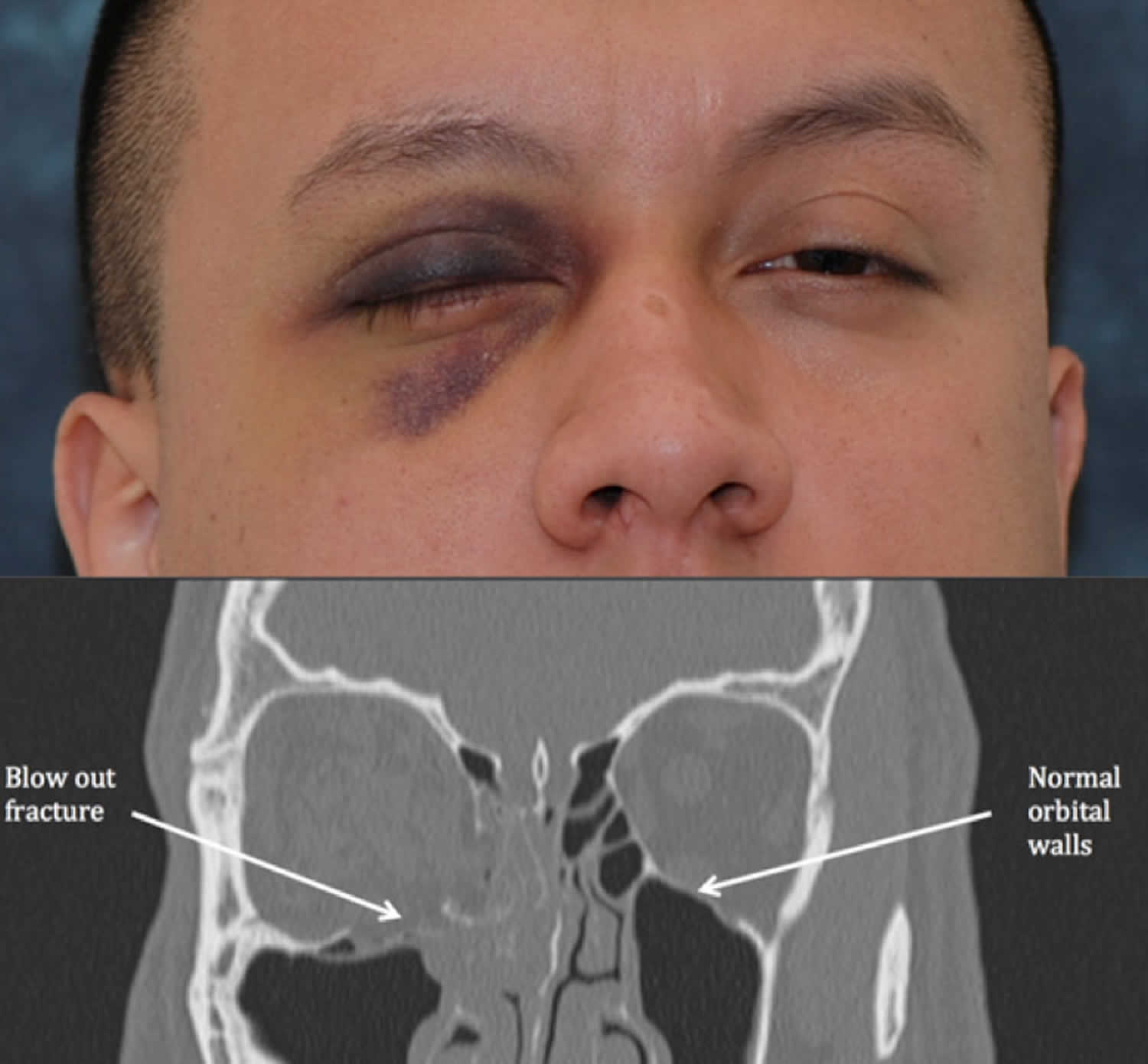
Orbital floor fracture
Orbital floor fracture also known as “blowout fracture” of the orbit (eye socket). Orbital floor fractures may result when a blunt object, which is of equal or greater diameter than the orbital aperture, strikes the eye or on the cheek 1. Getting hit with a baseball or a fist often causes a orbital blowout fracture. The globe usually does not rupture, and the resultant force is transmitted throughout the orbit (eye socket) causing a fracture of the orbital floor. Orbital floor fracture is common, it is estimated that about 10% of all facial fractures are isolated orbital wall fractures (the majority of these being the orbital floor), and that 30-40% of all facial fractures involve the orbit.
Orbital fractures are more common in males than in females and most often occur in men, ages 21 to 30 years of age 2.
The anatomy of the orbital floor predisposes it to fracture. The inferior orbital neurovascular bundle (comprising the infraorbital nerve and artery) courses within the bony floor of the orbit; the roof of this infraorbital canal is only 0.23mm thick, and the bone of the posterior medial orbital floor averages 0.37 mm thick. By contrast, the bone of the lateral portion of the orbital floor averages 1.25 mm thick, over 5 times the thickness of the bone over the neurovascular bundle. As one might suspect, it is this very thin area of the orbital floor overlying the neurovascular bundle where isolated orbital floor fractures invariably occur.
Fractures of the orbital floor and the medial orbital wall are the most common fractured site 3. Falls, motor vehicle accidents, and assaults account for most midfacial fractures 4.
