Myopericarditis
Myopericarditis is a primarily pericardial inflammatory syndrome occurring when clinical diagnostic criteria for pericarditis are satisfied and concurrent mild myocardial involvement is documented by elevation of biomarkers of myocardial damage (i.e., increased troponins) 1. Sometimes myopericarditis is used interchangeably with perimyocarditis 2. Myopericarditis is used when there are primarily pericarditis symptoms with evidence of the involvement of the myocardium as evidenced by cardiac biomarker elevation or imaging studies revealing normal wall motion 3. If there is evidence of regional wall motion abnormalities with reduced ventricular function, the term perimyocarditis has been used 2.
Limited clinical data on the causes of myopericarditis suggest that viral infections are among the most common causes in developed countries 1. Cardiotropic viruses can cause pericardial and myocardial inflammation via direct cytolytic or cytotoxic effects and/or subsequent immune-mediated mechanisms. Many cases of myopericarditis are subclinical. In other patients, cardiac symptoms and signs are overshadowed by systemic manifestations of infection or inflammation.
Myopericarditis is more common in younger male patients. Patients will often report a recent or concurrent respiratory or gastrointestinal illness with associated fever and myalgias 4. The clinical presentation is often proportional to the extent and pattern of myocardial involvement, with many cases being subclinical or obscured by the systemic symptoms of the viral illness. Typical manifestations may include positional or pleuritic chest pain, fatigue, decreased exercise tolerance, or palpitations. In most cases, the symptom pattern does not help differentiate between simple pericarditis and myopericarditis. Furthermore, it may be difficult to differentiate myopericarditis-related chest pain from ischemic chest pain 5. Physical examination may be normal in most patients, although physical findings may be proportional to the degree of organ involvement: systemic inflammation (fever), pericardial fluid (friction rub), and acute heart failure (jugular venous pressure, gallop, edema, rales, etc.).
The increased sensitivity of troponin assays and contemporary widespread use of troponins has greatly increased the reported number of cases. Management is similar to that reported for pericarditis, generally with a reduction of empiric anti-inflammatory doses mainly aimed at the control of symptoms. Rest and avoidance of physical activity beyond normal sedentary activities has been recommended for 6 months, is recommended as for myocarditis. At present, there is no evidence that troponin elevation confers worse prognosis (i.e., a greater risk of recurrence, death or transplantation) in patients with preserved left ventricular function. Usually complete remission is seen in 3-6 months.
The exact incidence and prevalence of myopericarditis have not been established. Acute pericarditis is the admitting diagnosis in 0.1% of hospital admissions. It is estimated the incidence of myocarditis is around 1 to 10 cases per 100,000 persons 2. Vaccine-associated myocarditis has been reported in 0.01% of military recruits following smallpox vaccination 2.
Myopericarditis has a good overall prognosis 6. Troponin elevation in this setting does not predict an adverse outcome in most cases. Thus it is important to reassure the patients on their prognosis, explaining the nature of the disease and the likely course. Diagnostic and therapeutic choices should take into account the overall good outcome of these patients, including less invasive diagnostic tools and toxic drugs.
Sudden cardiac death after strenuous exercise is a rare but observed complication of pericarditis and myopericarditis. Accordingly, experts generally recommend restricting patients from physical exercise for at least 6 months after a myopericarditis diagnosis 7; prolonged physical exertion restriction may be needed on an individual basis.
Myopericarditis causes
The majority of cases of myopericarditis are idiopathic as no definitive cause is identified even after extensive work up. Causes are divided into infectious and non-infectious causes 8. Viral infections are the most common cause in the developed world. The viruses typically seen in North America are coxsackievirus, adenoviruses, cytomegalovirus, Epstein-Barr virus, influenza, hepatitis A and C, varicella zoster, and parvovirus B19 8.
Bacterial causes are less common, with tuberculosis being the most important worldwide, particularly in association with HIV. There have been case reports implicating Campylobacter jejuni and Shigella. There have also been rare cases associating myopericarditis with Neisseria meningitides, Chlamydophila pneumoniae, streptococcal pharyngitis or tonsillitis, and even community-acquired bacterial pneumonia 8.
