Osteonecrosis hip
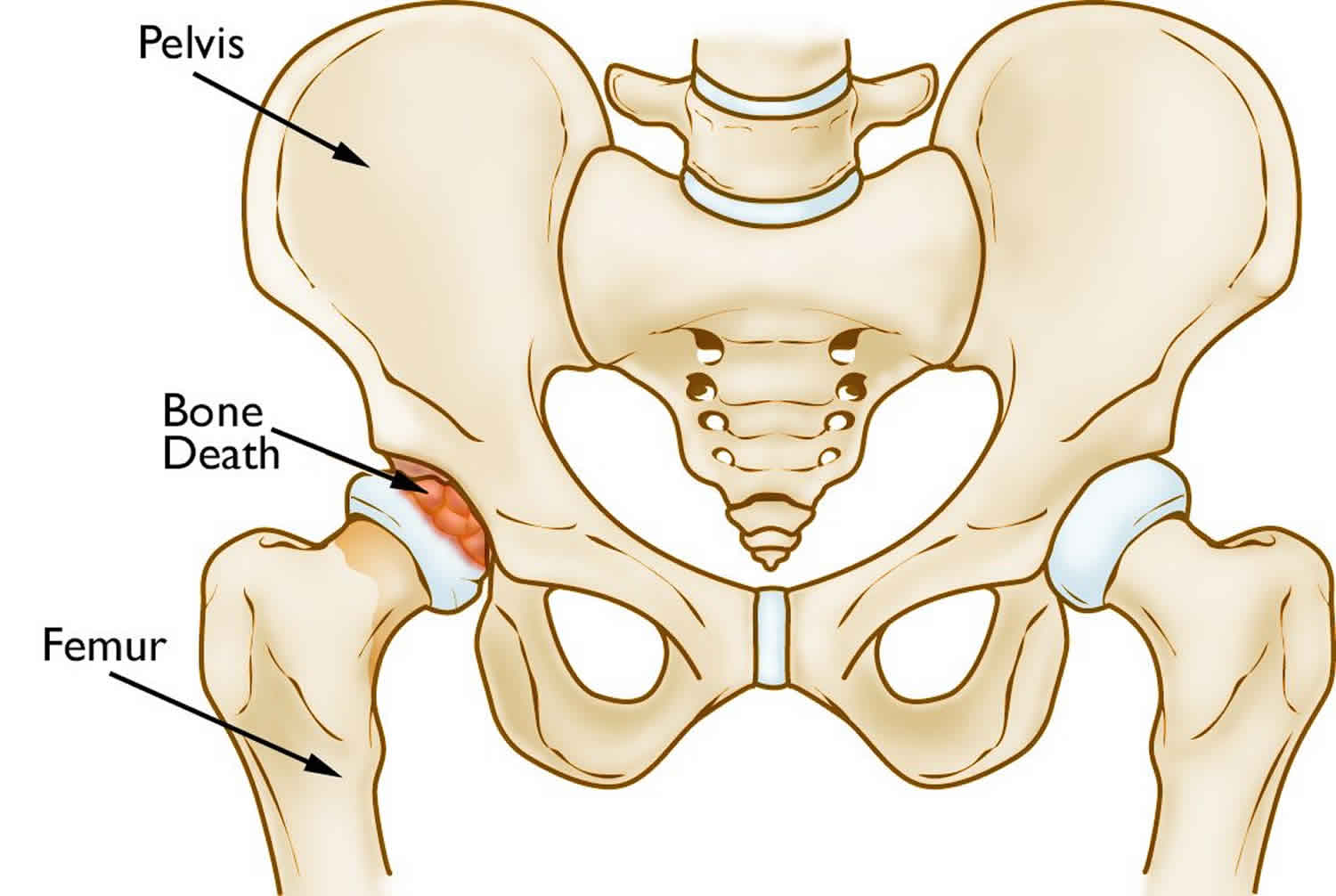
Osteonecrosis of the hip also called osteonecrosis of the femoral head, aseptic necrosis of the femoral head or avascular necrosis, is a condition where the blood supply to the femoral head is disrupted. Your femoral head is located at the top of your thigh bone (femur) and forms part of your hip joint. The lack of normal blood supply to the femoral head causes the bone to die. The bone is then weakened, predisposing it to collapse and osteoarthritis. Some people develop avascular necrosis in both hips (bilaterally).
There are 2 forms of osteonecrosis: traumatic (the most common form) and atraumatic. Other terms to describe osteonecrosis of the hip are avascular necrosis and ischemic necrosis to denote vascular cause. The term aseptic necrosis also has been used to indicate that infection does not play a causative role. The traumatic form of hip osteonecrosis occurs in 10% of undisplaced femoral neck fractures, 15-30% of displaced femoral neck fractures, and 10% of hip dislocations. At least 50% of patients with atraumatic hip osteonecrosis are thought to have bilateral involvement. Other bones often are involved in the atraumatic form, including the shoulder, knee, and talus. Corticosteroid use contributes to the atraumatic form of osteonecrosis in 5-25% of patients.