Orbital floor fracture signs and symptoms can be quite varied, ranging from asymptomatic with minimal bruising and swelling to double vision (diplopia), enophthalmos (posterior displacement of the eyeball within the orbit), hypo-ophthalmia (ie, hypoglobus), and hypoesthesia of the cheek and upper gum on the affected side. Treatment is titrated to the degree of injury 5.
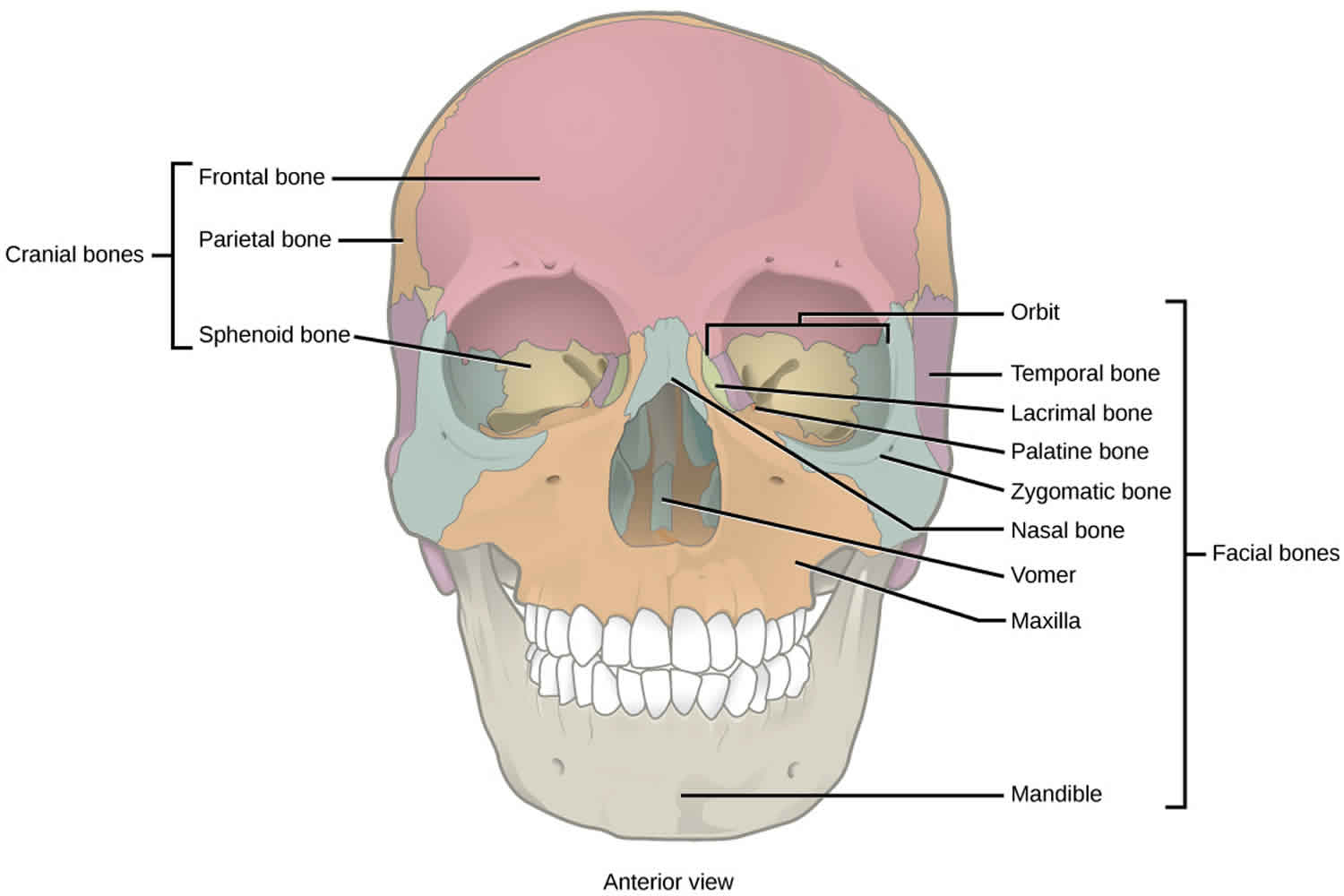
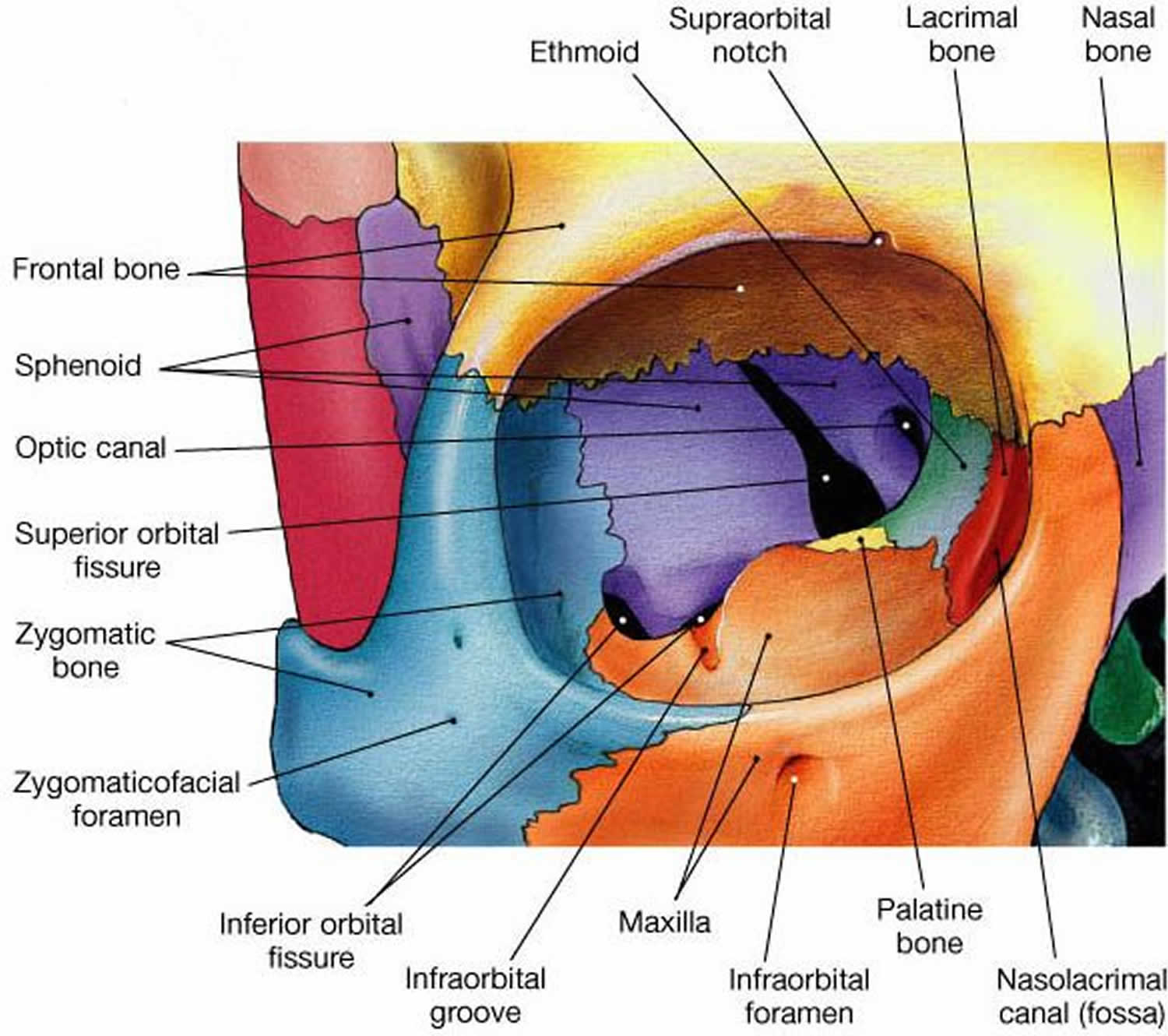
Eye socket (orbit) anatomy
The bony orbit is composed of 7 bones of varying thickness. The frontal bone forms the supraorbital rim and orbital roof. The medial surface consists of the maxillary, lamina papyracea of the ethmoid bone and the lacrimal bone, whereas the greater wing of the sphenoid and the zygoma create the lateral margin. The sphenoid bone forms the posterior wall and houses the orbital canal. Inferiorly, the floor and infraorbital rim are formed by the zygoma and maxilla. This portion is very thin; therefore, it is the most common site of fracture within the orbit. Located around the globe of the eye and attached to it are 6 extraocular muscles; the 4 rectus muscles and the superior and inferior oblique muscles. The fat and connective tissue around the globe help to reduce the pressure exerted by the extraocular muscles 6. Fracture of the orbital floor, also known as a blow-out fracture, can result in entrapment of the inferior rectus muscle, limiting upward gaze.
Lateral to the orbital canal lies the superior orbital fissure housing cranial nerves III, IV, V, and VI. The zygomatic bone forms the lateral wall. Superior and inferior borders are the frontal and maxillary bone.