Myopericarditis also occurs in association with immune-mediated diseases such as vasculitis (principally giant-cell arteritis), systemic lupus erythematosus, adult-onset Still’s disease, and inflammatory bowel disease. It has also been described in patients exposed to different drugs, including antineoplastic agents (e.g., 5-fluorouracil), phenytoin, antipsychotics (e.g., clozapine), and mesalazine. Last, it has been well described in association with the vaccinia (smallpox) vaccine and rarely in association with other vaccines (such as diphtheria, tetanus, and polio) 8.
A typical viral infection may involve direct cytolytic and cytotoxic-mediated inflammation in the pericardium and myocardium and/or indirect injury through immunopathic mechanisms such as molecular mimicry and epitope spreading. These immune mechanisms may result in continued myopericardial inflammation even after resolution of viremia. They may also explain the pathogenesis of vasculitis-connective tissue disease, inflammatory bowel disease, radiation, and drug-induced myopericarditis 8.
Infectious causes
- Viruses: Coxsackievirus, adenoviruses, herpes viruses, echovirus, Ebstein-Barr virus, cytomegalovirus, influenza virus, hepatitis C virus, parvovirus B19
- Bacterial: Mycobacterium tuberculosis, Streptococcus, Staphylococcus, Haemophilus, Legionella, Mycoplasma
- Fungal: Histoplasma, Aspergillus, Blastomyces, coccidioidomycosis
- Parasites: Toxoplasma, amebic, Chaga disease
Non-infectious causes
Drugs (cardiotoxic effects or hypersensitivity reactions): procainamide, isoniazid, hydralazine, alcohol, anthracycline, heavy metals
- Post-radiation to the chest cavity
- Systemic inflammatory diseases: Lupus, rheumatoid arthritis, scleroderma, Sjogren, mixed connective tissue disease
- Other inflammatory conditions: Granulomatosis, inflammatory bowel disease
- Metastatic cancers: Especially lung cancer, breast cancer, melanoma
- Primary cardiac tumors: Rhabdomyosarcoma
- Metabolic: Hypothyroidism, Renal failure/uremia
- Vaccine-associated myopericarditis
Myopericarditis symptoms
Clinical features depend on the degree of the inflammation of the pericardium, myocardium, and acuity of the illness. The clinical presentation can differ from a subtle, self-limiting illness to severe cardiogenic shock and death 2. Early symptoms included precordial chest pain, fatigue, dyspnea, palpitations, and fever. Patients may give symptoms suggestive of a viral prodrome (a runny nose, arthralgia, low-grade fever) 1 to 2 weeks preceding the presentation. In predominant pericardial involvement, they can describe the pain as sharp, worse with a cough or inspiration and relieved by sitting forward. If there is significant myocardial involvement, there may be a continuous pain, and sometimes, it is hard to differentiate from myocardial ischemia pain, especially in people with cardiovascular risk factors. They may also have predominant heart failure symptoms such as shortness of breath, orthopnea, pedal edema, and fatigue. Rare symptoms include arrhythmias, syncope, and sudden cardiac arrest. Physical examination findings can be variable, but common findings may include fever, pericardial friction rub and features of heart failure. Look for other signs of systemic illness which may contribute to the cause.
Myopericarditis diagnosis
The diagnosis of myopericarditis is suspected based on the history of pleuro-pericarditis chest pain, findings on the clinical exam like pericardial friction rub associated with typical changes of ECG and elevated cardiac biomarkers. Elevated markers of inflammation will support the diagnosis of myopericarditis and echocardiogram is done to assess the left ventricular function and pericardial involvement. In patients with atherosclerotic risk factors, they will need cardiac catheterization to rule out obstructive epicardial coronary artery disease. Cardiac magnetic resonance imaging is a useful test to assess the degree of myocardial involvement especially in patients with hemodynamic instability or symptoms of heart failure or cardiac arrhythmias.
