Onychorrhexis
Onychorrhexis is increased nail brittleness with longitudinal ridging and fissuring of the nail plate. Onychorrhexis is particularly frequent among middle-age women and characterized by longitudinal splitting and shallow parallel furrows running on the superficial layer of the nail (Figure 2). Some people may have onychorrhexis on only one nail while others will have it on all nails. The severity of the clinical presentation depends on the degree of the causative factor on the nail matrix. Longitudinal ridges may vary from a few superficial ridges up to deep furrows, affecting from a small part of the nail surface to at least 70% of the total nail surface. Likewise, longitudinal splitting may vary from a few superficial splits up to multiple deep fissures. A single longitudinal split of the entire nail plate is sometimes observed (split nail) (Figure 3). The pain induced by the deep splits may be the cause for medical advice being sought. According to causative factors, scientists can distinguish 2 forms of nail fragility: a primary “idiopathic or brittle nail syndrome” form and nail fragility secondary to different causes such as inflammatory nail disorders, infections, systemic diseases and general conditions, traumas and alteration of the nail hydration 1. Onychorrhexis can occur with several conditions, such as hypothyroidism, anemia, bulimia, ageing, lichen planus, psoriasis, fungal nail infection and Darier disease. Onychorrhexis may also be associated with use of nail polish remover or nail picking 2.
Optimal management requires treatment of the primary cause of brittle nails, when possible. In idiopathic nail fragility oral supplementation, vitamins (especially biotin, also known as vitamin B7), trace elements and amino acids (especially cysteine) have been reported to be useful. In addition, several products, such as topical moisturizers and lacquers could be considered to restructure the affected nail plate and to reduce psychological impacts of this common problem.
