What is obstructive uropathy
Obstructive uropathy is a catch-all term encompassing any cause of complete or partial, congenital or acquired and permanent or intermittent obstruction to the urinary tract 1. Depending on the severity of obstruction and extent, it may result in permanent change in both the collecting system proximal to the obstruction and to the renal parenchyma which normally drains into the affected collecting system. Obstructive uropathy is a common cause of acute and chronic renal failure 2.
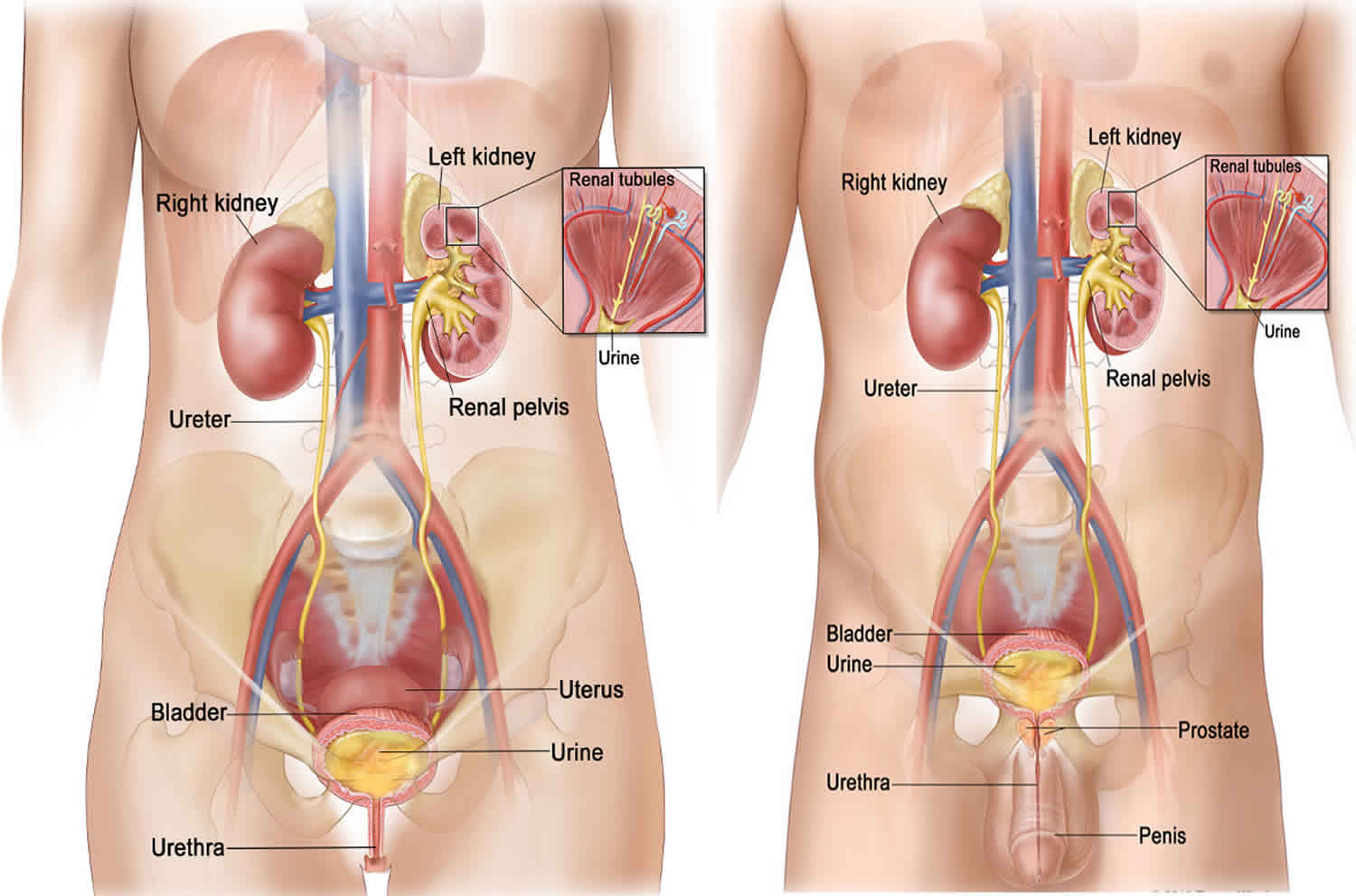
Normal urine production in an adult is about 1.5-2 L/day. Urine flow depends on 3 factors—a pressure gradient from the glomerulus to the Bowman capsule, peristalsis of the renal pelvis and ureters, and the effects of gravity (ie, hydrostatic pressure).
