Ureteral stricture
Ureteral stricture is a narrowing of the ureteral lumen, causing functional obstruction. The most common form of ureteral stricture is ureteropelvic junction obstruction, which is characterized by a congenital or acquired narrowing at the level of the ureteropelvic junction 1. Ureteral strictures may be staged based on location and severity. Location is divided into proximal (ureteropelvic junction to sacrum), mid (over sacrum), and distal (inlet of pelvis to ureterovesical junction). Severity commonly refers to the degree of urinary obstruction (ie, mild, moderate, severe).
Indications for intervention in patients with ureteral strictures include pain, infection, or obstruction, which may threaten a patient’s kidney function. Less common indications may include stone formation proximal to an obstruction or hematuria.
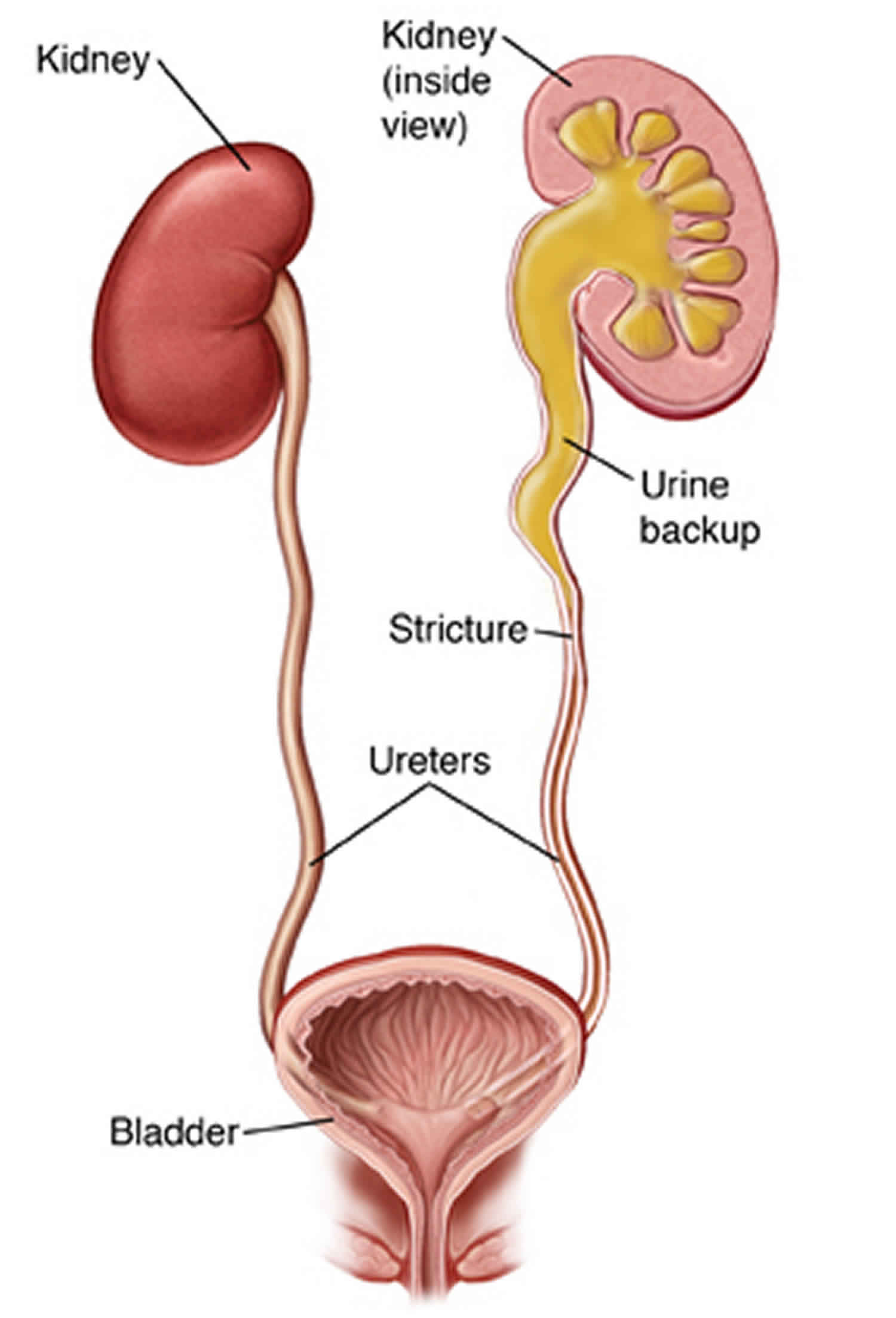
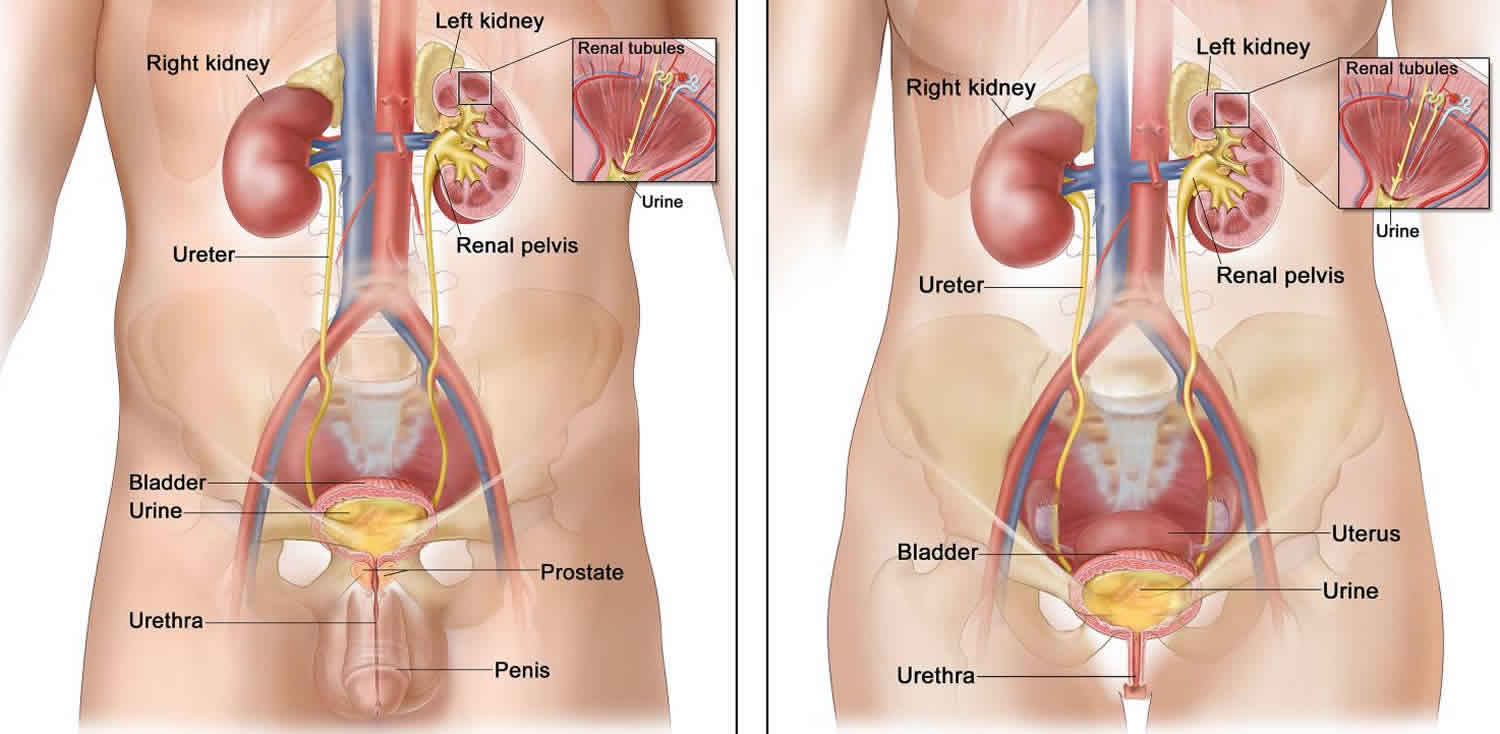
Ureter anatomy
The ureter is a muscular tube lined by transitional epithelium that courses from the renal pelvis to the bladder in the retroperitoneum.
The length of the ureter is 20-30 cm, depending on the individual’s height. The lumen size is 4-10 mm in circumference, depending on its location. The narrowest areas include the ureteropelvic junction, the overpass by the ureter where it crosses over the bifurcation of the iliac arteries, and the ureterovesical junction.
In both men and women, the ureter courses posterior to the gonadal vessels and anterior to the iliopsoas muscles, crosses the common iliac artery and vein, and enters inferiorly into the pelvis. In men, the vas deferens loops anterior to the ureter, prior to the ureter entering the bladder. In women, the ureter courses posterior to the uterine arteries (hence, the “water under the bridge” analogy) and close to the uterine cervix prior to reaching the intramural bladder.