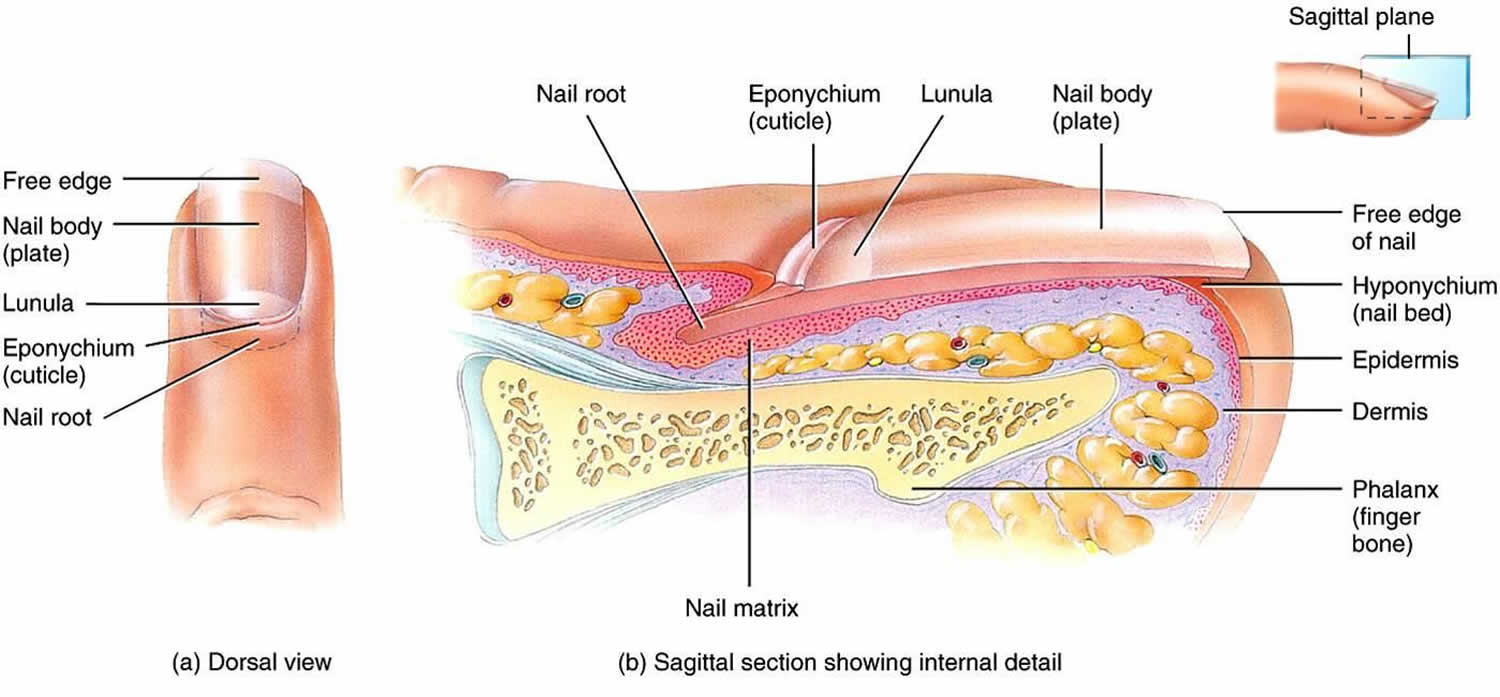
Figure 1. Nail anatomy
Figure 2. Onychorrhexis nails
Footnote: Several longitudinal parallel furrows and thin fissures running on the superficial layer of the nail.
[Source 1 ]Figure 3. Onychorrhexis
Footnote: Onychorrhexis presenting as single longitudinal split of nail plate.
[Source 1 ]Figure 4. Onychorrhexis due to lichen planus
Footnote: Nail fragility due to nail lichen planus: nail plate thinning, longitudinal fissuring and splitting of the nail plate.
[Source 1 ]Onychorrhexis causes
There are 2 forms of nail fragility: a primary “idiopathic” form and nail fragility secondary to different causes 1. Primary brittle nails are speculated to develop from the impairment of intercellular adhesive factors of the nail matrix or abnormalities in epidermal growth and keratinization. Brittle nails of secondary origin are typically linked to disordered keratinization from dermatologic disease or systemic disorders, such as endocrine, metabolic, or vascular abnormalities. Other precipitating factors for brittle nails include the repetitive wetting and drying of the hands, direct contact with chemicals (nail polish remover), trauma to the nail, and onychomycosis 3.
Causes of brittle nails include:
- Idiopathic Nail Brittleness (Brittle Nail Syndrome): This is the most common cause of nail brittleness, almost exclusively seen in the fingernails. In women, the intercellular keratinocyte bridges are constitutionally weaker than in males and this can be considered a cause of the higher frequency of this complaint among females. Moreover, normal nails contain 5% lipids and there is a decrease in cholesterol sulphate of the nail plate with age, especially in post-menopausal women, suggesting an important role of lipids in the development of nail brittleness 4. Some authors have identified reduced water content in the nail plate (< 16%) as a possible cause of brittle nails 5. In contrast, other studies found no significant difference in water content of brittle compared with normal nails 6.
