non-cardiac tissues. Cardiac troponin-I (cTnI) and cardiac troponin T (cTnT) are the preferred biomarkers for the evaluation of myocardial injury 15 and high-sensitivity (hs)-cardiac troponin assays are recommended for routine clinical use 44. Other biomarkers, e.g. creatine kinase MB isoform (CK-MB), are less sensitive and less specific 45. Myocardial injury is defined as being present when blood levels of cTn are increased above the 99th percentile upper reference limit (URL) 11. The injury may be acute, as evidenced by a newly detected dynamic rising and/or falling pattern of cardiac troponin values above the 99th percentile upper reference limit (URL) or chronic, in the setting of persistently elevatedcardiac troponin levels. Although elevated cardiac troponin values reflect injury to myocardial cells, they do not indicate the underlying pathophysiological mechanisms, and can arise following preload-induced mechanical stretch or physiological stresses in otherwise normal hearts 46. Various causes have been suggested for the release of structural proteins from the myocardium, including normal turnover of myocardial cells, apoptosis, cellular release of cardiac troponin degradation products, increased cellular wall permeability, the formation and release of membranous blebs, and myocyte necrosis 47. Yet, it is not clinically possible to distinguish which increases of cTn levels are due to which mechanisms 48. However, regardless of the mechanism, acute myocardial injury, when associated with a rising and/or falling pattern of cardiac troponins values with at least one value above the 99th percentile upper reference limit and caused by myocardial ischaemia, is designated as an acute myocardial infarction 49. Histological evidence of myocardial injury with myocyte death can be detected in clinical conditions associated with non-ischaemic mechanisms of myocardial injury as well 50.
Additional tests
If you’ve had or are having a myocardial infarction, doctors will take immediate steps to treat your condition. You might also have these additional tests.
- Chest X-ray. An X-ray image of your chest allows your doctor to check the size of your heart and its blood vessels and to look for fluid in your lungs.
- Echocardiogram. Sound waves directed at your heart from a wandlike device (transducer) held on your chest bounce off your heart and are processed electronically to provide video images of your heart. An echocardiogram can help identify whether an area of your heart has been damaged and isn’t pumping normally.
- Coronary catheterization (angiogram). A liquid dye is injected into the arteries of your heart through a long, thin tube (catheter) that’s fed through an artery, usually in your leg or groin, to the arteries in your heart. The dye makes the arteries visible on X-ray, revealing areas of blockage.
- Exercise stress test. In the days or weeks after your myocardial infarction, you might also have a stress test to measure how your heart and blood vessels respond to exertion. You might walk on a treadmill or pedal a stationary bike while attached to an ECG machine. Or you might receive a drug intravenously that stimulates your heart similar to the way exercise does. Another possibility is a nuclear stress test, which is similar to an exercise stress test, but uses an injected dye and special imaging techniques to produce detailed images of your heart while you’re exercising.
- Cardiac CT or MRI. These tests can be used to diagnose heart problems, including the extent of damage from myocardial infarctions. In a cardiac CT scan, you lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest. In a cardiac MRI, you lie on a table inside a long tubelike machine that produces a magnetic field. The magnetic field aligns atomic particles in some of your cells. When radio waves are broadcast toward these aligned particles, they produce signals that vary according to the type of tissue they are. The signals create images of your heart.
The three components in the evaluation of the myocardial infarction are clinical features, ECG findings, and cardiac biomarkers.
ECG
The resting 12 lead ECG is the first-line diagnostic tool for the diagnosis of an acute coronary syndrome (ACS). It should be obtained within 10 minutes of the patient’s arrival in the emergency room 51. Acute myocardial infarction is often associated with dynamic changes in the ECG waveform. Serial ECG monitoring can provide important clues to the diagnosis if the initial EKG is non-diagnostic at initial presentation 52. Serial or continuous ECG recordings may be helpful in determining reperfusion or re-occlusion status. A large and prompt reduction in ST-segment elevation is usually seen in reperfusion 52.
ECG findings suggestive of ongoing coronary artery occlusion (in the absence of left ventricular hypertrophy and bundle branch block) 53:
ST-segment elevation in two contiguous lead (measured at J-point) of:
- Greater than 5 mm in men younger than 40 years, greater than 2 mm in men older than 40 years, or greater than 1.5 mm in women in leads V2-V3 and/or
- Greater than 1 mm in all other leads
ST-segment depression and T-wave changes:
- New horizontal or down-sloping ST-segment depression greater than 5 mm in 2 contiguous leads and/or T inversion greater than 1 mm in two contiguous leads with prominent R waves or R/S ratio of greater than 1
The hyperacute T-wave amplitude, with prominent symmetrical T waves in two contiguous leads, may be an early sign of acute myocardial infarction that may precede the ST-segment elevation. Other ECG findings associated with myocardial ischemia include cardiac arrhythmias, intraventricular blocks, atrioventricular conduction delays, and loss of precordial R-wave amplitude (less specific finding) 52.
ECG findings alone are not sufficient to diagnose acute myocardial ischemia or acute myocardial infarction as other conditions such as acute pericarditis, left ventricular hypertrophy (LVH), left bundle branch block (LBBB), Brugada syndrome, Takatsubo syndrome and early repolarization patterns also present with ST deviation.