The adult orbital floor is composed of the maxillary, zygomatic, and palatine bones. The orbital floor is the shortest of all the walls; it does not reach the orbital apex, measures 35-40 mm, and terminates at the posterior edge of the maxillary sinus. The infraorbital groove, canal, and foramen are contiguous and tunnel through the maxilla, encasing the maxillary branch of the trigeminal nerve. The maxillary branch of cranial nerve V exits as the infraorbital nerve, providing sensory innervations to the ipsilateral orbital floor, mid face, and posterior upper gingival. The infraorbital artery, a branch of the maxillary artery, and the infraorbital vein also are found within the infraorbital groove, flanking the infraorbital nerve and exiting the infraorbital canal.
Figure 1. Orbit anatomy
Orbital floor fracture causes
A orbital blowout fracture is an isolated fracture of the orbital walls without compromise of the orbital rims 7. The common mechanisms are falls, high-velocity ball-related sports, traffic accidents, and interpersonal violence.
Pure orbital floor fractures, referred to as isolated floor fractures, result from impact injury to the globe and upper eyelid. The object is usually large enough not to perforate the globe and small enough not to result in fracture of the orbital rim.
The trauma mechanism is a blunt, directed force which may be aimed at the eye, without a pressure component toward the eye rim leading to an increase of pressure inside the orbit with a fracture of the bony structures (hydraulic mechanism). Alternatively, the trauma may be directed towards the orbital rim, which then leads to a bending of the orbital walls with consequent fracturing (buckling mechanism) 8.
The mechanism of entrapment is more frequently referred to as a trapdoor in children, as opposed to the “blowout or punched-out” fracture present in adults.