- Secondary Nail Brittleness:
- Secondary to impairment of intercellular adhesive factors of the nail plate:
- exogenous factors
- immersion/desiccation – in occupations such as nursing, and hairdressing, where repetitive wetting and drying of the hands
- chemicals – in particular, occupational exposure to thioglycolates, solvents, cement, acids, alkalis, anilines, salt, and sugar solutions
- trauma – for example typing, telephone dialing, improper nail clipping (also trauma caused by excessive length of the nails)
- fungi – fungal infections may cause both intracellular and intercellular fractures in the nail plate
- exogenous factors
- Secondary to pathologic nail formation
- Causes of pathologic nail formation resulting in brittle nails include:
- endocrine and metabolic diseases such as hypopituitarism, hyperthyroidism and hypothyroidism, hypoparathyriodism, acromegaly, diabetes mellitus, gout, osteoporosis, osteomalacia, pregnancy, and malnutrition (anorexia nervosa, bulimia)
- decreased nail formation has been observed after radiation or arsenic intoxication
- reduced vascularization and oxygenation directly affect epidermal growth and keratinization
conditions that have been associated with brittle nails in this context include, arteriosclerosis and age-related decrease of circulation, microangiopathy, Raynaud’s disease, anemia, polycythemia vera (polycythemia causing sludge formation), major chronic infectious diseases (pulmonary tuberculosis, empyema, bronchiectasis), and sarcoidosis - disordered keratinization may impair nail plate formation
- if a self-limiting impairment of short duration, nail pits or spots of leuconychia may be seen
- involvement of the entire nail plate or longitudinal involvement occur secondary to processes that have impaired the nail matrix during prolonged periods – conditions that may cause such involvement include Darier’s disease, pityriasis rubra pilaris, lichen planus, and alopecia areata – these conditons may cause longitudinal ridges, longitudinal splits, or sandpaper-like nails
- psoriasis, atopic dermatitis, and mycoses may lead to a thickened nail plate with a brittle appearance
- nail growths/tumours (such as melanoma, squamous cell carcinoma, warts) are diagnosed after removal of the nail plate – however the nail plate may show longitudinal abnormalities indicative of brittlenes
- Causes of pathologic nail formation resulting in brittle nails include:
- Secondary to impairment of intercellular adhesive factors of the nail plate:
Inflammatory nail disorders
Several dermatoses such as psoriasis, lichen planus, lichen striatus, alopecia areata, Darier’s disease and eczema may involve the nail apparatus 7. Usually these disorders are diagnosed as separate entities although features of nail fragility are common in these patients.
In fact, up to 50% of patients affected by psoriasis present nail abnormalities that are frequently associated with nail brittleness. When the proximal part of the nail matrix is involved, the nail plate presents irregular and deep pits, while a more extensive psoriatic involvement of the nail matrix induces a friable and brittle nail plate 8.
Lichen planus in its various forms can also affect the nails. About 10% of patients with lichen planus have specific nail involvement 9. Depending on the degree of inflammation, the nail changes consist of thinning, longitudinal ridging and splitting of the nail plate (Figure 4). Rarely, erosive lichen planus may involve the nails 10. In lichen striatus, nail involvement is similar to that of lichen planus, but typically only half of the nail plate is affected 11.
Approximately 2/3 of patients with alopecia areata have nail changes, such as pits secondary to proximal nail matrix involvement, onychorrhexis, thinning and trachyonychia. Changes may be seen in one, several or all the nails.
Periungual eczema, seen in contact dermatitis or atopic dermatitis, is frequently associated with nail plate fragility.
Infections
Superficial white onychomycosis is an example of a cause of nail fragility secondary to nail plate damage. In this type of onychomycosis, the fungal hyphae colonize the most superficial layers of the nail plate, and it becomes white, opaque, and friable in multiple small spots secondary to keratin digestion by fungi 12.
In distal subungual onychomycosis, fungi invade the nail bed from the distal free margin of the nail plate, inducing nail fragility in the distal portion.
Several infectious diseases such as syphilis and pulmonary tuberculosis can give nonspecific alterations to the nails such as nail thinning and fissuring of the free margin and an overall fragility 13.
Systemic diseases and general conditions
Brittle nails have also been linked with systemic diseases, nutritional deficiencies and medication ingestion, but they are often only a non-specific sign that accompanies these conditions 6.
The impairment of peripheral circulation secondary to arteriopathy, neurological disorders, chronic anemia and arteriosclerosis may lead to a reduced nail matrix vascularization with production of a thin nail plate 14.
Patients with endocrine disorders may present with brittle nails, slow nail growth and longitudinal ridging and fissuring. Nail changes, characterized by brittleness and softness, are present in about 5% of cases of hyperthyroidism and are often reversible following successful therapy. The nails are affected in 90% of patients with hypothyroidism and typically appear thin, brittle, slow-growing and with longitudinal or transverse striae 15.
Onycholysis, increased fragility, longitudinal ridging and crumbling may occur in amyloidosis.
Systemic medications such as cancer chemotherapeutic agents, retinoids or antiretrovirals may be responsible for lamellar onychoschizia.