ECG changes associated with prior myocardial infarction (in the absence of left ventricular hypertrophy and left bundle branch block):
- Any Q wave in lead V2-V3 greater than 0.02 s or QS complex in leads V2-V3
- Q wave > 03 s and greater than 1 mm deep or QS complex in leads I, II, aVL, aVF or V4-V6 in any two leads of contiguous lead grouping (I, aVL; V1-V6; II, III, aVF)
- R wave > 0.04 s in V1-V2 and R/S greater than 1 with a concordant positive T wave in the absence of conduction defect
Biomarker Detection of myocardial infarction
Cardiac troponins (I and T) are components of the contractile apparatus of myocardial cells and expressed almost exclusively in the heart. Elevated serum levels of cardiac troponin are not specific to the underlying mode of injury (ischemic vs. tension) 52. The rising and/or falling pattern of cardiac troponins (cTn) values with at least one value above the 99 percentile of upper reference limit (URL) associated with symptoms of myocardial ischemia would indicate an acute myocardial infarction. Serial testing of cTn values at 0 hours, 3 hours, and 6 hours would give a better perspective on the severity and time course of the myocardial injury. Depending on the baseline cardiac troponins value the rising/falling pattern is interpreted. If the cardiac troponins baseline value is markedly elevated, a minimum change of greater than 20% in follow up testing is significant for myocardial ischemia. Creatine kinase MB isoform can also be used in the diagnosis of myocardial infarction, but it is less sensitive and specific than cTn level 54.
Imaging
Different imaging techniques are used to assess myocardial perfusion, myocardial viability, myocardial thickness, thickening and motion, and the effect of myocyte loss on the kinetics of para-magnetic or radio-opaque contrast agents indicating myocardial fibrosis or scars 52. Some imaging modalities that can be used are echocardiography, radionuclide imaging, and cardiac magnetic resonance imaging (cardiac MRI). Regional wall motion abnormalities induced by ischemia can be detected by echocardiography almost immediately after the onset of ischemia when greater than 20% transmural myocardial thickness is affected. Cardiac MRI provides an accurate assessment of myocardial structure and function 52.
Myocardial infarction treatment
Each minute after a myocardial infarction, more heart tissue deteriorates or dies. Restoring blood flow quickly helps prevent heart damage.
The treatment options for a myocardial infarction depend on whether you’ve had an ST segment elevation myocardial infarction (STEMI), or another type of myocardial infarction.
A STEMI is the most serious form of myocardial infarction and requires emergency assessment and treatment. It’s important you’re treated quickly to minimise damage to your heart.
If you have symptoms of a myocardial infarction and an electrocardiogram (ECG) shows you have a STEMI, you’ll be assessed for treatment to unblock the coronary arteries.
The treatment used will depend on when your symptoms started and how soon you can access treatment:
- If your symptoms started within the past 12 hours – you’ll usually be offered primary percutaneous coronary intervention (PCI).
- If your symptoms started within the past 12 hours but you can’t access percutaneous coronary intervention quickly – you’ll be offered medication to break down blood clots.
- If your symptoms started more than 12 hours ago – you may be offered a different procedure, especially if symptoms have improved. The best course of treatment will be decided after an angiogram and may include medication, percutaneous coronary intervention or bypass surgery.
Medications
Medications given to treat a myocardial infarction might include:
- Aspirin. The emergency services operator might tell you to take aspirin, or emergency medical personnel might give you aspirin immediately. Aspirin reduces blood clotting, thus helping maintain blood flow through a narrowed artery.
- Thrombolytics. These drugs, also called clotbusters, help dissolve a blood clot that’s blocking blood flow to your heart. The earlier you receive a thrombolytic drug after a myocardial infarction, the greater the chance you’ll survive and have less heart damage.
- Antiplatelet agents. Emergency room doctors may give you other drugs known as platelet aggregation inhibitors to help prevent new clots and keep existing clots from getting larger.
- Other blood-thinning medications. You’ll likely be given other medications, such as heparin, to make your blood less “sticky” and less likely to form clots. Heparin is given intravenously or by an injection under your skin.
- Pain relievers. You might be given a pain reliever, such as morphine.
- Nitroglycerin. This medication, used to treat chest pain (angina), can help improve blood flow to the heart by widening (dilating) the blood vessels.
- Beta blockers. These medications help relax your heart muscle, slow your heartbeat and decrease blood pressure, making your heart’s job easier. Beta blockers can limit the amount of heart muscle damage and prevent future myocardial infarctions.
- ACE inhibitors. These drugs lower blood pressure and reduce stress on the heart.
- Statins. These drugs help control your blood cholesterol.
Thrombolytics
Medications used to break down blood clots, known as thrombolytics or fibrinolytics, are usually given by injection.
Thrombolytics or fibrinolytics, target and destroy a substance called fibrin. Fibrin is a tough protein that makes up blood clots by acting like a sort of fibre mesh that hardens around the blood.
Some examples of thrombolytics include:
- reteplase
- alteplase
- streptokinase
You may also be given an additional medication called a glycoprotein IIb/IIIa inhibitor if it is thought you have an increased risk of experiencing another myocardial infarction at some point in the near future.
Glycoprotein IIb/IIIa inhibitors don’t break up blood clots, but they prevent blood clots from getting bigger. They’re an effective method of stopping your symptoms getting worse.
Surgical and other procedures
In addition to medications, you might have one of these procedures to treat your myocardial infarction:
- Coronary angioplasty and stenting. In this procedure, also known as percutaneous coronary intervention (PCI), doctors insert a long, thin tube (catheter) that’s passed through an artery in your groin or wrist to a blocked artery in your heart. If you’ve had a myocardial infarction, this procedure is often done immediately after a cardiac catheterization, a procedure used to find blockages. This catheter has a special balloon that, once in position, is briefly inflated to open a blocked coronary artery. A metal mesh stent might then be inserted into the artery to keep it open long term, restoring blood flow to the heart. Depending on your condition, you might get a stent coated with a slow-releasing medication to help keep your artery open.