Orbital floor fracture pathophysiology
Orbital floor fractures are secondary to a sudden increase in intraorbital hydraulic pressure. A high-velocity object that impacts the globe and upper eyelid transmits kinetic energy to the periocular structures. This energy results in pressure with a downward and medial vector usually targeting the infraorbital groove. Most fractures occur in the posterior medial region that is comprised of the thinnest bones 9.
Another proposed mechanism that is less favored describes buckling of the orbital floor without displacement of orbital contents following high-velocity trauma.
Although most pure orbital fractures affect the region medial to the infraorbital groove, any fracture type, size, or geometry is possible.
Orbital floor fracture symptoms
After facial trauma, patients may describe decreased visual acuity, blepharoptosis, binocular vertical or oblique diplopia (especially in upgaze), and ipsilateral hypesthesia, dysesthesia, or hyperalgesia in the distribution of the infraorbital nerve. Patients with an orbital floor fracture may present with a tropia (misalignment of the eyes) in upgaze and/or downgaze, with the affected side demonstrating limitation of full movement. Occasionally, patients may have diplopia in primary gaze and even in horizontal gaze, but these presentations are much less common. In addition, patients may complain of nosebleeds (epistaxis) and eyelid swelling following nose blowing.
Enophthalmos (posterior displacement of the eyeball within the orbit due to changes in the volume of the orbit) of the affected side may be present initially, but more commonly develops days to weeks after the injury as orbital swelling subsides.
Periorbital ecchymosis and edema accompanied by pain are obvious external signs and symptoms, respectively. This swelling can restrict ocular motility, giving the impression of soft tissue or inferior rectus entrapment. Retrobulbar or peribulbar hemorrhage may be heralded by bulging eyes (proptosis). A bony step-off of the orbital rim and point tenderness are possible during palpation.
Examination of the globe is essential, albeit difficult because of soft tissue edema. Desmarres retractors may be helpful to spread edematous eyelids
Pupillary dysfunction coupled with decreased visual acuity should alert one to the possibility of a traumatic or compressive optic neuropathy.
Ocular misalignment, hypotropia or hypertropia, and limitation of elevation ipsilateral to the fracture are possible. Forced duction testing can differentiate entrapment versus neuromyogenic etiologies of muscle underaction.
The supratarsal crease may deepen, along with narrowing of the palpebral fissure stemming from enophthalmos or fibrous tissue contraction. Although the palpebral fissure may in fact narrow, the geometric shape is preserved, since dehiscence or disruption of the canthal tendons is uncommon.
A retrospective study by Bartoli et al 10 of 301 orbital floor fractures found the most common symptom to be hypesthesia extending through the region of the maxillary nerve (32.9% of patients). Diplopia was also common, being found in 20.2% of patients, while enophthalmos and reduction of extraocular movement occurred in 2.3% and 1.7% of patients, respectively 10.
A study by Boffano et al 11 of patients with blow-out fractures indicated that the characteristics of diplopia vary according to the position of the fracture. In the report, in which just over 50% of 447 patients with pure blow-out fractures presented with evidence of diplopia, statistically significant associations were found between orbital floor fractures and diplopia on eye elevation, and between medial wall fractures and horizontal diplopia. The investigators suggested, therefore, that the form of diplopia that a patient presents with may offer clues to the type of orbital fracture sustained 11.
Wilkins and Havins 12 reported a 30% incidence of a ruptured globe in conjunction with orbital fractures, supporting the notion that a thorough and complete ophthalmic examination is needed.
Orbital floor fracture diagnosis
Almost all patients will report recent trauma to the eye or the midface prior to the occurrence of the fracture. In cases of occult fractures discovered incidentally or years after the injury, the patient may have no recollection of the actual traumatic incident.
In the acute setting of midfacial trauma, a complete ophthalmologic examination is vital; in the event of a ruptured globe, retinal detachment, intraocular bleed, or other sight threatening complication, all orbital intervention should be postponed until the eye is stabilized. When an orbital floor fracture is suspected, the presence or absence of enophthalmos should be noted and the measurement of extraocular motility is vital.
Patients who have diplopia and/or pain with vertical movements of the eyes after blunt midfacial trauma should be suspected to have an orbital floor fracture; however, the diagnosis can only be made radiologically. Forced ductions to manually rotate the globe can sometimes be performed in the clinic or emergency room setting, and may indicate restriction of movement.
The following assessments are characteristic of orbital floor fractures and mandate further imaging:
- Diplopia (on upward gaze)
- Limitation of upward gaze
- Trigeminal function assessment: The infraorbital nerve runs along the floor of the orbit. decreased sensation over the inferior orbital rim, extending to the edge of the nose and ipsilateral upper lip.
- Tenderness, or step-offs at the infraorbital rim
- Subcutaneous emphysema (indicates fracture of the maxillary sinus)
- Oculomotor function: Entrapment of the inferior rectus muscle; often occurs between fragments of the lower orbit and is the cause of diplopia
- Pupillary light reflex: An absent reflex can show damage to the afferent or efferent nerve system
- Gross visual acuity
- Position of the globe: A dislocated fracture can lead to enophthalmos and swelling behind the globe, to exophthalmos
- Chemosis and sub-conjunctival hemorrhage 3
Diagnostic procedures
Computed tomography (CT) is the imaging modality of choice if a blowout fracture is suspected after blunt orbital trauma. Some symptoms include double vision, pain with eye movements, and restriction of extraocular muscle movements. A CT scan often reveals herniation of orbital fat or the inferior rectus muscle, into the maxillary sinus. Such a scan can also detect occult tears and retained foreign bodies if any are present.