A severe deficiency of vitamins, trace elements and aminoacids from daily food intake may result in nail fragility and thinning 16.
Traumas and alteration of nail hydration
Traumas significantly contribute to damage of the nail plate and alteration of the nail plate surface. nail fragility can be caused by mechanical micro-traumas secondary to routine professional activities, as in homemakers, housemaids, shoemakers, ironworkers, and carpenters. Occupational exposure to solvents and solutions (chemical/medical personnel, photographers or painters, for example) can dissolve intercellular lipids and damage intercellular cohesion. Onychotillomania (a compulsive neurosis in which a person picks constantly at the nails or tries to tear them off) and onychophagia are another two causes of traumatic brittle nails.
The methods used to prepare nails for cosmesis and all methods of removing the applied preparations damage the healthy nail plates. However, the application of nail polish itself does not cause an alteration of the pH of the nail lamina, being approximately 5.8, which is very close to the physiological value 17. Water is stored above all in the ventral portion of the nail plate and the alteration of water content of the nail plate could cause brittle nails (Fig. 12). Dehydration is more rapid if nails are not kept short 18. Moreover, hydration and desiccation may play a significant role in household employees, hairdressers, and nurses where repeated wetting and drying of the hands leads to fractures between nail plate onychocytes.
Finally, occlusive gloves applied over wet hands while working may be a cause of brittle nails, leading to splintered, fractured nails and onychoschisis 19.
Onychorrhexis symptoms
Patients with brittle nail syndrome may frequently report that their nails are fragile, break easily, and have difficulty preserving length 20. These nail abnormalities most typically affect the first three fingernails, and fingernails are more frequently affected than toenails 21. Not only are these nail features frequently a cosmetic concern for patients, but they can also cause significant pain and discomfort 22. The brittle nail findings may be associated with the onset of systemic disease, in certain cases.
Onychorrhexis diagnosis
A thorough review of systems and a review of medical history and medications should direct subsequent workup to assess for potential systemic causes. The following medical history elements are helpful in creating a differential diagnosis:
- Occupation
- Exposures to topical substances
- Medication history
- Smoking or tar use
- Illicit drug history
- Family history of similar findings/concerns
When it comes to the specific complaint, it is important to know the following information:
- How many digits are affected and whether the condition spread or affected all digits at once
- History of trauma to the affected digits
- Any recent stress
- Whether or not all the nails appear similar.
Examination of all 20 nails is recommended. Close inspection of the nail plate, lunula, and proximal, distal, and lateral nail folds is essential. The clinician should make note of any periungual scale, erythema, or other cutaneous findings that might indicate an underlying primary dermatologic disorder. The presence of increased longitudinal or transverse nail curvature and onycholysis should be assessed. Nailfold capillaroscopy should be performed to look for irregularities in the capillaries of the proximal nail folds, which may indicate an autoimmune connective-tissue disorder. Signs of cyanosis or ischemia suggest that circulatory insufficiency may play a role in the nail abnormalities.
Assessment of ridges and longitudinal grooves
- Proposed score for ridging
- 0 = None, clear of any signs of ridging and longitudinal grooves
- 1 = Mild, few plane ridges and longitudinal grooves
- 2 = Moderate, few deep ridges and longitudinal grooves
- 3 = Severe, more than 70% of the nail plate showing deep ridges and corresponding grooves
- Proposed score for longitudinal splitting
- 0 = None, clear of clinical signs of longitudinal nail splitting
- 1 = Mild, one single, superficial longitudinal split of the nail plate
- 2 = Moderate, at least one deep longitudinal split of the entire nail plate
- 3 = Severe, multiple, superficial and deep longitudinal splits of the nail plate.