- Coronary artery bypass surgery also known as a coronary artery bypass graft (CABG). In some cases, doctors perform emergency bypass surgery at the time of a myocardial infarction. If possible, however, you might have bypass surgery after your heart has had time — about three to seven days — to recover from your myocardial infarction. Bypass surgery involves sewing veins or arteries in place beyond a blocked or narrowed coronary artery, allowing blood flow to the heart to bypass the narrowed section. Once blood flow to your heart is restored and your condition is stable, you’re likely to remain in the hospital for several days.
Percutaneous coronary intervention
Primary percutaneous coronary intervention (PCI) or coronary angioplasty and stenting, is the term for emergency treatment of ST segment elevation myocardial infarction (STEMI), using a procedure to widen the coronary artery (coronary angioplasty).
Coronary angiography is performed first to assess your suitability for percutaneous coronary intervention (PCI).
You may also be given blood-thinning medication to prevent further clots from developing, such as:
- aspirin
- heparin
- clopidogrel
- prasugrel
- ticagrelor
- bivalirudin
Some of these medications may be continued for some time after percutaneous coronary intervention (PCI).
Coronary angioplasty
Coronary angioplasty is a potentially complex type of procedure that requires specialist staff and equipment, and not all hospitals have the facilities.
This means you’ll need to be taken urgently, by ambulance, to one of the specialist centers (myocardial infarction centers) that now serve most of the US’s regions.
During coronary angioplasty, a tiny tube known as a balloon catheter, with a sausage-shaped balloon at the end, is put into a large artery in your groin or arm. The catheter is passed through your blood vessels and up to your heart, over a fine guide wire, using X-rays to guide it, before being moved into the narrowed section of your coronary artery.
Once in position, the balloon is inflated inside the narrowed part of the coronary artery to open it wide. A stent (flexible metal mesh) is usually inserted into the artery to help keep it open afterwards.
Coronary artery bypass graft
A coronary angioplasty may not be technically possible sometimes if the anatomy of your arteries is different from normal. This may be the case if there are too many narrow sections in your arteries or if there are lots of branches coming off your arteries that are also blocked.
In such circumstances, an alternative surgical operation, known as a coronary artery bypass graft (CABG), may be considered. A CABG involves taking a blood vessel from another part of your body, usually your chest or leg, to use as a graft.
The graft bypasses any hardened or narrowed arteries in the heart. A surgeon will attach the new blood vessel to the aorta and the other to the coronary artery beyond the narrowed area or blockage.
Treating non-ST segment elevation myocardial infarction (NSTEMI) or unstable angina
If the results of your ECG show you have a “less serious” type of heart attack (known as a non-ST segment elevation myocardial infarction (NSTEMI) or unstable angina), then blood-thinning medication, including aspirin and other medications, is usually recommended.
In some cases, further treatment with coronary angioplasty or coronary artery bypass graft may be recommended in cases of NSTEMI or unstable angina, after initial treatment with these medications.
Myocardial infarction recovery
Recovering from a myocardial infarction can take several months, and it’s very important not to rush your rehabilitation.
During your recovery period, you’ll receive help and support from a range of healthcare professionals, which may include:
- nurses
- physiotherapists
- dietitians
- pharmacists
- exercise specialists
These healthcare professionals will support you physically and mentally to ensure your recovery is conducted safely and appropriately.
The recovery process usually takes place in stages, starting in hospital, where your condition can be closely monitored and your individual needs for the future can be assessed.
After being discharged, you can continue your recovery at home.
The 2 most important aims of the recovery process are:
- to gradually restore your physical fitness so you can resume normal activities (known as cardiac rehabilitation)
- to reduce your risk of another myocardial infarction
Cardiac rehabilitation
Your cardiac rehabilitation program will begin when you’re in hospital. Most hospitals offer programs that might start while you’re in the hospital and continue for weeks to a couple of months after you return home. Cardiac rehabilitation programs generally focus on four main areas:
- medications,
- lifestyle changes,
- emotional issues and
- a gradual return to your normal activities.
It’s extremely important to participate in this program. People who attend cardiac rehab after a myocardial infarction generally live longer and are less likely to have another myocardial infarction or complications from the myocardial infarction. If cardiac rehab is not recommended during your hospitalization, ask your doctor about it.
You should also be invited back for another session taking place within 10 days of leaving hospital.
A member of the cardiac rehabilitation team will visit you in hospital and provide detailed information about:
- your state of health and how the heart attack may have affected it
- the type of treatment you received
- what medications you’ll need when you leave hospital
- what specific risk factors are thought to have contributed to your heart attack
- what lifestyle changes you can make to address those risk factors
They can also answer any questions you have about finance, welfare rights, housing and social care.
Cardiac rehabilitation medications
There are currently 4 types of medication widely used to reduce the risk of a myocardial infarction:
- angiotensin-converting enzyme (ACE) inhibitors
- anti-platelets
- beta blockers
- statins
ACE inhibitors
ACE inhibitors are often used to lower blood pressure, as they block the actions of some of the hormones that help regulate blood pressure.
By stopping these hormones working, the medicine helps to reduce the amount of water in your blood and also widens your arteries, both of which will reduce your blood pressure.
ACE inhibitors have been known to reduce the supply of blood to the kidneys, which can reduce their efficiency.
This means blood and urine tests may be carried out before you start taking ACE inhibitors to make sure there are no pre-existing problems with your kidneys.
Annual blood and urine tests may be required if you continue to use ACE inhibitors.
The side effects of ACE inhibitors can include:
- dizziness
- tiredness or weakness
- headaches
- a persistent, dry cough
Most of these should pass within a few days, although some people continue to have a dry cough.
If ACE inhibitors are taken with other forms of medication, including over-the-counter medicines, they can cause unpredictable effects.
Check with your doctor or pharmacist before taking anything in combination with ACE inhibitors.
It’s usually recommended that you begin taking ACE inhibitors immediately after having a myocardial infarction and, in most cases, continue taking them indefinitely.