Most of the 10,000 to 20,000 Americans who develop osteonecrosis each year are between the ages of 20 and 50. Osteonecrosis can affect anyone, but is more common in people between the ages of 40 and 65. Men develop osteonecrosis of the hip more often than women (male-to-female ratio is about 4:1). These people most often have a history of serious trauma, corticosteroid use and excess alcohol intake.
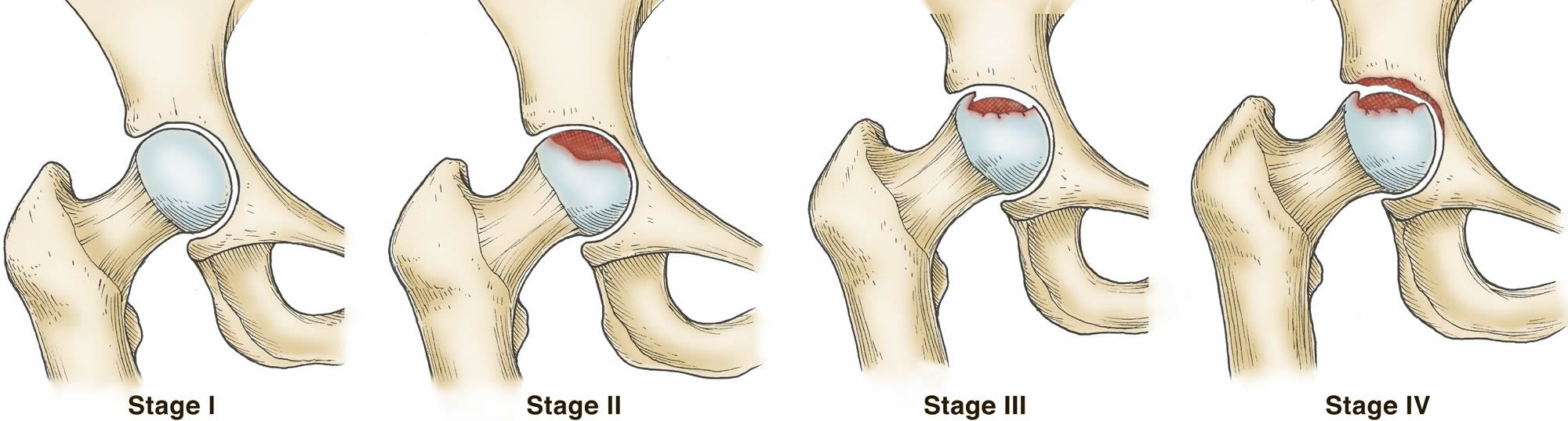
Osteonecrosis develops in stages (see Figure 2 below). Hip pain is typically the first symptom. This may lead to a dull ache or throbbing pain in the groin or buttock area. As the disease progresses, it becomes more difficult to stand and put weight on the affected hip, and moving the hip joint is painful.
Patients with osteonecrosis often have severe pain in the hip joint but relatively good range of motion. This is because only the femoral head is involved in the earlier stages of the disease. Later, as the surface of the femoral head collapses, the entire joint becomes arthritic. Loss of motion and stiffness can then develop.
It may take from several months to over a year for the disease to progress. It is important to diagnose osteonecrosis early, because some studies show that early treatment is associated with better outcomes.
If bone collapse occurs, complications include:
- Osteoarthritis
- Loss of joint function
- The need for a total or partial hip replacement
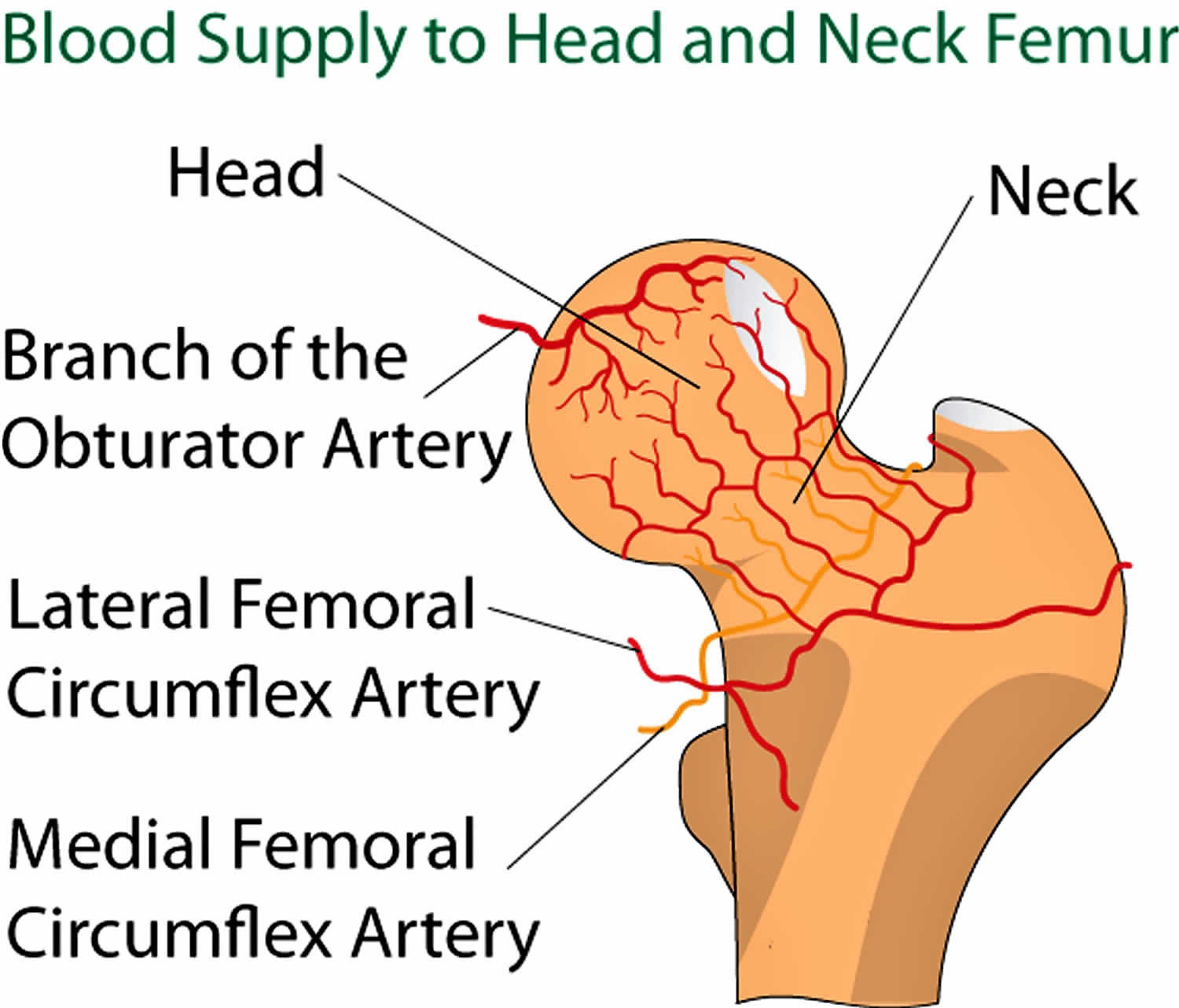
Femoral head blood supply
Blood is supplied to the femoral head primarily from branches of the medial and lateral circumflex vessels, which arise from the femoral artery. The retinacular branches deep to the posterior capsule are the most important. Blood also is supplied from the obturator artery.
Figure 1. Femoral head blood supply
Osteonecrosis hip staging
Several radiographic staging systems are currently used.
Ficat classification 1:
- Stage 0 – No pain, normal radiographic findings, abnormal bone scan or MRI findings
- Stage I – Pain, normal x-ray findings, abnormal bone scan or MRI findings
- Stage IIa – Pain, cysts and/or sclerosis visible on x-ray, abnormal bone scan or MRI findings, without subchondral fracture
- Stage III – Pain, femoral head collapse visible on x-ray, abnormal bone scan or MRI findings, crescent sign (subchondral collapse) and/or step-off in contour of subchondral bone