Laboratory studies
Depending on the clinical severity and pertinent positives on review of systems, it may be important to collect bloodwork to investigate further. In a brittle nail workup, physicians may be inclined to order thyroid studies, an erythrocyte sedimentation rate (marker of acute inflammation), complete blood cell counts, a comprehensive metabolic panel (which includes glucose, electrolytes, and markers of renal and hepatic function), antinuclear antibody titers, and iron (iron deficiency), ferritin, and zinc levels. If onychomycosis is suspected, nail plate and subungual debris samples should be sent for fungal culture, periodic acid-Schiff staining, and/or molecular testing.
Histologic findings
The histopathology for onychorrhexis can be variable depending on the underlying cause. Nail plate thinning seen in onychorrhexis is caused by a shortening of the nail matrix length. However, a biopsy is not always performed, as onychorrhexis is more often a clinical diagnosis. When onychorrhexis is associated with a dermatologic disorder, biopsy of the nail matrix reveals typical histology for that disorder (eg, lichen planus, sarcoidosis, amyloidosis). In one study 23, nail bed biopsy of age-related onychorrhexis revealed lichen planus–like changes including hyperkeratosis, hypergranulosis, and hydropic degeneration of the basal cell layer with necrotic keratinocytes. Epidermal thickening, papillomatous change, and bending of rete ridges was also noted.
Onychorrhexis treatment
Onychorrhexis treatment involves the correct diagnosis and treating the underlying cause. In secondary nail brittleness cases, treatment includes the cure of the dermatological/systemic condition, avoidance of traumas and allergens/irritants, limiting contact with water and detergents, and regular use of emollients 4. However, most patients consulting for nail brittleness have an idiopathic nail fragility. Oral supplementation with vitamins (especially biotin, also known as vitamin B7), trace elements, and amino acids (especially cysteine) have been reported useful in improving idiopathic nail fragility 24. However, these studies were small, not well controlled, and one study was retrospective, survey based.
Biotin or vitamin B7 is a water-soluble vitamin contained in several foods such as cereals, walnuts, peanuts, milk, and egg yolks. Vitamin B7 is also synthetized by intestinal bacteria. Biotin:
- Takes part in keratin biosynthesis and intercellular cement holding keratinocytes together, acting as the prosthetic group of several essential enzymes;
- Improves the ultrastructure of the nail plate (onychocytes show more regular arrangements and distribution) and its resistance to tension.
Several studies have demonstrated, both with clinical and electron microscopy examinations 25, an improvement of firmness and hardness of the fingernails of patients receiving biotin supplementation 26. A dosage of 5–10 mg a day for 3–6 months is usually recommended.
High biotin intake (more than 10 mg per day) can cause falsely high or falsely low laboratory test results 27. Troponins, thyroid, prolactin and pregnancy tests are some of the most frequently altered 28. The presence of biotin can interfere with tests that use biotin–streptavidin technology. The interaction between biotin and streptavidin is used as the basis for many biotin-based immunoassays, and these immunoassays are vulnerable to interference when they are used to analyze a sample that contains biotin. The FDA warning on this topic emphasizes that physicians should obtain an updated list of medications, including vitamins and supplements, and doses, at each visit 27. This is particularly important as patients are not aware of the risks associated with biotin 29.
A combination of an arginine silicate complex and magnesium biotinate (a novel well-absorbed biotin salt) was demonstrated to increase nail growth 30. However, the studies were small and two of them lacked a control group 31.
Iron supplementation (plus vitamin C) may be very effective when ferritin levels are below 10 ng/ml. However, studies that correlate iron deficit with brittle nails are rarely reported 32.
Primary and secondary zinc deficiency is a cause of nail fragility. Prolonged treatment with zinc 20–30 mg/day seems to be effective in improving brittle nails 32.
In a recent randomized trial, a biomineral formulation containing amino acids (l-cystine, l-arginine, glutamic acid), vitamins (C, E, B6 and biotin) and minerals (zinc, iron and copper) proved to be well tolerated and effective in strengthening and smoothing fingernails in subjects with onychoschizia after 3 months of treatment 33. No data about dosage of the single elements is provided in the article 33.
In an open-label single-center trial, supplementation with “bioactive collagen peptides” was shown to be very effective in patients with brittle nails after 24 weeks of treatment. In this study it was reported that nail growth rate increased by 12% and the frequency of broken nails decreased by 42% 34.