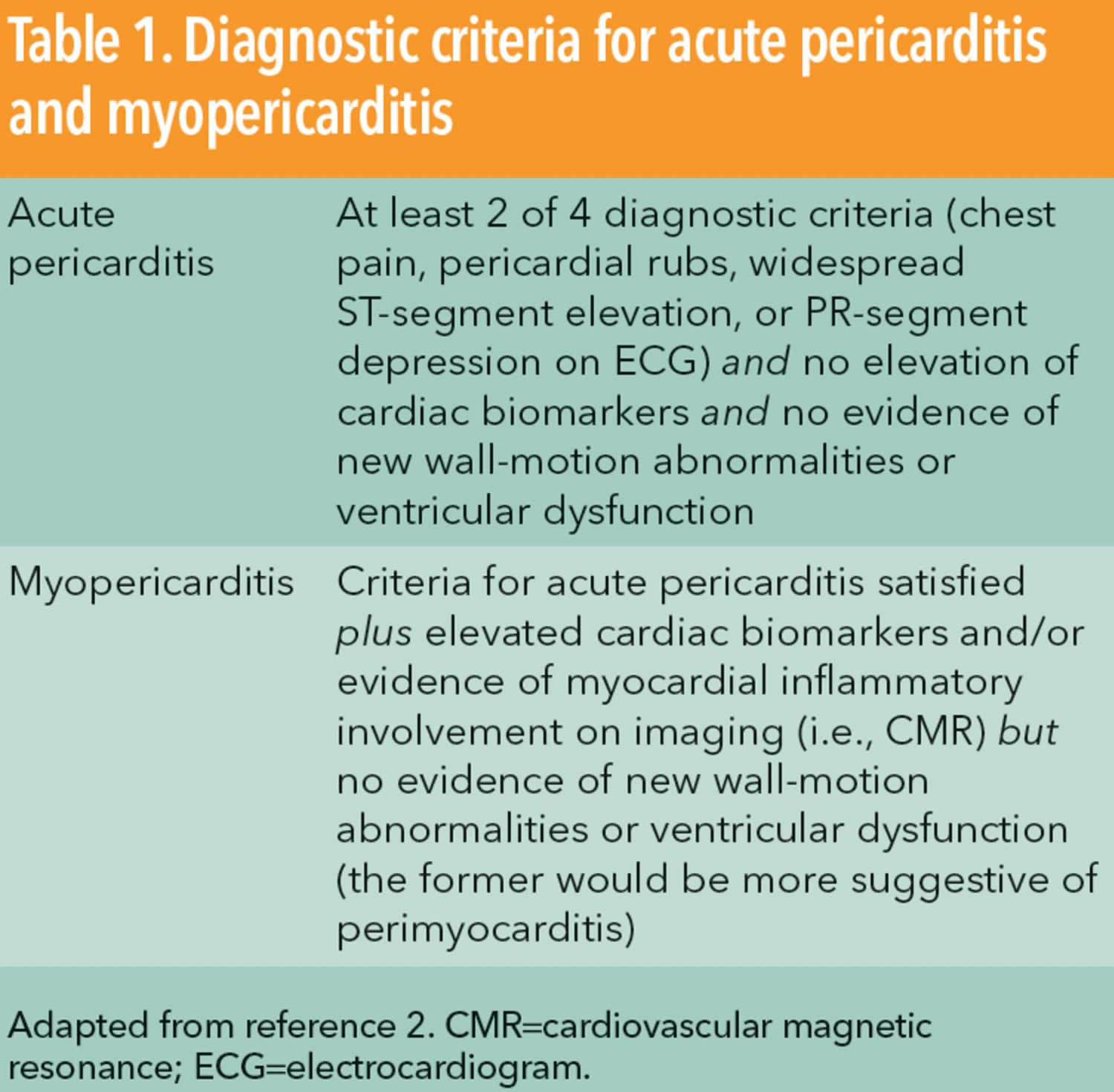
Diagnostic criteria
Myopericarditis is diagnosed when the patient satisfies the diagnostic criteria for pericarditis (see Table 1 below) and also demonstrates evidence of myocardial inflammation (i.e., elevated cardiac enzymes or inflammation seen on cardiac MRI). In addition, the patient should not have evidence of significant myocardial dysfunction on echocardiogram (which would be more suggestive of perimyocarditis) 8.