- Stage IV – Pain, acetabular disease with joint space narrowing and arthritis (osteoarthrosis) visible on x-ray, abnormal MRI or bone scan findings
Steinberg staging system 2:
- Stage 0 – Normal or nondiagnostic radiographic, bone scan, and MRI findings
- Stage I – Normal radiographic findings, abnormal bone scan and/or MRI findings
- A – Mild: < 15% of head affected
- B – Moderate: 15-30%
- C – Severe: >30%
- Stage II – Lucent and sclerotic changes in femoral head
- A – Mild: < 15%
- B – Moderate: 15-30%
- C – Severe: >30%
- Stage III – Subchondral collapse (crescent sign) without flattening
- A – Mild: < 15% of articular surface
- B – Moderate: 15-30%
- C – Severe: >30%
- Stage IV – Flattening of femoral head
- A – Mild: < 15% of surface or < 2-mm depression
- B – Moderate: 15-30% of surface or 2- to 4-mm depression
- C – Severe: >30% of surface or >4-mm depression
- Stage V – Joint narrowing and/or acetabular changes
- A – Mild: Average of femoral head involvement as in stage IV and estimated acetabular
- B – Moderate involvement
- C – Severe
- Stage VI – Advanced degenerative changes
International classification of osteonecrosis of the femoral head (Association Research Circulation Osseus) 3:
- Stage 0 – Bone biopsy results consistent with osteonecrosis; other test results normal
- Stage I – Positive findings on bone scan, MRI, or both
- A – < 15% involvement of the femoral head (MRI)
- B – 15-30% involvement
- C – >30% involvement
- Stage II – Mottled appearance of femoral head, osteosclerosis, cyst formation, and osteopenia on radiographs; no signs of collapse of femoral head on radiographic or CT study; positive findings on bone scan and MRI; no changes in acetabulum
- A – < 15% involvement of the femoral head (MRI)
- B – 15-30% involvement
- C – >30% involvement
- Stage III – Presence of crescent sign lesions classified on basis of appearance on AP and lateral radiographs
- A – < 15% crescent sign or < 2-mm depression of femoral head
- B – 15-30% crescent sign or 2- to 4-mm depression
- C – >30% crescent sign or >4-mm depression
- Stage IV – Articular surface flattened; joint space shows narrowing; changes in acetabulum with evidence of osteosclerosis, cyst formation, and marginal osteophytes
Figure 2. Osteonecrosis hip stages (International classification)
Footnote: The four stages of hip osteonecrosis. The disease can progress from a normal, healthy hip (Stage I) to the collapse of the femoral head and severe osteoarthritis (Stage IV).