Nail moisturizers are useful in patients with brittle nails. They may contain occlusive material (petrolatum or lanolin) and humectants (glycerin, propylene glycol and proteins). Alpha-hydroxy acids and urea may also be added to increase the water-binding capacity of the nail plate.
Several lacquers are commercially available to restructure nails affected by fragility. These products are known as nail hardeners, nail strengtheners, and fortifying nail builders, and may contain silicon. A new water-soluble nail strengthener specially formulated with a combination of active ingredients (silanediol salicylate and Pistacia lentiscus gum) that increase the quantity and quality of silicon and keratin in the nails. It contains cationic hyaluronic acid that adheres to the surface and deeply moisturizes the nails and cuticles. This combination of ingredients (patent pending) helps the natural process of nail growth. The safety and efficacy are supported by a 6-month clinical study 35.
A recent study observed that hydroxypropyl chitosan nail lacquer when applied on the nails is useful to protect them against physical injuries, improving the nail structure 36. The authors correlate the efficacy of hydroxypropyl chitosan to the high affinity with keratin that is secondary to water solubility without pH correction 36.
A second lacquer composed of 16% polyureaurethane could be used in brittle nails to create a flexible waterproof barrier to environmental hazards 37. The once daily application of both lacquers is recommended.
In a randomized controlled pilot study, the efficacy of topical cyclosporine emulsion versus emulsion (vehicle) alone have been compared. Cyclosporine emulsion and also emulsion alone appeared to improve signs of brittle nails. Limitations of this study were the small sample size and the method for detection of efficacy 38.
These nail lacquers could increase the cosmetic outcomes of brittle nails, but further data are necessary to prove their true efficacy 39.
In recalcitrant fragility, nail wrapping limited to the distal portion of the nail may afford protection and camouflage. The procedure of nail wrapping consists of the application of layers of fibrous substances made of tissue paper, silk, linen, plastic film, or fiberglass on the distal edge of the nail plate to strengthen or repair its free edge. This same method is performed in artificial nails and sculptured nails and can considerably improve brittle nails cosmetically. However, artificial nails could themselves be responsible for fragility because of the materials and procedures used to apply them 40.
Good advice is to wear cotton gloves under vinyl gloves for wet work and heavy cotton gloves for dry work.
Onychorrhexis prognosis
Onychorrhexis is not considered life-threatening. However, it can have a negative impact on quality of life and may impede with one’s daily activities and occupational responsibilities 41. Idiopathic onychorrhexis is typically milder than onychorrhexis associated with inflammatory nail matrix diseases, such as lichen planus 42. It can take a significant amount of time for patients to notice major clinical improvement, especially given the slow growth of the nail plate (range, 0.5-1.2 mm/week) and that many systemic conditions known to contribute to onychorrhexis are considered chronic 43.
References- Chessa MA, Iorizzo M, Richert B, et al. Pathogenesis, Clinical Signs and Treatment Recommendations in Brittle Nails: A Review [published correction appears in Dermatol Ther (Heidelb). 2020 Jan 22;:]. Dermatol Ther (Heidelb). 2020;10(1):15-27. doi:10.1007/s13555-019-00338-x https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6994568
- Singh G, Haneef NS, Uday A. Nail changes and disorders among the elderly. Indian J Dermatol Venereol Leprol. 2005;71(6):386–392.
- van de Kerkhof PC, Pasch MC, Scher RK, Kerscher M, Gieler U, Haneke E, et al. Brittle nail syndrome: a pathogenesis-based approach with a proposed grading system. J Am Acad Dermatol. 2005 Oct. 53 (4):644-51.
- Brosche T, Dressler A, Platt D. Age-associated changes in integral cholesterol and cholesterol sulfate concentrations in human scalp hair and fingernail clippings. Aging Clin Exp Res. 2001;13:131–138. doi: 10.1007/BF03351535
- Scher RK, Bodian AB. Brittle nails. Semin Dermatol. 1991;10:21–25.