- Acute pericarditis is diagnosed in the presence of 2 or more of the following features: Pleuro-pericarditis chest pain, pericardial friction rub on the exam, ECG changes (diffuse concave ST-segment elevation and PR depression), or pericardial effusion 9.
- Myopericarditis is diagnosed in the presence of one additional feature: Elevated cardiac biomarkers, presumed new Left ventricular systolic dysfunction based on echocardiography or cardiac magnetic resonance imaging (CMR), myocardial inflammation by cardiac magnetic resonance imaging.
Laboratory studies
Myopericarditis can result in elevation of markers of inflammation like erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), white blood cell and cardiac biomarkers suggesting myocardial involvement. All the patients should also have routine blood work to rule out thyroid pathology, hepatitis, and renal function. Workup with serological markers is undertaken in patients with persistent symptoms or associated with signs of such illness. Routine viral serologies are unlikely to be helpful in the diagnostics process as the results from these studies rarely alter the treatment.
Viral and serologic studies
Experts do not routinely recommend serological studies in the setting of uncomplicated pericarditis or myopericarditis. The vast majority of pericarditis and myopericarditis cases in immunocompetent hosts from developed countries are viral or idiopathic in origin. Furthermore, a viral cause for myocarditis can only be proven if the virus is detected within altered myocardium by histopathology 10. As a result, a comprehensive workup is unlikely to add value to the patient’s care and would add unnecessary cost. It seems reasonable to follow the general guidelines for pericarditis, which recommend an extensive etiologic workup in higher-risk patients with fever, subacute onset, immunosuppression, trauma, oral anticoagulant therapy, or severe pericardial effusion 11. In addition, patients in whom conservative therapy fails should be considered for more exhaustive workup, including serologic studies.
Electrocardiogram
Typical ECG findings of pericarditis include diffuse concave ST-segment elevation and PR depression. Depending on the degree of myocardial involvement, these classic changes may or may not be present with diffuse T-wave changes or inversions. Even though ST-segment changes are diffuse in most cases, it is not uncommon to see localized ECG changes (inferolateral or anterolateral) depending on the degree of the involvement. Common arrhythmias include supraventricular or ventricular ectopic beats or non-sustained ventricular arrhythmias.
Chest radiography
Chest x-ray is normal in most of the self-limiting and minor forms of the disease or may reveal an enlarged cardiac silhouette suggesting significant fluid accumulation in the pericardial space in some patients. There may be signs of heart failure as well in some very sick patients.
Echocardiogram
An echocardiogram is routinely performed and in most patients may be normal with normal heart function with a trace or no significant pericardial effusion. Researchers have described increased pericardial brightness as a marker of the pericardial inflammation, but this is a non-specific finding with limited specificity.
Some patients may have significant pericardial fluid accumulation with or without hemodynamic compromise (tamponade physiology). An echocardiogram will also assess the left and right ventricular function and associated valvular heart disease abnormalities 12. Patients with reduced left ventricular function are preferably managed in tertiary centers, and these patients have high morbidity and mortality.
Coronary angiography
Coronary angiography is not indicated in young patients with typical features of myopericarditis, but in patients with risk factors for atherosclerotic cardiovascular disease it may be difficult to differentiate from myocardial ischemia based on non-invasive tests and would need cardiac catheterization to rule out acute coronary syndrome.
Cardiac Magnetic Resonance Imaging
Cardiac magnetic resonance imaging (CMR) can be a very good diagnostic test in these patients to assess the degree of myocardial and pericardial involvement. In patients with myopericarditis, subepicardial or mid-myocardial inflammatory changes are seen along with myocardial edema in different vascular territories, as opposed to subendocardial or transmural myocardial enhancement in one arterial territory in acute coronary syndrome. Cardiac magnetic resonance imaging will also assess the left ventricular function. Pericarditis can be diagnosed on cardiac magnetic resonance imaging by the presence of noncalcified pericardial thickening with pericardial effusion.
Endomyocardial biopsy
Endomyocardial biopsy may be needed in a few selective sick patients, who exhibit clinical signs of continued deterioration despite standard supportive care. In these patients, endomyocardial biopsy is recommended if it may alter treatment options, for example for giant cell arteritis.