Patients suspected of suffering an orbital floor fracture should undergo thin cut (1.0 – 1.5mm) axial CT scans of the orbit with coronal reconstruction. (Thin cut coronal reconstructions are actually preferred to direct coronal images as they avoid artifact from dental amalgam.) In the great majority of floor fractures, a fracture can be localized above, or just medial to, the course of the infraorbital nerve. A fracture in this location leads either to a “trap door” displacement of the orbital floor, or, if a second fracture is present at the junction of the floor and medial wall, to a completely depressed, separate bony fragment. These deformities are best appreciated on coronal images. Herniation of the inferior rectus muscle into the maxillary sinus through the orbital defect does not predict clinical dysmotility. Many patients with radiologic evidence of inferior rectus herniation do not have clinical entrapment, while many patients in whom orbital fat herniates into the defect, but where the inferior rectus muscle remains in the orbit, have severe dysmotility. The extraocular muscles are connected to each other and to the orbital fat through a complicated interconnecting web of septa, such that even if fat alone is incorporated into the fracture, profound dysmotility may result. Entrapment is a purely clinical diagnosis, not a radiologic one.
Orbital floor fracture treatment
Immediately after an orbital floor fracture, the affected eye may have impaired motility, resulting in double vision. The eye may be proptotic or enophthalmic, depending on the amount of edema (causing proptosis) and the size of the fracture (leading to enophthalmos). As the acute swelling resolves, double vision will generally either stay the same or improve, while the enophthalmos will either remain the same or worsen. Thus while diplopia may be an initial concern immediately after the injury, it may resolve over time on its own without surgical intervention.
Patients with dysmotility may benefit from a short (three day) course of steroids (0.75 – 1.0 mg/kg per day of prednisone) in the acute setting if there are no contraindications. Such treatment may help periorbital and extraocular muscle edema to subside more quickly to determine if the patient’s dysmotility is transient or if surgery is necessary. Antibiotics may be prescribed in the acute setting. Patients should be informed that nose-blowing could lead to orbital or soft tissue emphysema and is discouraged for 4-6 weeks after the injury.
Surgical repair of the fracture is indicated when enophthalmos is troublesome to the patient, or when diplopia interferes with the patient’s activities. In cases of severe entrapment—for example, where there is a complete lack of supraduction or fairly severe pain on eye movement, or hemodynamic instability—urgent intervention is warranted. However, since cases with less severe dysmotility often resolve without intervention, it is often prudent to wait at least 10-14 days to repair an orbital floor fracture, especially if improvement in motility is seen in the first week after the injury. If disabling diplopia is still present two to three weeks after the injury without signs of improving motility, surgical repair is warranted. While motility is improving, especially if documented with a progressively smaller prismatic deviation over time, surgery may be delayed to determine if the diplopia will completely resolve on its own, or at least resolve to the patient’s satisfaction. Usually, by three weeks after the injury, a decision regarding surgery can be made with respect to disabling diplopia. There is no compelling evidence that orbital fracture surgery should be performed within a two week “window” following the injury, and many patients will continue to note improvement in diplopia even after the two week window, thus avoiding surgery.
Surgery to prevent enophthalmos should probably be discouraged, since it is impossible to predict who will develop enophthalmos and how enophthalmos will affect the patient (i.e., the patient may not be bothered by it). Furthermore, studies support the notion that enophthalmos is corrected equally well when addressed several weeks after an injury when compared to repair within the “two week window.” The risks of surgery should also be discussed with the patient, including implant infection or reaction, hyperglobus, diplopia, hemorrhage, infection, injury to the globe or optic nerve, and loss of vision.
Medical therapy
Medical treatment is warranted for patients for whom surgery is not indicated. This may include patients who present without significant enophthalmos (2 mm or more), a lack of marked hypo-ophthalmus, absence of an entrapped muscle or tissue, a fracture less than 50% of the floor, or a lack of diplopia.
Patients with dysmotility may benefit from a short (three day) course of steroids (0.75 – 1.0 mg/kg per day of prednisone) in the acute setting if there are no contraindications. Such treatment may help periorbital and extraocular muscle edema to subside more quickly to determine if the patient’s dysmotility is transient or if surgery is necessary. Antibiotics may be prescribed in the acute setting due to the disruption of the integrity of the orbit in communication with the maxillary sinus.
Patients should be informed that nose-blowing could lead to orbital or soft tissue emphysema and is discouraged for 4-6 weeks after the injury. Nasal decongestants can be used if not contraindicated.
Orbital floor fracture surgery
The timing and requirements for surgical repair of pure orbital floor fractures has been long debated. Most literature supports a 2-week window for repair to prevent fibrosis, resulting tissue contracture and entrapment. The authors often wait several days to allow dissipation of edema and hemorrhage in order to better assess enophthalmos and extraocular muscle function. In the event of tense inferior rectus incarceration, more immediate action is taken.
Pediatric patients with an orbital floor fracture, nausea, vomiting, and extraocular muscle dysfunction experienced rapid improvement of these signs and symptoms and less risk of residual extraocular muscle dysfunction when the fracture was repaired within 7 days 13.
A pure orbital floor fracture involving more than 50% of the floor, with orbital tissue prolapse, usually results in significant enophthalmos (>2 mm). These 2 findings indicate the need for timely repair.