Obstruction of the urinary tract at any level eventually results in elevation of intraluminal ureteral pressure. With prolonged obstruction, ureteral peristalsis is overcome and increased hydrostatic pressures are transmitted directly to the nephron tubules.
As pressures in the proximal tubule and Bowman space increase, glomerular filtration rate (GFR) falls. After 12-24 hours of complete obstruction, intratubular pressure decreases to preobstruction levels. If complete obstruction is not relieved, a depressed GFR is maintained by decreases in renal blood flow mediated by thromboxane A2 and angiotensin 2 (angiotensin II). With continued obstruction, renal blood flow progressively falls, resulting in ischemia and incremental nephron loss. Thus, obstructive uropathy may lead to obstructive nephropathy. Several phases of obstructive nephropathy may be seen, including an early hyperemia and a late vasoconstriction followed by regulation of GFR post obstruction. Recovery of GFR depends on the duration and level of obstruction, preobstruction blood flow, and coexisting medical illness or infection.
Obstructive uropathy causes
Obstructive uropathy causes include:
- Ureter
- transitional cell carcinoma of the ureter
- retrocaval ureter
- urolithiasis
- ureterocoele
- Bladder
- transitional cell carcinoma (TCC) of the bladder
- Urethra
- posterior urethral valves (PUV)
- urethral atresia
- urethral stenosis
- urethral carcinoma
- benign prostatic hypertrophy (BPH)
Infants and children obstructive uropathy causes
Urethral and bladder outlet obstruction may be associated with the following:
- Urethral atresia
- Phimosis
- Meatal stenosis
- Anterior and posterior urethral valves (males)
- Calculus (Southeast Asia)
- Blood clot
- Neurogenic bladder (meningomyelocele)
- Ureterocele
Ureteral obstruction may be associated with the following:
- Vesicoureteral reflux (female preponderance)
- Ureterovesical junction narrowing or obstruction
- Ureterocele
- Retrocaval ureter
- Retroperitoneal tumor
- Megaureter -Prune belly syndrome
- Blood clot
- Ureteropelvic junction narrowing or obstruction
In a study 3 of 56 patients (42 boys, 14 girls) younger than 18 years who presented to the emergency department with acute urinary retention, causes of urinary retention were mechanical obstruction in 14 patients (25%), infection or inflammation in 10 (18%), fecal impaction in 7 (13%), neurologic disorders in 6 (11%), gynecologic disorders in 4 (7%), and behavioral processes in 3 (5%); 12 patients (21%) were idiopathic. All patients with mechanical obstruction were boys, 5 of whom had a pelvic tumor. Fifteen children underwent surgery, and 3 children required continuous catheterization during follow-up.
Adults obstructive uropathy causes
Urethral and bladder outlet obstruction may be associated with the following:
- Phimosis
- Stricture (male preponderance)
- Sexually transmitted diseases (STDs), particularly in women with severe genital herpes involving the urethral orifice, occasionally in males with significant prostatitis or purulent urethritis
- Trauma
- Blood clot
- Calculi
- Benign prostate hypertrophy (BPH)
- Cancer of prostate or bladder
- Carcinoma of cervix or colon
- Neurogenic bladder (diabetes mellitus, spinal cord disease, multiple sclerosis, Parkinson disease, anticholinergic drugs, alpha-adrenergic antagonists, calcium channel blockers, opioids, sedative-hypnotics) 4
Ureteral obstruction may be associated with the following:
- Vesicoureteral reflux (female preponderance)
- Calculi
- Uric acid crystals
- Blood clot
- Trauma
- Papillary necrosis (sickle cell disease, diabetes mellitus, pyelonephritis)
- Inflammatory bowel disease
- Pregnant uterus
- Aortic aneurysm
- Carcinoma of ureter, uterus, prostate, bladder, colon, or rectum
- Retroperitoneal fibrosis
- Idiopathic tumors (cervix, uterus, prostate, colon)
- Tuberculosis
- Sarcoidosis
- Chronic UTI (methysergide, propranolol)
- Retroperitoneal lymphoma
- Uterine leiomyomata
- Stricture (tuberculosis, radiation, schistosomiasis, nonsteroidal anti-inflammatory drugs [NSAIDs])
- Accidental surgical ligation
Intrarenal obstruction may be associated with the following:
- Crystals (uric acid, sulfonamide, acyclovir)
- Protein casts (multiple myeloma, amyloidosis)
Obstructive uropathy symptoms
Most acute obstructive uropathies are associated with significant pain or abrupt diminution of urine flow; however, chronic urinary obstruction is insidious and requires a careful history and a high index of suspicion. The following may be noted in urinary obstruction:
- Pain (most common symptom in acute obstruction but typically absent with slowly obstructing conditions)
- Altered patterns of micturition
- Acute and chronic renal failure
- Gross or microscopic hematuria
- Recurrent urinary tract infection (UTI)
- New-onset or poorly controlled hypertension secondary to obstruction and increased renin-angiotensin
- Polycythemia secondary to increased erythropoietin production in the hydronephrotic kidney
- History of recent gynecologic or abdominal surgery
Most acute obstructive uropathies are associated with significant pain or the abrupt diminution of urine flow that alerts the clinician to the need for further evaluation and treatment. However, the insidious nature of chronic urinary obstruction requires a careful history and a high index of suspicion, which prompt an appropriate evaluation that may confirm or rule out the presence of obstruction. A large (933 patients) prospective study by de la Rosette et al 5 failed to correlate a wide range of symptoms of lower urinary tract obstruction with bladder outflow studies.