In some individuals who prove intolerant of ACE inhibitors, a related alternative medication (an angiotensin receptor blocker, or ARB) may be prescribed.
Anti-platelets
Anti-platelets are a type of medication that can help prevent blood clots.
They work by reducing the “stickiness” of platelets, which are tiny particles in the blood that help it to clot.
It’s usually recommended that you take low-dose aspirin, which has blood-thinning properties, as well as being a painkiller.
You’re more likely to be given additional anti-platelet medication, such as clopidogrel, prasugrel or ticagrelor, especially if you have had stent treatment.
These can also be used if you’re allergic to aspirin.
Side effects can include:
- diarrhea
- bruising or bleeding
- breathlessness
- abdominal pain
- indigestion
- heartburn
As with ACE inhibitors, treatment with anti-platelets usually begins immediately after a myocardial infarction.
The amount of time for which you’re prescribed these medications can be anywhere between 4 weeks and 12 months, and depends on the type of myocardial infarction you have had and the other treatment you have received.
It’s usually recommended that you take aspirin indefinitely.
If you experience troublesome side effects from aspirin, you should contact your doctor for advice.
Don’t suddenly stop taking the aspirin, as this could increase your risk of another myocardial infarction.
You may occasionally also be put on another blood-thinning medication, called warfarin.
This usually only happens if you have remained in an irregular heart rhythm (atrial fibrillation) or sustained severe damage to your heart.
Excessive bleeding is the most serious side effect of warfarin.
Seek immediate medical attention and have an urgent blood test if you experience any of the following side effects:
- passing blood in your pee or poo
- passing black poo
- severe bruising
- prolonged nosebleeds that last longer than 10 minutes
- blood in your vomit
- coughing up blood
- unusual headaches
- heavy or increased bleeding during your period or any other bleeding from the vagina
Immediate medical attention must also be sought if you:
- are involved in major trauma (an accident)
- experience a significant blow to the head
- are unable to stop any bleeding
Beta blockers
Beta blockers are a type of medication used to protect the heart from further damage after a myocardial infarction.
They help to relax the heart’s muscles so the heart beats slower and blood pressure drops, both of which will reduce the strain on your heart.
It’s usually recommended that you begin treatment with beta blockers as soon as your condition stabilizes, and continue taking them indefinitely.
Fairly common side effects of beta blockers include:
- tiredness
- cold hands and feet
- a slow heartbeat
- diarrhea
- feeling sick
Less common side effects include:
- sleep disturbances
- nightmares
- inability to obtain or maintain an erection (erectile dysfunction, or impotence)
Beta blockers can also interact with other medicines, causing possible adverse side effects.
Check with your doctor or pharmacist before taking other medicines, including over-the-counter medication, in combination with beta blockers.
Statins
Statins are a type of medication used to lower your blood cholesterol level.
This will help prevent further damage to your coronary arteries and should reduce the risk of another myocardial infarction.
Statins block the effects of an enzyme in your liver called HMG-CoA reductase, which is used to make cholesterol.
Statins sometimes have mild side effects, including:
- constipation
- diarrhea
- headaches
- abdominal pain
Occasionally, statins can cause muscle pain, weakness and tenderness.
Contact your doctor if you experience these symptoms, as your dosage may need to be adjusted.
It’s usually recommended that you take statins indefinitely.
Lifestyle and home remedies
To improve your heart health, take the following steps:
- Avoid smoke. The most important thing you can do to improve your heart’s health is to not smoke. Also, avoid being around secondhand smoke. If you need to quit, ask your doctor for help.
- Control your blood pressure and cholesterol levels. If one or both of these is high, your doctor can prescribe changes to your diet and medications. Ask your doctor how often you need to have your blood pressure and cholesterol levels monitored.
- Get regular medical checkups. Some of the major risk factors for myocardial infarction — high blood cholesterol, high blood pressure and diabetes — cause no symptoms early on. Your doctor can test for these conditions and can help you manage them, if necessary.
- Exercise. Regular exercise helps improve heart muscle function after a myocardial infarction and helps prevent a myocardial infarction. Walking 30 minutes a day, five days a week can improve your health.
- Maintain a healthy weight. Excess weight strains your heart and can contribute to high cholesterol, high blood pressure and diabetes.
- Eat a heart-healthy diet. Saturated fat, trans fats and cholesterol in your diet can narrow arteries to your heart, and too much salt can raise blood pressure. Eat a heart-healthy diet that includes lean proteins, such as fish and beans, and fruits and vegetables and whole grains.
- Manage diabetes. Regular exercise, eating well and losing weight all help to keep blood sugar levels at more-desirable levels. Many people also need medication to manage their diabetes.
- Control stress. Reduce stress in your day-to-day activities. Rethink workaholic habits and find healthy ways to minimize or deal with stressful events in your life.
- If you drink alcohol, do so in moderation. That means up to one drink a day for women and men older than age 65, and up to two drinks a day for men age 65 and younger.
Exercise
Once you return home, it’s usually recommended that you rest and only do light activities, such as walking up and down the stairs a few times a day or taking a short walk.
Gradually increase the amount of activity you do each day over several weeks. How quickly you can do this will depend on the condition of your heart and your general health.
Your care team can provide more detailed advice about a recommended plan to increase your activity levels.
Your rehabilitation program should contain a range of different exercises, depending on your age and ability.
Most of the exercises will be aerobic. These are designed to strengthen the heart, improve circulation and lower blood pressure.
Examples of aerobic exercises include riding an exercise bike, jogging on a treadmill and swimming.
Regular physical activity
Once you have made a sufficient physical recovery from the effects of a heart attack, it’s recommended that you do regular physical activity.
Adults should do at least 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity such as cycling or fast walking every week.