Diplopia within 30° of primary gaze, positive forced-duction testing, and CT scan confirmation of a fracture warrant an early repair. Trapdoor or anteroposterior fractures can have clinical findings that are out of proportion to radiologic studies.
Although diplopia within 30° of primary gaze, extraocular muscle entrapment, and enophthalmos greater than 2 mm are discussed in the context of large floor fractures, each on its own can be an indication for repair.
Infraorbital nerve dysfunction occurs and is often the only complaint following pure orbital floor fracture. This sensory disturbance traditionally has not been an indication for repair. Some authors have reported improvement of this neuropathy following repair and nerve decompression 14.
All orbital floor fractures should be repaired via a transconjunctival approach. While a lateral canthotomy and inferior cantholysis are often advocated, they are unnecessary and can be omitted with no loss of exposure.
Transconjunctival approach
A conjunctival incision is made with monopolar cautery (with a corneal protector in place) across the length of the eyelid just below the base of the tarsus. Once the incision is complete, two 5-0 silk traction sutures are placed in the free conjunctival edge, pulled superiorly, and clamped to the head drape over the forehead, pulling a sheet of conjunctiva superiorly to cover the cornea; this maneuver serves to protect the cornea as well as to provide retraction. Blunt dissection can be performed in the eyelid atraumatically in the plane between the orbital septum and orbicularis muscle with a cotton tipped applicator down to the orbital rim, while the anterior lamella is simultaneously retracted with a DeMarres retractor. The perisoteum is opened with monopolar cautery and lifted off of the orbital floor.
In order to perform a successful repair, all of the herniated orbital tissue must be reposited back into the orbit. When possible, the infraorbital neurovascular bundle, inferior rectus, and inferior oblique should be visualized as they are important surgical landmarks. A plane should be developed between the orbital tissue (above the plane of dissection) and the infraorbital nerve and the exposed sinus mucosa (below the plane of dissection). Both blunt and sharp dissection may need to be employed. It is important to completely dissect the entire fracture site, i.e., 360 degrees of bony edge should be visualized around the fracture site. An orbital implant should be fashioned in the shape of a “guitar pick” with the narrow-width portion placed posteriorly, and if porous, can be soaked in an antibiotic solution such as a mixture of Bacitracin and Polymixin. The orbital implant should then be placed so that it rests on the posterior lip of the fracture, thereby covering the entire defect, without incarcerating orbital tissue beneath the implant. The implant may be fixated by a variety of methods, depending on the surgeon’s preference. Following the placement of the implant, a forced duction test can be performed to insure that no tissue is trapped beneath the implant. In some cases where the inferior rectus muscle is swollen or hemorrhagic, a forced duction test may still reveal resistance despite a properly performed surgical repair; in such cases, diplopia may still resolve over time but there is a greater likelihood that some level of diplopia will persist due to intrinsic damage to the inferior rectus muscle.
One technique that may be useful in implant fixation is to use a few drops of a cyanoacrylate derivative (a “superglue” such as Iso-DentTM) just beneath the leading edge of the implant to cause adherence of the implant to the (dry) bone beneath it. A 1 cc tuberculin syringe with a 26 gauge needle is ideal for this purpose. This technique is especially valuable with porous implants that will eventually fibrose into place biologically but may need 3-4 weeks of stabilization postoperatively prior to tissue ingrowth.
Intraoperatively, steroids can be given intravenously (20 mg of Decadron), followed by a three to five day course of oral prednisone (0.75 – 1.0 mg/kg per day) to limit orbital swelling.
It is helpful to remind patients preoperatively that even with a perfect repair, residual/permanent diplopia can still result if the inferior rectus is damaged. Further, even though herniated tissue is reposited back into the orbit, fat atrophy may occur and enophthalmos is therefore typically improved but not always completely eliminated. Prior to surgery, patients should also be reassured that recovery of extraocular muscle function will not be immediate, and that several weeks (and even a few months) may be required for full recovery to occur. Usually 6-9 months should elapse after surgery before assuming that no further recovery will be observed, and before strabismus surgery, if indicated, should be performed.
Postoperatively, if motility is not improving or improving very slowly, a CT scan can be performed to check the placement of the implant. Radiologically visible implants hold an advantage in this regard, and a CT image showing proper implant placement can reassure the patient (and surgeon) that no further intervention is warranted.
Cutaneous approach
The cutaneous approach commences with a skin-muscle flap elevation via an incision 2-3 mm below the lower lid margin. Carry this dissection anterior to the orbital septum until the orbital rim is exposed.
Incise the periosteum and release it from its bony attachments as described in the transconjunctival approach. Of note is the downward sloping of the floor immediately posterior to the rim, which can result in breach of the septum during periosteal dissection.
Transantral approach
A transantral approach allows access to the orbital floor via the maxillary sinus. This approach may be especially useful when repairing a floor fracture of the trap door variety.
Achieve exposure of the incision site with upper labial retraction exposing the buccal-gingival sulcus.
Create a horizontal incision just inferior to the buccal-gingival sulcus so that a wide mucosal band is present. This wide band allows for imbrication of the wound, avoiding oral-antral fistulization.
Use a periosteal elevator to strip the anterior maxillary wall of periosteum. The proximity of the infraorbital foramen should be kept in mind to minimize the risk of insult to the neurovascular bundle.
Create a Caldwell-Luc antrostomy with an osteotome and mallet, followed by rongeurs to increase the diameter of the antrostomy, providing access to the orbital floor, medial wall, and ethmoid sinus complex.