- Duarte AF, Correia O, Baran R. Nail plate cohesion seems to be water independent. Int J Dermatol. 2009;48:193–195. doi: 10.1111/j.1365-4632.2009.03978.x
- Van de Kerkhof PC, Pasch MC, Scher RK, et al. Brittle nail syndrome: a pathogenesis-based approach with a proposed grading system. J Am Acad Dermatol. 2005;53:644–651. doi: 10.1016/j.jaad.2004.09.002
- Bardazzi F, Lambertini M, Chessa MA, Magnano M, Patrizi A, Piraccini BM. Nail involvement as a negative prognostic factor in biological therapy for psoriasis: a retrospective study. J Eur Acad Dermatol Venereol. 2017;31:843–846. doi: 10.1111/jdv.13979
- Tosti A, Piraccini BM, Cameli N. Nail changes in lichen planus may resemble those of yellow nail syndrome. Br J Dermatol. 2000;142:848–849. doi: 10.1046/j.1365-2133.2000.03460.x
- Chessa MA, Alessandrini A, Starace M, et al. Erosive lichen planus: beyond the nails. J Eur Acad Dermatol Venereol. 2019;33:e97–e99. doi: 10.1111/jdv.15319
- Kim M, Jung HY, Eun YS, Cho BK, Park HJ. Nail lichen striatus: report of seven cases and review of the literature. Int J Dermatol. 2015;54:1255–1260. doi: 10.1111/ijd.12643
- Piraccini BM, Balestri R, Starace M, Rech G. Nail digital dermoscopy (onychoscopy) in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2013;27:509–513. doi: 10.1111/j.1468-3083.2011.04323.x
- Fustà X, Morgado-Carrasco D, Mascaró JM., Jr Image gallery: nail involvement in syphilis: the great forgotten. Br J Dermatol. 2017;177:e158. doi: 10.1111/bjd.15819
- Samman PD, Fenton DA. Samman’s the nails in disease. In: 5th ed Oxford. Boston: Butterworth-Heinemann; 1995.
- Taguchi T. Brittle nails and hair loss in hypothyroidism. N Engl J Med. 2018;379:1363. doi: 10.1056/NEJMicm1801633
- Geyer AS, Onumah N, Uyttendaele H, Scher RK. Modulation of linear nail growth to treat diseases of the nail. J Am Acad Dermatol. 2004;50:229–234. doi: 10.1016/j.jaad.2003.07.011
- Batory M, Namieciński P, Rotsztejn H. Evaluation of structural damage and pH of nail plates of hands after applying different methods of decorating. Int J Dermatol. 2019;58:311–318. doi: 10.1111/ijd.14198
- Zaias N. The nail in health and disease. 2nd edn. Mc graw Hill Professional, 1992.
- Weistenhöfer W, Uter W, Drexler H. Protection during production: problems due to prevention? Nail and skin condition after prolonged wearing of occlusive gloves. J Toxicol Environ Health A. 2017;80:396–404. doi: 10.1080/10937404.2017.1304741
- Dimitris R, Ralph D. Management of simple brittle nails. Dermatol Ther. 2012 Nov-Dec. 25 (6):569-73.
- Iorizzo M. Tips to treat the 5 most common nail disorders: brittle nails, onycholysis, paronychia, psoriasis, onychomycosis. Dermatol Clin. 2015 Apr. 33 (2):175-83.
- Iorizzo M, Pazzaglia M, M Piraccini B, Tullo S, Tosti A. Brittle nails. J Cosmet Dermatol. 2004 Jul. 3 (3):138-44.
- El-Domyati M, Abdel-Wahab H, Abdel-Azim E. Nail changes and disorders in elderly Egyptians. J Cosmet Dermatol. 2014 Dec. 13 (4):269-76.