The level of activity should be strenuous enough to leave you slightly breathless.
If you find it difficult to achieve 150 minutes of activity a week, start at a level that you feel comfortable with (for example, 5 to 10 minutes of light exercise a day) and gradually increase the duration and intensity of your activity as your fitness begins to improve.
Returning to work
Most people can return to work after having a myocardial infarction, but how quickly will depend on your health, the state of your heart and the kind of work you do.
If your job involves light duties, such as if you work in an office, you may be able to return to work in as little as 2 weeks.
But if your job involves heavy manual work or your heart was extensively damaged, it may be several months before you can return to work.
Your care team will provide a more detailed prediction of how long it’ll take for you to return to work.
Sex after a myocardial infarction
Some people worry about having sex after a myocardial infarction, but most people can safely return to sexual activity after recovery. When you can resume sexual activity will depend on your physical comfort, psychological readiness and previous sexual activity. Ask your doctor when it’s safe to have sex.
According to the British Heart Foundation, you’re usually able to start having sex again once you feel well enough, usually about 4 to 6 weeks after having a myocardial infarction.
Having sex won’t put you at further risk of having another myocardial infarction.
Following a myocardial infarction, about 1 in 3 men have erectile dysfunction, which may make having sex difficult.
This is most commonly due to anxiety and the emotional stress associated with having a myocardial infarction.
Less commonly, erectile dysfunction is a side effect of beta blockers.
If you experience erectile dysfunction, speak to your doctor. They may be able to recommend treatment.
For example, you may be prescribed medication that stimulates the flow of blood to your penis, which makes it easier to get an erection.
Some heart medications can affect sexual function. If you’re having problems with sexual dysfunction, talk to your doctor.
Driving
If you drive a car or motorcycle and you have a myocardial infarction, you don’t have to inform the Driver and Vehicle Licensing Agency (DMV).
Many people can now return to driving 1 week after a myocardial infarction, as long you don’t have any other condition or complication that would disqualify you from driving.
But in more severe cases, you may need to stop driving for 4 weeks.
Your doctor or rehabilitation team should advise how long you must wait before driving after your myocardial infarction.
If you drive a large goods vehicle or passenger-carrying vehicle, you must inform the DMV if you have a myocardial infarction.
Your licence will be temporarily suspended, for a minimum of 6 weeks, until you have adequately recovered.
Your licence will be reissued if you can pass a basic health and fitness test, and don’t have any other condition that would disqualify you from driving.
Depression
Having a myocardial infarction can be frightening and traumatic, and it’s common to have feelings of anxiety afterwards.
For many people, the emotional stresses can cause them to feel depressed and tearful for the first few weeks after returning home from hospital.
If feelings of depression persist, speak to your doctor as you may have a more serious form of depression.
It’s important to seek advice as serious types of depression often don’t get better without treatment.
Your emotional state could also have an adverse effect on your physical recovery.
Reducing your risk for another myocardial infarction
Reducing your risk of having another myocardial infarction involves making lifestyle changes and taking a long-term course of different medications.
Diet
Making changes to your diet can help reduce your risk of having another myocardial infarction.
Other lifestyle changes, such as drinking less alcohol, taking regular exercise, giving up smoking (if you smoke) and maintaining a healthy weight can also help.
You should aim to follow a Mediterranean-style diet. This means eating more bread, fruit, vegetables and fish, and less meat.
Replace butter and cheese with products based on vegetable and plant oil, such as olive oil.
Oily fish, like herring, sardines and salmon, can form part of a Mediterranean-style diet, but there’s no need to eat this type of fish specifically to try to prevent another myocardial infarction.
Also, omega-3 fatty acid capsules or foods fortified with omega-3 fatty acids haven’t been found to help prevent another myocardial infarction.
Never take a food supplement without first consulting your doctor. Some supplements, such as beta-carotene, are potentially harmful.
Mediterranean diet
There’s evidence to show that eating a Mediterranean-style diet can reduce your risk of having another myocardial infarction.
To make your diet more Mediterranean you can:
- eat more fruit, salad and vegetables
- eat more wholegrains, nuts and seeds
- eat more fish
- eat less meat
- choose products made from vegetable and plant oils, such as olive oil, rather than dairy products, such as butter and cheese
Oily fish
You should eat at least 2 portions of fish a week, including a portion of oily fish.
Oily fish is a rich source of omega-3 fatty acids, which help prevent heart disease.
Examples of oily fish include:
- herring
- sardines
- mackerel
- salmon
- trout
One portion is about 140g, which is equivalent to a small tin of oily fish or a small fillet of fresh fish.
Healthier ways to cook
Don’t fry or roast food in fat. Instead, prepare and cook your food using healthy methods such as:
- steaming
- poaching
- baking
- stir-frying
- making a casserole
- using the microwave
Buttery, cheesy or creamy sauces tend to be high in fat. Instead, try adding flavour to your sauces using spices, herbs and lemon juice.
Foods to avoid
Avoid foods that are high in:
- saturated fat (this is the current guidance, although further studies on saturated fat are needed)
- salt
- sugar
Foods containing high amounts of fat, salt or sugar include:
- fried foods
- sweets and confectionery
- takeaways
- processed foods
- pre-packaged foods
Supplements to avoid
Don’t take beta-carotene supplements (beta-carotene is a type of vitamin A). Research has shown that taking these supplements may increase your risk of having another myocardial infarction.
Also, taking vitamin C, vitamin E or folic acid supplements won’t help prevent another myocardial infarction. There’s no evidence to suggest that taking any of these supplements will have any benefit.
References- Akbar H, Foth C, Kahloon RA, et al. Acute ST Elevation Myocardial Infarction. [Updated 2020 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532281
- Myocardial infarction redefined–a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J. 2000 Sep;21(18):1502-13. doi: 10.1053/euhj.2000.2305
- Thygesen K, Alpert JS, White HD, Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Circulation. 2007 Nov 27;116(22):2634-53.