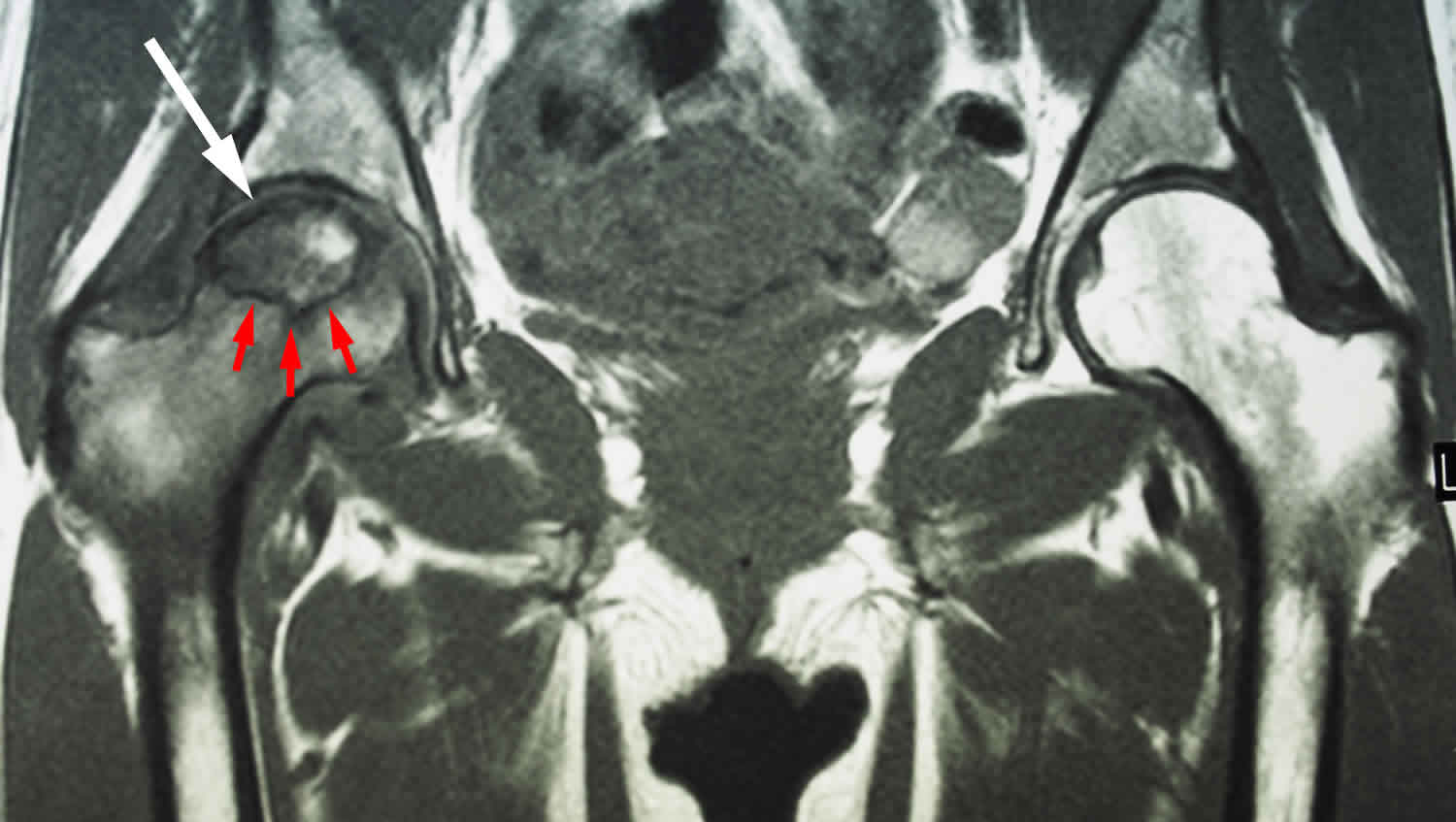
[Source 4 ]Figure 3. Osteonecrosis hip MRI scan
Footnote: This MRI scan shows osteonecrosis in a patient’s right hip (white arrow). The dark line (red arrows) denotes the border between dead bone and living bone. The patient’s left hip is normal.
Osteonecrosis hip causes
Osteonecrosis usually occurs when the blood vessels that provide blood to the femoral head are damaged, torn, or pinched. Without blood, the head of your femur dies and collapses leading to a deformity of the joint. This can lead to early osteoarthritis in the hip joint. Cartilage in the hip’s socket may also break down.
Traumatic osteonecrosis is secondary to direct injury to the femoral head with resultant damage of the blood supply to the femoral head. Fracture of the femoral head or neck and hip dislocation are the primary mechanisms of injury. Death of bone marrow occurs within 6-12 hours after vascular insult. Death of the bone becomes apparent several days later.