Pain secondary to stretching of the urinary collecting system is the most common symptom in acute obstruction. Prevalence of pain is related more to acuity of obstruction than degree of distention. Acute obstruction of the ureter by a calculus commonly results in an excruciating pain, commonly referred to as renal colic. This pain is described as unrelenting, radiating from the flank to lower abdomen and testicles or labia on the affected side.
Patients often present to the emergency department with acute urinary tract disorders manifesting as flank pain. Because laboratory and clinical findings (eg, hematuria) are neither sensitive nor specific for identifying the cause of the flank pain, imaging is important for both diagnosis and management 6.
By contrast, pathological processes that slowly obstruct, such as retroperitoneal tumors, are relatively pain free. Prostatic hypertrophy also may be associated with an obstructive uropathy that is relatively painless. It usually is identified when a superimposed acute obstruction occurs with the inability to void effectively; the resultant painful, distended bladder prompts a visit to an emergency physician.
Alterations in patterns of micturition often associated with more distal obstructions are early but frequently missed symptoms. Although anuria is dramatic and specific for obstruction, nocturia and polyuria are much more common presenting symptoms associated with renal concentrating defects due to partial obstruction. Bladder outlet obstruction leads to the symptoms of prostatism (eg, frequency, urgency, hesitancy, dribbling, decrease in voiding stream, the need to double void).
Acute and chronic renal failures are common complications of urinary obstruction. Obstructive nephropathy should be considered especially in uremic patients without a previous history of renal disease, hypertension, or diabetes.
Gross or microscopic hematuria often is associated with renal calculi, papillary necrosis, and tumors, all of which can cause obstruction.
Recurrent UTIs should always lead to an investigation for urinary obstruction.
New-onset or poorly controlled hypertension secondary to obstruction and increased renin-angiotensin has been reported.
Polycythemia secondary to increased erythropoietin production in the hydronephrotic kidney also has been reported.
History of recent gynecologic or abdominal surgery can give important clues to the etiology of urinary obstruction.
Pediatric patients may present with recurrent infections. Symptoms of voiding dysfunction such as enuresis, incontinence, or urgency should be sought.
A thorough medication history should be elicited. A variety of drugs and toxins affect renal function. Bladder dysfunction is seen with a variety of xenobiotic drugs with antimuscarinic anticholinergic activity such as antihistamines, antipsychotics, and antidepressants. A variety of xenobiotics such as ethylene glycol, indinavir, methotrexate, phenylbutazone, or sulfonamides will induce crystal deposition throughout the tubulointerstium obstructing urine output. Additionally, drug-induced retroperitoneal fibrosis may obstruct ureteral function such as methysergide or other natural-occurring ergotamines.
In cases of both acute and chronic obstructive uropathy, occupational exposure history may be beneficial. For example, in textile manufactures, shipyard workers, roofers, or asbestos miners, retroperitoneal fibrosis due to asbestos-induced mesothelioma should be considered. Bladder cancer–induced outlet obstruction may occur in textile workers, rubber manufacturing workers, leather workers, painters, hairdressers, or drill press workers exposed to alpha- or beta-naphthylamine, 4-aminobiphenyl, benzidine, chlornaphazine, 4-chlor-o-toluidine, 2-chloroaniline, phenacetin compounds, benzidine azo dyes, or methylenedianiline.
Obstructive uropathy diagnosis
Physical exam
The physical examination should include the following:
- Evaluation for signs of dehydration and intravascular volume depletion; peripheral edema, hypertension, and signs of congestive heart failure from fluid overload may be observed in obstruction from renal failure
- Palpable kidney or bladder (indicative of a dilated urinary collection system)
- Rectal or pelvic examination to help determine whether enlargement of pelvic organs is a possible source of urinary obstruction.