- Reimer KA, Jennings RB, Tatum AH. Pathobiology of acute myocardial ischemia: metabolic, functional and ultrastructural studies. Am. J. Cardiol. 1983 Jul 20;52(2):72A-81A
- Apple FS, Sandoval Y, Jaffe AS, Ordonez-Llanos J., IFCC Task Force on Clinical Applications of Cardiac Bio-Markers. Cardiac Troponin Assays: Guide to Understanding Analytical Characteristics and Their Impact on Clinical Care. Clin. Chem. 2017 Jan;63(1):73-81
- Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, Zheng ZJ, Flegal K, O’Donnell C, Kittner S, Lloyd-Jones D, Goff DC, Hong Y, Adams R, Friday G, Furie K, Gorelick P, Kissela B, Marler J, Meigs J, Roger V, Sidney S, Sorlie P, Steinberger J, Wasserthiel-Smoller S, Wilson M, Wolf P., American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006 Feb 14;113(6):e85-151
- Ojha N, Dhamoon AS. Myocardial Infarction. [Updated 2019 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537076
- Benjamin EJ et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018 Mar 20;137(12):e67-e492
- Mendis S, Thygesen K, Kuulasmaa K, Giampaoli S, Mähönen M, Ngu Blackett K, Lisheng L; Writing group on behalf of the participating experts of the WHO consultation for revision of WHO definition of myocardial infarction. World Health Organization definition of myocardial infarction: 2008-09 revision. Int J Epidemiol. 2011 Feb;40(1):139-46. doi: 10.1093/ije/dyq165
- Apple FS, Murakami MM. Cardiac troponin and creatine kinase MB monitoring during in-hospital myocardial reinfarction. Clin Chem. 2005 Feb;51(2):460-3. doi: 10.1373/clinchem.2004.042887
- Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD; Writing Group on the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction, Thygesen K, Alpert JS, White HD, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman BA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasché P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S; ESC Committee for Practice Guidelines (CPG). Third universal definition of myocardial infarction. Eur Heart J. 2012 Oct;33(20):2551-67. doi: 10.1093/eurheartj/ehs184
- Tau S Hartikainen, Nils Arne Sörensen, Paul Michael Haller, Alina Goßling, Jonas Lehmacher, Tanja Zeller, Stefan Blankenberg, Dirk Westermann, Johannes Tobias Neumann, Clinical application of the 4th Universal Definition of Myocardial Infarction, European Heart Journal, Volume 41, Issue 23, 14 June 2020, Pages 2209–2216, https://doi.org/10.1093/eurheartj/ehaa035
- Basit H, Malik A, Huecker MR. Non ST Segment Elevation Myocardial Infarction. [Updated 2021 Jul 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513228
- Nascimento BR, Brant LCC, Marino BCA, Passaglia LG, Ribeiro ALP. Implementing myocardial infarction systems of care in low/middle-income countries. Heart. 2019 Jan;105(1):20-26.
- Kristian Thygesen, Joseph S Alpert, Allan S Jaffe, Bernard R Chaitman, Jeroen J Bax, David A Morrow, Harvey D White, ESC Scientific Document Group, Fourth universal definition of myocardial infarction (2018), European Heart Journal, Volume 40, Issue 3, 14 January 2019, Pages 237–269, https://doi.org/10.1093/eurheartj/ehy462
- Garcia-Garcia HM, McFadden EP, Farb A, Mehran R, Stone GW, Spertus J, Onuma Y, Morel MA, van Es GA, Zuckerman B, Fearon WF, Taggart D, Kappetein AP, Krucoff MW, Vranckx P, Windecker S, Cutlip D, Serruys PW; Academic Research Consortium. Standardized End Point Definitions for Coronary Intervention Trials: The Academic Research Consortium-2 Consensus Document. Eur Heart J. 2018 Jun 14;39(23):2192-2207. doi: 10.1093/eurheartj/ehy223
- Kamińska, J., Koper, O. M., Siedlecka-Czykier, E., Matowicka-Karna, J., Bychowski, J., & Kemona, H. (2018). The utility of inflammation and platelet biomarkers in patients with acute coronary syndromes. Saudi journal of biological sciences, 25(7), 1263–1271. https://doi.org/10.1016/j.sjbs.2016.10.015
- Rupprecht HJ, Geeren M, Geeren M, Weilemann S, Schuster HP. Akutes Koronarsyndrom ohne ST-Hebung (NSTE-ACS) [Acute coronary syndrome without ST-elevation (NSTE-ACS)]. Herz. 2019 Feb;44(1):10-15. German. doi: 10.1007/s00059-018-4776-1
- Sriha Belguith, A., Beltaief, K., Msolli, M. A., Bouida, W., Abroug, H., Ben Fredj, M., Zemni, I., Grissa, M. H., Boubaker, H., ESCor Investigators group, Hsairi, M., Nouira, S., & ESCorT Investigators group (2018). Management of acute coronary syndrome in emergency departments: a cross sectional multicenter study (Tunisia). BMC emergency medicine, 18(1), 50. https://doi.org/10.1186/s12873-018-0201-6
- Lemkes JS, Janssens GN, van der Hoeven NW, van de Ven PM, Marques KMJ, Nap A, van Leeuwen MAH, Appelman YEA, Knaapen P, Verouden NJW, Allaart CP, Brinckman SL, Saraber CE, Plomp KJ, Timmer JR, Kedhi E, Hermanides RS, Meuwissen M, Schaap J, van der Weerdt AP, van Rossum AC, Nijveldt R, van Royen N. Timing of revascularization in patients with transient ST-segment elevation myocardial infarction: a randomized clinical trial. Eur Heart J. 2019 Jan 14;40(3):283-291. doi: 10.1093/eurheartj/ehy651
- Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined–a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000 Sep;36(3):959-69. doi: 10.1016/s0735-1097(00)00804-4. Erratum in: J Am Coll Cardiol 2001 Mar 1;37(3):973.