The list of causes for atraumatic osteonecrosis is long and includes alcohol abuse, gout, Caisson disease (decompression sickness), renal osteodystrophy (kidney disease), sickle cell anemia, Gaucher disease, systemic lupus erythematosus, coagulopathies, hyperlipidemia, organ transplantation, thyroid disorders and steroid use (corticosteriods) 5. Genetic factors may also play a role.
Sometimes, a cause cannot be found for osteonecrosis and is termed ‘idiopathic’ meaning there is no known cause.
Hip osteonecrosis resulting from corticosteroid use or alcohol abuse is associated with the worst prognosis 6. Frequently, steroid-induced osteonecrosis involves multiple bones and, in the case of the hip, results in nearly 100% bilateral involvement. The exact dose required to induce osteonecrosis remains an enigma, but most studies indicate that higher doses, even over a short duration, present the highest risk. Often, patients on steroids have other associated risk factors.
Osteonecrosis associated with alcohol abuse usually occurs in those who drink more than 400 mL of alcohol per week. It is more common in those with a long-term history of heavy consumption.
Studies have shown evidence of acquired hypercoagulabiltiy. This effect appears to be augmented by tobacco abuse 7. Recent studies have also shown elevated cryofibrinogen levels in atraumatic osteonecrosis 8.
Risk factors for osteonecrosis hip
It is important to remember that most patients with the following risk factors never develop osteonecrosis, and many patients without identifiable risk factors do acquire the disease. The process is most likely multifactorial.
It is not always known what causes the lack of blood supply, but doctors have identified a number of risk factors that can make someone more likely to develop osteonecrosis:
- Trauma – Hip dislocations, hip fractures, and other injuries to the hip can damage the blood vessels and impair circulation to the femoral head.
- Corticosteroid use – Many diseases, including asthma, rheumatoid arthritis, and systemic lupus erythematosus, are treated with steroid medications. Although it is not known exactly why these medications can lead to osteonecrosis, research shows that there is a connection between the disease and long-term corticosteroid use.
- Medical conditions. Conditions such as rheumatoid arthritis, sickle cell disease, myeloproliferative disorders, Gaucher’s disease, chronic pancreatitis, Crohn’s disease, Caisson’s disease (diver’s disease or “the bends”) or systemic lupus erythematosus (SLE).
- Excessive alcohol use. Overconsumption of alcohol over time can cause fatty deposits to form in the blood vessels and can elevate cortisone levels, resulting in a decreased blood supply to the bone.
Osteonecrosis hip prevention
The best way to prevent osteonecrosis of the hip is to avoid the risk factors, such as heavy alcohol intake.
Osteonecrosis hip symptoms
Osteonecrosis of the hip develops in stages. Many people have no symptoms in the early stages of osteonecrosis of the hip. As bone damage worsens, your affected joint might hurt only when you put weight on it. Eventually, you might feel the pain even when you’re lying down. Pain can be mild or severe and usually develops gradually. Pain associated with avascular necrosis of the hip might center on the groin, thigh or buttock.
You may have the following symptoms:
- Pain in the joint that may increase over time, and will become very severe if the bone collapses
- Pain that occurs even at rest
- Limited range of motion
- Groin pain
- Limping
Osteonecrosis hip diagnosis
Patients are typically asymptomatic early in the course of osteonecrosis and eventually have groin pain when walking.
A thorough history and physical examination will be performed to discover potential risk factors and to determine the extent of the problem.
The physical examination will involve the hip being flexed and rotated to check for pain.
X-rays will usually be taken as a first step of investigating the problem. Sometimes in early stages of osteonecrosis, the X-rays may appear normal in spite of the damage that may be present. In later stages of osteonecrosis, X-rays will show up characteristic signs due to the collapse of the bone caused by the osteonecrosis. Associated osteoarthritis may also be picked up on X-rays in long standing osteonecrosis of the hip.
There are other tests which may be performed which are more sensitive to the changes associated with osteonecrosis. These tests include
- Bone scanning – may be able to pick up early osteonecrosis
- Magnetic resonance imaging (MRI) allows earlier diagnosis of osteonecrosis of the femoral head and allows determination of the exact stage and extent of the process without. When X-rays show changes in only one joint, MRI of both hips is indicated, not only to define clearly the extent of the disease in the symptomatic hip, but also to evaluate the asymptomatic (unaffected) hip. This can allow detection of the disease in the early stages when most treatments are more effective. Sensitivity and specificity of MRI is greater than 98%, which is higher than all other modalities.
Laboratory tests have limited utility in the diagnosis of osteonecrosis, with exceptions as follows:
- Sickle cell testing in African Americans
- Lipid profile
- Screening for coagulopathies -Protein S and protein C deficiencies, factor V Leiden disease
Osteonecrosis hip treatment
Treatment depends on the extent of the damage to the hip joint due to the avascular necrosis. Once diagnosed with osteonecrosis of the hip, patients should not weight bear on the affected hip and crutches should be used, minimizing the amount of movement. However, nonsurgical treatment of osteonecrosis is limited. Certain cases of early-stage disease (eg, Ficat stage 1) can be treated successfully with this option. However, most studies indicate that the risk of disease progression is greater with nonsurgical treatment than with surgical intervention.
Nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to reduce pain and inflammation in patients who cannot have surgery for medical or other reasons or for patients who are undergoing surgical treatment.
Physical therapy can be helpful to restore motion and improve gait.
Electrical stimulation has been used in several centers. In some studies, it has been helpful in treatment prior to femoral head collapse. The benefit of surgical treatment options versus observation is controversial in certain cases. Further study is required.
Pharmacotherapy that addresses the pathophysiology of the disease has had mixed results. Examples include gemfibrozil (Lopid) for hyperlipidemias and nifedipine for vascular disorders. Alendronate has been suggested as an option to avoid or delay progression of the disease clinically and radiographically. However, one randomized study showed no significant difference in radiographic and MRI data between the alendronate and control groups 9. Short-term follow-up (about 24 months) of patients in alendronate studies have demonstrated delayed femoral head collapse 10.
Extracorporeal shockwave treatment has shown some promise in treating early disease by promoting angiogenesis and bone remodeling 11.
Surgical therapy
The mainstay of treatment for osteonecrosis is surgical. Numerous procedures are available, indicating that no single procedure is distinctly advantageous. Preoperative staging, particularly with collapse of the femoral head, and acetabular involvement are the determining factors for choosing a particular operation.
If the femoral head has not collapsed, a procedure known as Core Decompression may be performed. This involves removing some of the dead bone which has formed due to the blood supply being cut off and filling the area with a bone graft. This may stop the femoral head from collapsing and improve the chance of the joint remaining viable. Core decompression prevents osteonecrosis from progressing to severe arthritis and the need for hip replacement in some cases. This depends upon the stage and size of the osteonecrosis at the time of the procedure. Other procedures may also be performed with a view to minimizing damage to the hip.
The trapdoor procedure and allograft procedures are indicated for stage IIb or stage III lesions. Osteotomies are used for stage II and stage III disease. Arthrodesis (fusion of the hip joint) and arthroplasty (surgical reconstruction of hip joint) are utilized primarily for stages III and IV but occasionally are used for stages I and II.
If osteonecrosis has already collapsed your hip, total hip replacement surgery may be necessary to eliminate your pain and give you better hip mobility.
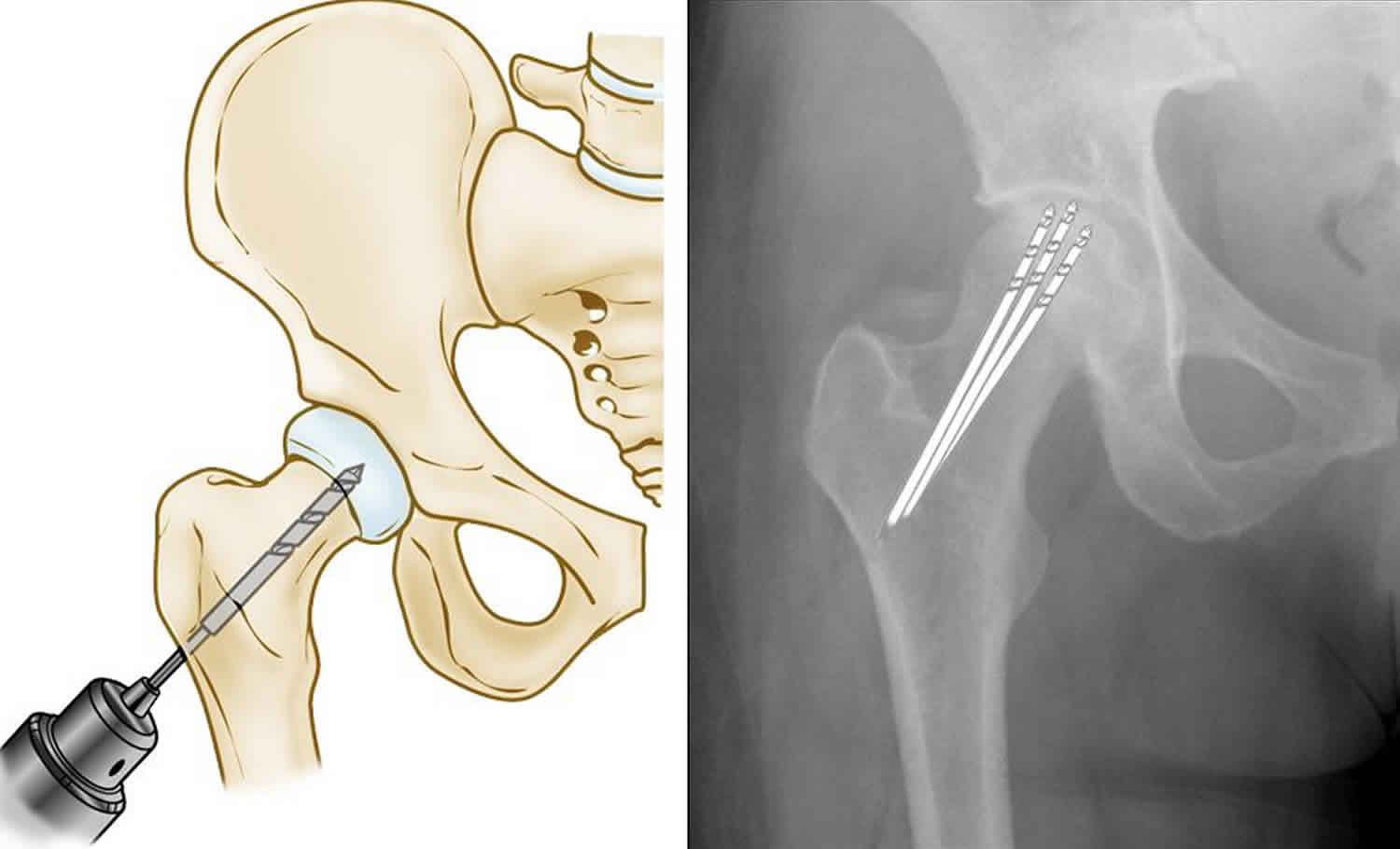
Core decompression
This procedure involves drilling one larger hole or several smaller holes into the femoral head to relieve pressure in the bone and create channels for new blood vessels to nourish the affected areas of the hip.