Myopericarditis treatment
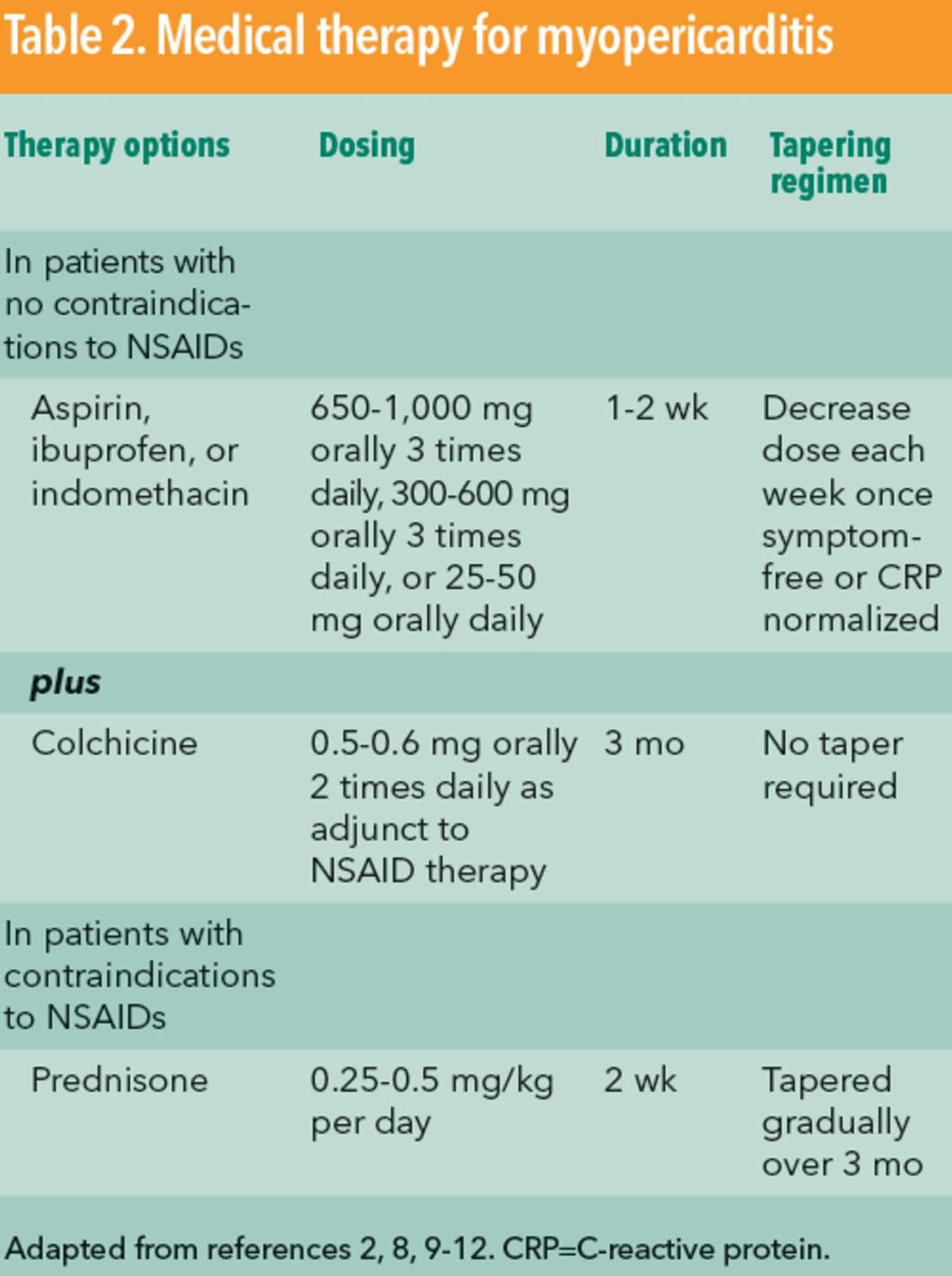
The overall prognosis of myopericarditis is very good with no long-term complications in most patients 13. Limited data are available to guide the treatment of myopericarditis. Given that most myopericarditis cases are idiopathic or viral in origin, the current evidence does not support any specific therapies aimed at the underlying causal agent. If the presenting illness has more of pericarditis symptoms with preserved left ventricular function, nonsteroidal anti-inflammatory drugs (NSAIDs) are the first line of drugs used (see Table 2 below). Current recommendations are generally based on the 2004 European Society of Cardiology guidelines 14. NSAID regimens include ibuprofen, aspirin, or indomethacin and are summarized along with other treatments in Table 2. NSAIDs are generally administered over several weeks at therapeutic doses and then gradually tapered. C-reactive protein measurements can be used to predict a higher rate of recurrence and to monitor disease progression while guiding therapy duration 15. In patients with contraindications to NSAID therapy, corticosteroids can be used as a second-line agent but are generally tapered more gradually. Colchicine can be used as an adjunct to NSAID therapy and has been shown to reduce symptom duration and rate of recurrence in pericarditis 16. But in patients with significant myocardial involvement, caution is suggested with NSAIDS, as they can worsen the myocardial function. In these patients, minimal doses of NSAIDs are used to achieve symptomatic relief.
Currently there is insufficient evidence to support using colchicine in myopericarditis; however, it seems reasonable to consider on an individual basis. Patients at high risk for gastrointestinal bleeding complications (history of peptic ulcer disease, advanced age, concurrent anticoagulation) should be prescribed acid prophylaxis. Corticosteroids are usually used in specific conditions like giant cell myocarditis or recurrent pericarditis.
In cases where there is significant left ventricular dysfunction (e.g., perimyocarditis), the patient should be concurrently treated with conventional heart failure methods and expert cardiology consultation. Sudden cardiac death after strenuous exercise is a rare but observed complication of pericarditis and myopericarditis. Accordingly, experts generally recommend restricting patients from physical exercise for at least 6 months after a myopericarditis diagnosis 7; prolonged physical exertion restriction may be needed on an individual basis.