- Canto, J. G., Kiefe, C. I., Rogers, W. J., Peterson, E. D., Frederick, P. D., French, W. J., Gibson, C. M., Pollack, C. V., Jr, Ornato, J. P., Zalenski, R. J., Penney, J., Tiefenbrunn, A. J., Greenland, P., & NRMI Investigators (2011). Number of coronary heart disease risk factors and mortality in patients with first myocardial infarction. JAMA, 306(19), 2120–2127. https://doi.org/10.1001/jama.2011.1654
- Bentzon JF, Otsuka F, Virmani R, Falk E. Mechanisms of plaque formation and rupture. Circ Res. 2014 Jun 6;114(12):1852-66. doi: 10.1161/CIRCRESAHA.114.302721
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018 Jan 7;39(2):119-177. doi: 10.1093/eurheartj/ehx393
- Cediel G, Gonzalez-Del-Hoyo M, Carrasquer A, Sanchez R, Boqué C, Bardají A. Outcomes with type 2 myocardial infarction compared with non-ischaemic myocardial injury. Heart. 2017 Apr;103(8):616-622. doi: 10.1136/heartjnl-2016-310243
- Chapman AR, Shah ASV, Lee KK, Anand A, Francis O, Adamson P, McAllister DA, Strachan FE, Newby DE, Mills NL. Long-Term Outcomes in Patients With Type 2 Myocardial Infarction and Myocardial Injury. Circulation. 2018 Mar 20;137(12):1236-1245. doi: 10.1161/CIRCULATIONAHA.117.031806
- Lambrecht S, Sarkisian L, Saaby L, Poulsen TS, Gerke O, Hosbond S, Diederichsen ACP, Thygesen K, Mickley H. Different Causes of Death in Patients with Myocardial Infarction Type 1, Type 2, and Myocardial Injury. Am J Med. 2018 May;131(5):548-554. doi: 10.1016/j.amjmed.2017.11.043
- Sandoval Y, Thygesen K. Myocardial Infarction Type 2 and Myocardial Injury. Clin Chem. 2017 Jan;63(1):101-107. doi: 10.1373/clinchem.2016.255521
- Saw J, Mancini GBJ, Humphries KH. Contemporary Review on Spontaneous Coronary Artery Dissection. J Am Coll Cardiol. 2016 Jul 19;68(3):297-312. doi: 10.1016/j.jacc.2016.05.034. Erratum in: J Am Coll Cardiol. 2016 Oct 4;68(14):1606
- Jangaard N , Sarkisian L, Saaby L, Mikkelsen S, Lassen AM, Marcussen N, Thomsen JL, Diederichsen A, Thygesen K, Mickley H. Incidence, frequency and clinical characteristics of type 3 myocardial infarction in clinical practice. Am J Med2017;130:862.e9–862.e14.
- Zeitouni M, Silvain J, Guedeney P, Kerneis M, Yan Y, Overtchouk P, Barthelemy O, Hauguel-Moreau M, Choussat R, Helft G, Le Feuvre C, Collet JP, Montalescot G; ACTION Study Group. Periprocedural myocardial infarction and injury in elective coronary stenting. Eur Heart J. 2018 Apr 1;39(13):1100-1109. doi: 10.1093/eurheartj/ehx799
- Jørgensen PH, Nybo M, Jensen MK, Mortensen PE, Poulsen TS, Diederichsen AC, Mickley H. Optimal cut-off value for cardiac troponin I in ruling out Type 5 myocardial infarction. Interact Cardiovasc Thorac Surg. 2014 May;18(5):544-50. doi: 10.1093/icvts/ivt558
- Rahimi K, Banning AP, Cheng AS, Pegg TJ, Karamitsos TD, Channon KM, Darby S, Taggart DP, Neubauer S, Selvanayagam JB. Prognostic value of coronary revascularisation-related myocardial injury: a cardiac magnetic resonance imaging study. Heart. 2009 Dec;95(23):1937-43. doi: 10.1136/hrt.2009.173302
- Thielmann M, Sharma V, Al-Attar N, Bulluck H, Bisleri G, Bunge JJH, Czerny M, Ferdinandy P, Frey UH, Heusch G, Holfeld J, Kleinbongard P, Kunst G, Lang I, Lentini S, Madonna R, Meybohm P, Muneretto C, Obadia JF, Perrino C, Prunier F, Sluijter JPG, Van Laake LW, Sousa-Uva M, Hausenloy DJ. ESC Joint Working Groups on Cardiovascular Surgery and the Cellular Biology of the Heart Position Paper: Perioperative myocardial injury and infarction in patients undergoing coronary artery bypass graft surgery. Eur Heart J. 2017 Aug 14;38(31):2392-2407. doi: 10.1093/eurheartj/ehx383
- Pegg TJ, Maunsell Z, Karamitsos TD, Taylor RP, James T, Francis JM, Taggart DP, White H, Neubauer S, Selvanayagam JB. Utility of cardiac biomarkers for the diagnosis of type V myocardial infarction after coronary artery bypass grafting: insights from serial cardiac MRI. Heart. 2011 May;97(10):810-6. doi: 10.1136/hrt.2010.213462
- Mechanic OJ, Grossman SA. Acute Myocardial Infarction. [Updated 2019 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459269
- Massberg S, Polzin A. [Update ESC-Guideline 2017: Dual Antiplatelet Therapy]. Dtsch. Med. Wochenschr. 2018 Aug;143(15):1090-1093.