- Almohanna HM, Ahmed AA, Tsatalis JP, Tosti A. The role of vitamins and minerals in hair loss: a review. Dermatol Ther (Heidelb). 2019;9:51–70. doi: 10.1007/s13555-018-0278-6
- Kitamori K, Kobayashi M, Akamatsu H, et al. Weakness in intercellular association of keratinocytes in severely brittle nails. Arch Histol Cytol. 2006;69:323–328. doi: 10.1679/aohc.69.323
- Hochman LG, Scher RK, Meyerson MS. Brittle nails: response to daily biotin supplementation. Cutis. 1993;51:303–305.
- Administration USFaD. Biotin (vitamin B7): Safety communication – may interfere 154 with lab tests. In: 11/28/2017, ed.
- Maddy AJ, Tosti A. What’s new in nail disorders. Dermatol Clin. 2019;37:143–147. doi: 10.1016/j.det.2018.12.004
- John JJ, Cooley V, Lipner SR. Assessment of biotin supplementation among patients in an outpatient dermatology clinic. J Am Acad Dermatol. 2019;81:620–621. doi: 10.1016/j.jaad.2018.12.045
- James K, Sara PO, Sarah S et al. The effect of a combination of an arginine silicate complex and magnesium biotinate on hair and nail growth in rats (P06-026-19). Curr Dev Nutr. 2019;3:nzz031.P06-026-19
- Lipner SR, Scher RK. Biotin for the treatment of nail disease: what is the evidence? J Dermatol Treat. 2018;29:411–414. doi: 10.1080/09546634.2017.1395799
- Di Baise M, Tarleton SM. Hair, nails, and skin: differentiating cutaneous manifestations of micronutrient deficiency. Nutr Clin Pract. 2019;34:490–503. doi: 10.1002/ncp.10321
- Sparavigna A, Tenconi B, La Penna L. Efficacy and tolerability of a biomineral formulation for treatment of onychoschizia: a randomized trial. Clin Cosmet Investig Dermatol. 2019;13(12):355–362. doi: 10.2147/CCID.S187305
- Hexsel D, Zague V, Schunck M, Siega C, Camozzato FO, Oesser S. Oral supplementation with specific bioactive collagen peptides improves nail growth and reduces symptoms of brittle nails. J Cosmet Dermatol. 2017;16:520–526. doi: 10.1111/jocd.12393
- Starace M, Alessandrini A, Bruni F, Brandi N, Piraccini BM. An open clinical investigation on clinically and dermoscopically visible effects of application of a topical product for 6 months on brittle nails and weak nails with rough surface and/or tendency to break. Poster presented at the 24th Word Congress of Dermatology, Milan, 10–15 June 2019.
- Sparavigna A, Caserini M, Tenconi B, et al. Effects of a novel nail lacquer based on hydroxypropyl-chitosan (HPCH) in subjects with fingernail onychoschizia. J Dermatol Clin Res. 2014;2:1013–1018.
- Iorizzo M. Tips to treat the 5 most common nail disorders: brittle nails, onycholysis, paronychia, psoriasis, onychomycosis. Dermatol Clin. 2015;33:175–183. doi: 10.1016/j.det.2014.12.001
- Mackay-Wiggan J, Marji J, Walt JG, et al. Topical cyclosporine versus emulsion vehicle for the treatment of brittle nails: a randomized controlled pilot study. J Drugs Dermatol. 2014;13:1232–1239.
- Iorizzo M, Piraccini BM, Tosti A. Nail cosmetics in nail disorders. J Cosmet Dermatol. 2007;6:53–58. doi: 10.1111/j.1473-2165.2007.00290.x
- Dahdah MJ, Scher RK. Nail diseases related to nail cosmetics. Dermatol Clin. 2006;24(233–9):vii.
- Shemer A, Daniel CR 3rd. Common nail disorders. Clin Dermatol. 2013 Sep-Oct. 31 (5):578-86.
- Maddy AJ, Tosti A. Hair and nail diseases in the mature patient. Clin Dermatol. 2018 Mar – Apr. 36 (2):159-166.
- Fenton DA, Samman PD, eds. Samman’s the Nails in Disease. 5th ed. Oxford; 1994.