In patients with significant pericardial effusion associated with pericardial tamponade, percutaneous or surgical drainage is recommended for hemodynamic stabilization. In patients with signs and symptoms of heart failure with myocardial involvement, standard heart failure therapy with beta blockers and angiotensin-converting enzyme inhibitors and/or diuretics are recommended.
When to admit
Experts recommend initial hospitalization for all patients with suspected myopericarditis 17. The primary objectives in evaluating a patient with suspected myopericarditis should be 1) establishing the diagnosis, 2) excluding an acute coronary syndrome, and 3) assessing for significant left ventricular dysfunction or other high-risk features. Once the diagnosis of myopericarditis has been established and no high-risk features have been found (such as ventricular arrhythmias or significant left ventricular dysfunction), the patient can be safely discharged.
Vaccine-associated myopericarditis
Symptoms and signs of myopericarditis occurring within 30 days of a vaccine are defined as vaccine-associated myopericarditis in the absence of other pathology. These symptoms have reported following smallpox vaccine, and the incidence is about 0.01% 18. Diagnostic tests and treatment are similar to what has been described above. Most patients will make a spontaneous recovery, but a small fraction of patients with highly-active viral infection as evidenced by polymerase chain reaction (PCR) may need treatment with vaccinia immune globulin.
Myopericarditis prognosis
In a recent systematic review with up to 31 months of follow-up, authors demonstrated a favorable long-term prognosis for myopericarditis. The reported pericardial complications seen with simple pericarditis, such as recurrent pericarditis, cardiac tamponade, and constrictive pericarditis, were exceedingly rare 7. The overall mortality rates reported in this review were also low, with only 3 reported deaths out of 389 patients followed, and only 1 study out of 8 reporting any deaths associated with myopericarditis. In those cases, all 3 deaths occurred during the initial hospitalization; 1 death resulted from cardiac tamponade and the other 2 resulted from sudden cardiac death. The authors concluded that in the absence of significant myocardial dysfunction, the presence of myocardial involvement in pericarditis (also known as myopericarditis) is not a negative prognostic marker.