- Berg DD, Wiviott SD, Braunwald E, Guo J, Im K, Kashani A, Gibson CM, Cannon CP, Morrow DA, Bhatt DL, Mega JL, O’Donoghue ML, Antman EM, Newby LK, Sabatine MS, Giugliano RP. Modes and timing of death in 66 252 patients with non-ST-segment elevation acute coronary syndromes enrolled in 14 TIMI trials. Eur. Heart J. 2018 Nov 07;39(42):3810-3820.
- Anand SS, Islam S, Rosengren A, Franzosi MG, Steyn K, Yusufali AH, Keltai M, Diaz R, Rangarajan S, Yusuf S., INTERHEART Investigators. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur. Heart J. 2008 Apr;29(7):932-40.
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L., INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004 Sep 11-17;364(9438):937-52.
- Stampfer MJ, Malinow MR, Willett WC, Newcomer LM, Upson B, Ullmann D, Tishler PV, Hennekens CH. A prospective study of plasma homocyst(e)ine and risk of myocardial infarction in US physicians. JAMA. 1992 Aug 19;268(7):877-81
- Nielsen M, Andersson C, Gerds TA, Andersen PK, Jensen TB, Køber L, Gislason G, Torp-Pedersen C. Familial clustering of myocardial infarction in first-degree relatives: a nationwide study. Eur. Heart J. 2013 Apr;34(16):1198-203
- Samani NJ, Burton P, Mangino M, Ball SG, Balmforth AJ, Barrett J, Bishop T, Hall A., BHF Family Heart Study Research Group. A genomewide linkage study of 1,933 families affected by premature coronary artery disease: The British Heart Foundation (BHF) Family Heart Study. Am. J. Hum. Genet. 2005 Dec;77(6):1011-20.
- Thygesen K, Mair J, Giannitsis E, Mueller C, Lindahl B, Blankenberg S, Huber K, Plebani M, Biasucci LM, Tubaro M, Collinson P, Venge P, Hasin Y, Galvani M, Koenig W, Hamm C, Alpert JS, Katus H, Jaffe AS; Study Group on Biomarkers in Cardiology of ESC Working Group on Acute Cardiac Care. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J. 2012 Sep;33(18):2252-7. doi: 10.1093/eurheartj/ehs154
- Goodman SG, Steg PG, Eagle KA, Fox KA, López-Sendón J, Montalescot G, Budaj A, Kennelly BM, Gore JM, Allegrone J, Granger CB, Gurfinkel EP; GRACE Investigators. The diagnostic and prognostic impact of the redefinition of acute myocardial infarction: lessons from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2006 Mar;151(3):654-60. doi: 10.1016/j.ahj.2005.05.014
- Weil BR , Suzuki G, Young RF, Iyer V, Canty JMJr. Troponin release and reversible left ventricular dysfunction following transient pressure overload: Stress-induced myocardial stunning. J Am Cardiol Coll2018;71:2906–2916.
- Mair J, Lindahl B, Hammarsten O, Müller C, Giannitsis E, Huber K, Möckel M, Plebani M, Thygesen K, Jaffe AS; European Society of Cardiology (ESC) Study Group on Biomarkers in Cardiology of the Acute Cardiovascular Care Association (ACCA). How is cardiac troponin released from injured myocardium?Eur Heart J Acute Cardiovasc Care; doi: 10.1177/2048872617748553
- Jaffe AS, Wu AH. Troponin release–reversible or irreversible injury? Should we care? Clin Chem. 2012 Jan;58(1):148-50. doi: 10.1373/clinchem.2011.173070. Epub 2011 Oct 28. Erratum in: Clin Chem. 2012 Apr;58(4):796.
- Apple FS, Jaffe AS, Collinson P, Mockel M, Ordonez-Llanos J, Lindahl B, Hollander J, Plebani M, Than M, Chan MH; International Federation of Clinical Chemistry (IFCC) Task Force on Clinical Applications of Cardiac Bio-Markers. IFCC educational materials on selected analytical and clinical applications of high sensitivity cardiac troponin assays. Clin Biochem. 2015 Mar;48(4-5):201-3. doi: 10.1016/j.clinbiochem.2014.08.021
- Eggers KM, Lindahl B. Application of Cardiac Troponin in Cardiovascular Diseases Other Than Acute Coronary Syndrome. Clin Chem. 2017 Jan;63(1):223-235. doi: 10.1373/clinchem.2016.261495
- Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF, Windecker S., ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2016 Jan 14;37(3):267-315.
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, Mickley H, Crea F, Van de Werf F, Bucciarelli-Ducci C, Katus HA, Pinto FJ, Antman EM, Hamm CW, De Caterina R, Januzzi JL, Apple FS, Alonso Garcia MA, Underwood SR, Canty JM, Lyon AR, Devereaux PJ, Zamorano JL, Lindahl B, Weintraub WS, Newby LK, Virmani R, Vranckx P, Cutlip D, Gibbons RJ, Smith SC, Atar D, Luepker RV, Robertson RM, Bonow RO, Steg PG, O’Gara PT, Fox KAA. [Fourth universal definition of myocardial infarction (2018)]. Kardiol Pol. 2018;76(10):1383-1415.
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P., ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018 Jan 07;39(2):119-177
- Thygesen K, Mair J, Giannitsis E, Mueller C, Lindahl B, Blankenberg S, Huber K, Plebani M, Biasucci LM, Tubaro M, Collinson P, Venge P, Hasin Y, Galvani M, Koenig W, Hamm C, Alpert JS, Katus H, Jaffe AS., Study Group on Biomarkers in Cardiology of ESC Working Group on Acute Cardiac Care. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur. Heart J. 2012 Sep;33(18):2252-7.