When osteonecrosis of the hip is diagnosed early, core decompression is sometimes successful in preventing collapse of the femoral head and the development of arthritis.
Core decompression achieves the best results when osteonecrosis is diagnosed in its early stages, before the bone collapses. In some of these cases, the bone heals and regains its blood supply after core decompression. It takes a few months for the bone to heal and, during this time, you will need to use a walker or crutches to avoid putting stress on the damaged bone.
Patients with successful core decompression procedures typically return to walking unassisted in about 3 months and have complete pain relief.
When osteonecrosis is diagnosed after collapse of the bone, core decompression is not usually successful in preventing further collapse. In this situation, the patient is best treated with a total hip replacement.
Figure 4. Core decompression
Footnote: (Left) Illustration of core decompression. (Right) In this x-ray, the drill lines show the pathway of the small drill holes used in the procedure.
Osteochondral (Bone and Cartilage) Grafting
Core decompression is often combined with bone and cartilage grafting to help regenerate healthy bone and support cartilage at the hip joint. A bone graft is healthy bone tissue that is transplanted to an area of the body where it is needed. The tissue may be taken from a donor (allograft) or from another bone in your body (autograft).
There are also several synthetic bone grafts available today.
Vascularized Fibula Graft
Another surgical option is a vascularized fibula graft. In this procedure, a segment of bone is taken from the small bone in your leg (fibula) along with its blood supply (an artery and vein). This graft is transplanted into a hole created in the femoral neck and head, and the artery and vein are reattached to help heal the area of osteonecrosis.
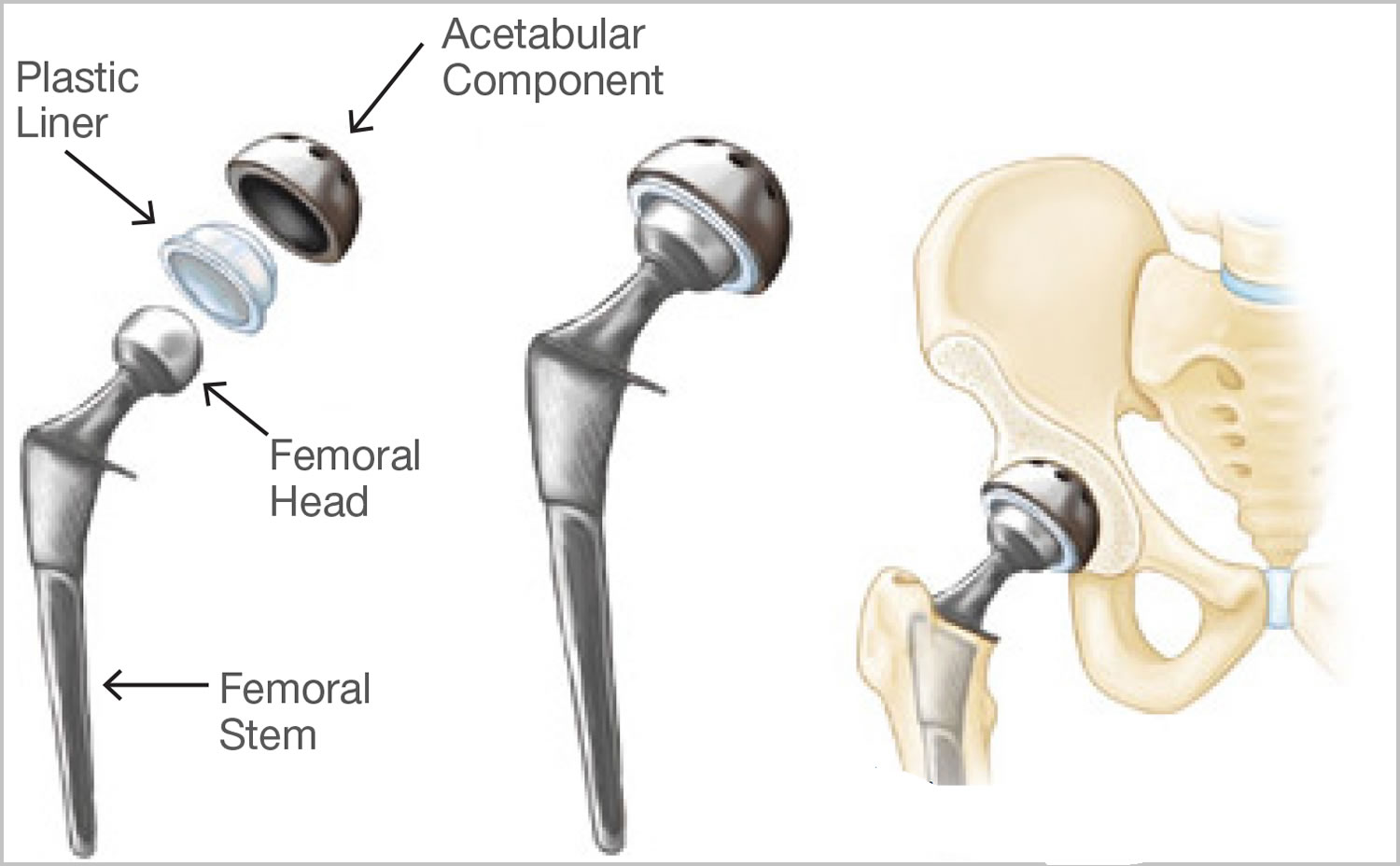
Total hip replacement
If osteonecrosis has advanced to the point where the femoral head has already collapsed, the most successful treatment is total hip replacement. In this procedure, your doctor removes the damaged bone and cartilage, then positions new metal or plastic joint surfaces to restore the function of your hip.
Total hip replacement is successful in relieving pain and restoring function in the majority of patients with osteonecrosis.
Figure 5. Total hip replacement
Osteonecrosis hip prognosis
The natural history of atraumatic osteonecrosis is still not well understood. Different causes of the disease often have different clinical courses. Steroid-induced disease has the worst prognosis, and most cases progress to collapse of the femoral head. Future studies hopefully will focus on the natural history of the disease.