References- Massimo Imazio & Leslie T Cooper (2013) Management of myopericarditis, Expert Review of Cardiovascular Therapy, 11:2, 193-201, DOI: 10.1586/erc.12.184 https://doi.org/10.1586/erc.12.184
- Manda YR, Baradhi KM. Myopericarditis. [Updated 2019 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534776
- Imazio M, Trinchero R. Myopericarditis: Etiology, management, and prognosis. Int. J. Cardiol. 2008 Jun 23;127(1):17-26.
- Imazio M, Cecchi E, Demichelis B, Chinaglia A, Ierna S, Demarie D, et al. Myopericarditis versus viral or idiopathic acute pericarditis. Heart. 2008;94:498-501.
- Imazio M, Trinchero R. Myopericarditis: Etiology, management, and prognosis. Int J Cardiol. 2008;127:17-26. doi:10.1016/j.ijcard.2007.10.053
- Prognosis of myopericarditis as determined from previously published reports. J Cardiovasc Med (Hagerstown). 2014 Dec;15(12):835-9. doi: 10.2459/JCM.0000000000000082 https://journals.lww.com/jcardiovascularmedicine/Abstract/2014/12000/Prognosis_of_myopericarditis_as_determined_from.1.aspx
- Imazio M, Brucato A, Spodick DH, Adler Y. Prognosis of myopericarditis as determined from previously published reports. J Cardiovasc Med (Hagerstown). 2014;15:835-9. doi:10.2459/JCM.0000000000000082
- Imazio M, Cooper LT. Management of myopericarditis. Expert Rev Cardiovasc Ther. 2013 Feb;11(2):193-201. doi: 10.1586/erc.12.184 https://doi.org/10.1586/erc.12.184
- Imazio M, Trinchero R. Triage and management of acute pericarditis. Int. J. Cardiol. 2007 Jun 12;118(3):286-94.
- Oakley CM. Myocarditis, pericarditis and other pericardial diseases. Heart. 2000;84:449-54.
- Lurz P, Eitel I, Adam J, Steiner J, Grothoff M, Desch S, et al. Diagnostic performance of CMR imaging compared with EMB in patients with suspected myocarditis. JACC Cardiovasc Imaging. 2012;5:513-24. doi:10.1016/j.jcmg.2011.11.022
- Klein AL, Abbara S, Agler DA, Appleton CP, Asher CR, Hoit B, Hung J, Garcia MJ, Kronzon I, Oh JK, Rodriguez ER, Schaff HV, Schoenhagen P, Tan CD, White RD. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013 Sep;26(9):965-1012.e15
- Imazio M, Brucato A, Spodick DH, Adler Y. Prognosis of myopericarditis as determined from previously published reports. J Cardiovasc Med (Hagerstown). 2014 Dec;15(12):835-9.
- Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmüller R, Adler Y, et al. Task Force on the Diagnosis and Management of Pricardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587-610.
- Imazio M, Brucato A, Maestroni S, Cumetti D, Dominelli A, Natale G, et al. Prevalence of C-reactive protein elevation and time course of normalization in acute pericarditis: implications for the diagnosis, therapy, and prognosis of pericarditis. Circulation. 2011;123:1092-7. doi:10.1161/CIRCULATIONAHA.110.986372
- Imazio M, Brucato A, Cemin R, Ferrua S, Maggiolini S, Beqaraj F, et al. ICAP Investigators. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013;369:1522-8. doi:10.1056/NEJMoa1208536
- Imazio M, Cooper LT. Management of myopericarditis. Expert Rev Cardiovasc Ther. 2013;11:193-201. doi:10.1586/erc.12.184
- Halsell JS, Riddle JR, Atwood JE, Gardner P, Shope R, Poland GA, Gray GC, Ostroff S, Eckart RE, Hospenthal DR, Gibson RL, Grabenstein JD, Arness MK, Tornberg DN., Department of Defense Smallpox Vaccination Clinical Evaluation Team. Myopericarditis following smallpox vaccination among vaccinia-naive US military personnel. JAMA. 2003 Jun 25;289(24):3283-9.