Strip the mucosa from the maxillary antrum and cauterize the remnants.
Following repair of the fracture, attention to hemostasis is followed by closing the buccal-gingival mucosa with fast-absorbing suture material.
This approach results in inferior orbital floor exposure and is not favored for floor fracture repair.
Some authors have advocated an endoscopic transantral approach for improved visualization of fractures and to eliminate the need for eyelid incisions 15.
Other approaches
Tessier described vertical osteotomy of an intact orbital rim for exposure of the orbital floor. This osteotomy is essentially 2 vertical osteotomies on either side of the infraorbital foramen conjoined by a horizontal osteotomy. Two osteotomies of the orbital floor originating at the inferior rim and extending past the infraorbital groove origins are created, allowing for removal of this segment, which can be replaced at the conclusion of surgery.
Endoscopic-assisted approaches via a transmaxillary and transnasal route have been described 16. Suzuki et al 17 described a modified transnasal endoscopic approach designed to address problems with repairing anterior and lateral orbital floor fractures that have been encountered with previous transnasal endoscopic techniques. The modified approach involves going through the anterior space to the nasolacrimal duct, with surgeons removing the medial maxillary bone, shifting the lateral wall of the nose medially to provide greater access to the maxillary sinus, carefully removing bone fragments entrapping the orbital content, and correcting the periorbita (orbital periosteum).
Implants
Several types of implants are available for reconstructive use. The ideal implant should be easy to insert and manipulate, inert, not prone to infection or extrusion, easily anchored to surrounding structures, and reasonably priced. It should not rouse fibrous tissue formation. Most orbital floor defects can be repaired with synthetic implants composed of porous polyethylene, silicone, metallic rigid miniplates, Vicryl mesh, resorbable materials, or metallic mesh. Autogenous bone from the maxillary wall or the calvaria can be used, as can nasal septum or conchal cartilage. Each material has advantages and disadvantages. The surgeon should have a certain comfort level and familiarity with his or her choice of material.
A study by Holtmann et al 18 found better results with resorbable 0.15-mm diameter polydioxanone foil than with titanium mesh in the repair of median orbital floor defects of 250-300 mm2 in size. Using the foil, diplopia was reduced from 16% of patients preoperatively to 4.9% postoperatively. Fifty percent of patients who underwent reconstruction with titanium mesh reported foreign body sensations and a cold feeling in the operative region during weather changes, compared with just 4.7% of patients reconstructed with the 0.15-mm foil.
A retrospective study by Kronig et al 19 indicated that good functional and aesthetic results can be achieved 1 year after the repair of pure orbital floor fractures with autogenous bone. In patients with both orbital floor and medial wall fractures, reconstruction of both walls resulted in an absence of enophthalmos, while in those in whom the medial wall was not reconstructed, 29% still had enophthalmos after a year.
Surgical follow up
Patients undergoing repair should have the vision checked in the recovery room t insure there is no intraoperative loss of vision, and then can be seen one week postoperatively, 3 weeks postoperatively, and 2-3 months postoperatively. A postoperative CT scan is often warranted to document the proper placement of the implant.
Orbital floor fracture repair complications
As with any surgical procedure, bleeding, infection, and the need for additional surgery are risks. The possible loss of vision is the most ominous complication associated with floor repair.
Residual or new-onset diplopia, neuralgia, and extraocular muscle dysfunction are potential complications. The patient should understand these risks completely, and no promises are to be made concerning resolution of any presurgical neuralgia 20.
Implant extrusion and residual enophthalmos are postoperative sequelae requiring additional surgery.
The most common mistakes and complications in the management of orbital floor fractures are the following:
- Operating too early: In many cases, diplopia resolves on its own in two or three weeks, or resolves to the point where it does not interfere with the patient’s activities (e.g, the patient is left with diplopia only in extreme upgaze). Unless there is severe restriction of motility where recovery of normal movement is clearly impossible without intervention, observing the patient for a period of one or two weeks is preferred prior to making a decision regarding surgery.
- Creating a subciliary incision or performing aggressive dissection through the lower eyelid: Lower eyelid malposition (such as severe cicatricial retraction) following a subciliary incision is common and difficult to treat; creating a transconjunctival incision and atraumatically dissecting through the lower eyelid bluntly prevents a multiple plane dissection, and minimizes the chances of scarring in the eyelid causing postoperative contracture and retraction.
- Not covering the entire posterior extent of the bony defect with the implant, especially posteriorly: Failure to cover the defect posteriorly can lead to herniation of tissue through the residual hole with scarring to the sinus mucosa, leading to postoperative enophthalmos and diplopia. It is essential to cover the entire defect, and fixation can insure that, once in place, the implant will not shift (especially anteriorly) and be displaced through the hole in the orbital floor.
- Visual loss: Nearly all cases of visual loss following orbital floor fracture repair occur due to elevated pressure in the orbit causing a compartment syndrome, either due to orbital hemorrhage or edema compressing the optic nerve. The optic nerve exits the orbit through the optic foramen, located at the superonasal portion of the orbit. As one surgically dissects posteriorly to gain access to the posterior rim of the floor fracture, the nerve is actually not in close proximity to the area of dissection. Many more complications ensue from failure to dissect posteriorly enough in the repair of the fracture than from causing direct injury to the optic nerve, an intraoperative complication which is extraordinarily rare and, from an anatomic point of view, difficult to produce.