The success rate in patients not treated by arthroplasty (surgical reconstruction of hip joint) in stage 0 or I approaches 90% in some series. Once femoral head collapse occurs, these treatments offer limited benefit. Procedures such as the trapdoor procedure potentially may improve results in stage II and III, but presently, total hip replacement remains the treatment of choice once collapse has occurred. If not treated, 80% of femoral heads collapse within 4 years of diagnosis. Location and extent of the necrotic lesion appear to be good indicators of collapse of the femoral head.
References- Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg [Br]. 1985 Jan. 67(1):3-9.
- Steinberg ME, Hayken GD, Steinberg DR. A new method for evaluation and staging of avascular necrosis of the femoral head. In: Arlet J, Ficat,P, Hungerford. Bone Circulation. Baltimore, Md: Williams and Wilkins. 1984:398-403.
- ARCO Committee on Terminology and Staging. The ARCO perspective for reaching one uniform staging system for osteonecrosis. In: Schoutens pathologic conditions. New York, NY: Plenum Press. 1993:375-80.
- Beaule PE, Amstutz, HC: Management of ficat stage III and IV osteonecrosis of the hip. J Amer Acad Orthop Surg 2004; 12: 96-105.
- Flouzat-Lachaniette CH, Roubineau F, Heyberger C, Bouthors C, Hernigou P. Multifocal osteonecrosis related to corticosteroid: ten years later, risk of progression and observation of subsequent new osteonecroses. Int Orthop. 2015 Dec 3.
- Hip Osteonecrosis. https://emedicine.medscape.com/article/1247804-overview
- Cenni E, Fotia C, Rustemi E, Yuasa K, Caltavuturo G, Giunti A, et al. Idiopathic and secondary osteonecrosis of the femoral head show different thrombophilic changes and normal or higher levels of platelet growth factors. Acta Orthop. 2011 Feb. 82(1):42-9.
- Soyfoo MS, Watik A, Stordeur P, Gangji V. Cryofibrinogen levels are increased in non-traumatic osteonecrosis: a new pathogenic clue to osteonecrosis?. Rheumatology (Oxford). 2013 Sep. 52(9):1694-700.
- Chen CH, Chang JK, Lai KA, Hou SM, Chang CH, Wang GJ. Alendronate in the prevention of collapse of the femoral head in nontraumatic osteonecrosis: A two-year multicenter, prospective, randomized, double-blind, placebo-controlled study. Arthritis Rheum. 2012 May. 64(5):1572-8.
- Lai KA, Shen WJ, Yang CY, Shao CJ, Hsu JT, Lin RM. The use of alendronate to prevent early collapse of the femoral head in patients with nontraumatic osteonecrosis. A randomized clinical study. J Bone Joint Surg Am. 2005 Oct. 87(10):2155-9.
- Gao F, Sun W, Li Z, Guo W, Wang W, Cheng L, et al. High-Energy Extracorporeal Shock Wave for Early Stage Osteonecrosis of the Femoral Head: A Single-Center Case Series. Evid Based Complement Alternat Med. 2015. 2015:468090.