- Examination of the external urethra for phimosis or meatal stenosis
Lab studies
Laboratory studies that may be helpful include the following:
- Urinalysis and examination of sediment
- Urinary diagnostic indices (eg, sodium, creatinine, osmolality)
- Serum electrolytes (sodium, potassium, chloride, bicarbonate), as well as blood urea nitrogen (BUN), creatinine, calcium, phosphate, magnesium, uric acid, and albumin
- Complete blood count (CBC)
Imaging studies
The goals of any imaging study are to distinguish anatomic etiologies from functional forms of collecting system dilation and to identify the site of blockage. Imaging studies that may be considered include the following:
- CT – Helical CT (especially without contrast) rapidly is replacing kidneys-ureters-bladder (KUB) x-rays as the first step in the radiologic evaluation of the urinary system
- MRI – Where available, MRI quickly is becoming the imaging study of choice for urinary obstruction
- IV pyelography (IVP) – IVP is the procedure of choice for defining the extent and anatomy of obstruction
- Invasive pyelography – This modality provides the same information as IVP without depending on renal function and can be used when the risks of IVP are considered too great
- Ultrasonography – This is the procedure of choice for determining the presence of hydronephrosis
Obstructive uropathy treatment
The overriding therapeutic goal is reestablishment of urinary flow. Before specific therapy for obstruction is initiated, the life-threatening complications of obstructive uropathy must be investigated and treatment started.
Once urinary obstruction is under consideration, a transurethral bladder catheter should be placed:
- If the catheter is properly placed and fluid returns freely, the catheter tip is probably in the bladder, and obstruction above the bladder should be investigated; if a question still remains, imaging studies may be used to establish proper placement
- If a large postvoid residual (PVR) volume is noted, obstruction below the bladder should be investigated; catheter drainage should be maintained until the cause of the obstruction is treated appropriately
- Urine should be drained completely and rapidly from an obstructed bladder; prolonged urine stasis only predisposes the patient to UTI, urosepsis, and renal failure
- A urologist should be consulted when a transurethral catheter cannot provide adequate bladder drainage
Calculi are the most common causes of unilateral ureteral obstruction. The following considerations apply:
- Most small renal calculi pass spontaneously; conservative treatment typically suffices
- Surgical drainage is necessary only for patients with unrelenting pain, UTI, or persistent obstruction
- The position of the stone in the ureter determines the preferred method of removal
- Calculi in the renal pelvis and proximal ureter are amenable to nephroscopy and removal under direct visualization
- Percutaneous nephrostomy drainage is used for midureteral stones
- Distal ureter stones can be removed cystoscopically by the use of a loop or basket
- Extracorporeal shock wave lithotripsy is another viable option for stones in any position in the ureter
Bilateral obstruction of the ureters is almost always asymmetric. The following considerations apply:
- For midureteral or proximal ureteral obstruction, percutaneous nephrostomy tube placement is indicated
- For distal obstruction, cystoscopic placement of a ureteral stent can be attempted
- In case of suspected urosepsis from bilateral ureteral obstruction, bilateral percutaneous nephrostomy tubes must be placed
For obstruction of prostatic origin, medical therapy for benign prostate hypertrophy (BPH) has provided a very successful alternative to surgical therapy but should not be offered to individuals presenting with absolute indications for surgical intervention (eg, recurrent urinary retention, recurrent UTIs, renal insufficiency, bladder calculi, recurrent gross hematuria) 7.
References- Mujoomdar M, Russell E, Dionne F, et al. Optimizing Health System Use of Medical Isotopes and Other Imaging Modalities [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2012. APPENDIX 2.17, Suspected Obstructive Uropathy. Available from: https://www.ncbi.nlm.nih.gov/books/NBK174850
- Urinary Obstruction. https://emedicine.medscape.com/article/778456-overview
- Nevo A, Mano R, Livne PM, Sivan B, Ben-Meir D. Urinary retention in children. Urology. 2014 Dec. 84 (6):1475-9.
- Elhebir ES, Hughes JD, Hilmi SC. Calcium Antagonists Use and Its Association with Lower Urinary Tract Symptoms: A Cross-Sectional Study. PLoS One. 2013. 8(6):e66708
- de la Rosette JJ, Witjes WP, Schafer W, et al. Relationships between lower urinary tract symptoms and bladder outlet obstruction: results from the ICS-“BPH” study. Neurourol Urodyn. 1998. 17(2):99-108.
- Goel RH, Unnikrishnan R, Remer EM. Acute Urinary Tract Disorders. Radiol Clin North Am. 2015 Nov. 53 (6):1273-92.
- Shin SH, Kim JW, Kim JW, Oh MM, Moon du G. Defining the degree of intravesical prostatic protrusion in association with bladder outlet obstruction. Korean J Urol. 2013 Jun. 54(6):369-72.