Orbital floor fracture prognosis
Most patients who suffer an isolated orbital floor fracture—even those requiring surgical repair—have good outcomes. In those patients whose fractures are repaired appropriately, poor outcomes are generally associated with permanent paresis of an extraocular muscle (usually due to the initial injury) or fibrosis of an exrtraocular muscle causing restriction. Persistent enophthalmos may occur in the setting of fat atrophy.
Successful repair of orbital blowout fractures may be complicated by persistent problems. Neuralgia in the distribution of the infraorbital nerve may worsen after surgery. Improvement of this problem, if any, may take 6 months or more.
More troubling is persistent diplopia. If isolated to extreme positions of gaze, it may go unnoticed or may not be bothersome to the patient. However, if the diplopia affects functional positions of gaze, corrective prisms can be tried. Ultimately, eye muscle surgery may be required to address this problem with repositioning of the extraocular muscles to allow for orthophoric fixation of images.
A study by Su et al 21 of 83 pediatric patients with orbital blowout fractures found that the length of time for postoperative recovery from diplopia was associated with age, with the younger patients taking longer to recover than the older ones.
Enophthalmos can worsen over time. Despite adequately repairing the fracture, atrophy of the orbital fat can occur, resulting in further enophthalmos.
Long term complications related to implants, however, include implant infection, migration, capsular hemorrhage, and need for implant removal. These have been reported to occur even many years after the initial repair.
References- Koenen L, Waseem M. Orbital Floor (Blowout) Fracture. [Updated 2018 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534825
- Shin JW, Lim JS, Yoo G, Byeon JH. An analysis of pure blowout fractures and associated ocular symptoms. J Craniofac Surg. 2013 May;24(3):703-7.
- Joseph JM, Glavas IP. Orbital fractures: a review. Clin Ophthalmol. 2011 Jan 12;5:95-100.
- Emodi O, Wolff A, Srouji H, Bahouth H, Noy D, Abu El Naaj I, Rachmiel A. Trend and Demographic Characteristics of Maxillofacial Fractures in Level I Trauma Center. J Craniofac Surg. 2018 Mar;29(2):471-475.
- Della Rocca RC, Nassif JM. Blowout fractures. Linberg JV, ed. Oculoplastic and Orbital Emergencies. Appleton & Lange; 1990. 155-165.
- Hopper RA, Salemy S, Sze RW. Diagnosis of midface fractures with CT: what the surgeon needs to know. Radiographics. 2006 May-Jun;26(3):783-93.
- Felding UNA. Blowout fractures – clinic, imaging and applied anatomy of the orbit. Dan Med J. 2018 Mar;65(3).
- Schaller A, Huempfner-Hierl H, Hemprich A, Hierl T. Biomechanical mechanisms of orbital wall fractures – a transient finite element analysis. J Craniomaxillofac Surg. 2013 Dec;41(8):710-7.
- Patel S, Andrecovich C, Silverman M, Zhang L, Shkoukani M. Biomechanic Factors Associated With Orbital Floor Fractures. JAMA Facial Plast Surg. 2017 Mar 9. 2153.
- Bartoli D, Fadda MT, Battisti A, et al. Retrospective analysis of 301 patients with orbital floor fracture. J Craniomaxillofac Surg. 2015 Mar. 43(2):244-7.
- Boffano P, Roccia F, Gallesio C, et al. Diplopia and orbital wall fractures. J Craniofac Surg. 2014 Mar. 25(2):e183-5.
- Wilkins RB, Havins WE. Current treatment of blow-out fractures. Ophthalmology. 1982 May. 89(5):464-6.
- Tse R, Allen L, Matic D. The white-eyed medial blowout fracture. Plast Reconstr Surg. 2007 Jan. 119(1):277-86.
- Boush GA, Lemke BN. Progressive infraorbital nerve hypesthesia as a primary indication for blow-out fracture repair. Ophthal Plast Reconstr Surg. 1994 Dec. 10(4):271-5.
- Cheong EC, Chen CT, Chen YR. Endoscopic management of orbital floor fractures. Facial Plast Surg. 2009 Feb. 25(1):8-16.
- Farwell DG, Strong EB. Endoscopic repair of orbital floor fractures. Otolaryngol Clin North Am. 2007 Apr. 40(2):319-28.
- Suzuki M, Nakamura Y, Ozaki S, Yokota M, Murakami S. Repair of Orbital Floor Fracture With Modified Transnasal Endoscopic Approach Through Anterior Space to Nasolacrimal Duct. J Craniofac Surg. 2017 Jan 18.
- Holtmann H, Eren H, Sander K, Kubler NR, Handschel J. Orbital floor fractures–short- and intermediate-term complications depending on treatment procedures. Head Face Med. 2016 Jan 5. 12:1.
- Kronig SA, van der Mooren RJ, Strabbing EM, et al. Pure orbital blowout fractures reconstructed with autogenous bone grafts: functional and aesthetic outcomes. Int J Oral Maxillofac Surg. 2016 Apr. 45 (4):507-12.
- Harris GJ. Avoiding complications in the repair of orbital floor fractures. JAMA Facial Plast Surg. 2014 Jul-Aug. 16 (4):290-5.
- Su Y, Shen Q, Lin M, et al. Diplopia of pediatric orbital blowout fractures: a retrospective study of 83 patients classified by age groups. Medicine (Baltimore). 2015 Jan. 94(4):e477.