The ureteral blood supply is provided from multiple sources. Superiorly, branches from the renal and gonadal arteries may contribute. As the ureter courses through the retroperitoneum, the aorta contributes numerous small branches. In the pelvis, the iliac, vesical, uterine, and hemorrhoidal arteries also contribute to the ureteral blood supply.
Figure 1. Ureter anatomy
Ureteral stricture causes
Ureteral strictures may be classified as follows 1:
- Extrinsic or intrinsic
- Benign or malignant
- Iatrogenic or noniatrogenic
Extrinsic malignant ureteral strictures include those caused by primary or metastatic cancer. Primary pelvic malignancies, particularly cancers of the cervix, prostate, bladder, and colon, frequently cause extrinsic compression of the distal ureter. Retroperitoneal lymphadenopathy, caused by a wide range of malignancies, particularly lymphoma, testicular carcinoma, breast cancer, or prostate cancer, may cause proximal to midureteral obstruction.
Extrinsic benign compression due to idiopathic retroperitoneal fibrosis may also cause unilateral or bilateral ureteral obstruction, leading to azotemia.
Transitional cell carcinoma may cause malignant intrinsic obstruction.
Malignant ureteral obstruction is differentiated from benign ureteral obstruction by (1) the presence of an extrinsic mass on a CT scan or sonogram and (2) the appearance of the ureter on contrast-study images.
Ureteral transitional cell carcinoma may manifest as ureteral obstruction. Ureteral transitional cell carcinomas typically have an irregular mucosal pattern and are associated with dilatation of the ureter below the lesion (goblet sign). Benign strictures are usually smooth, without distal dilatation. In some cases, biopsy may be required to differentiate benign from malignant strictures. Biopsy samples can usually be collected ureteroscopically or with a fluoroscopically directed ureteral brush. Ureteral tumors can also be diagnosed during transureteral resection of the tumor with specialized ureteral resectoscopes.
Benign intrinsic strictures may be congenital (eg, congenital obstructing megaureter), iatrogenic, or noniatrogenic (eg, those that follow passage of calculi or chronic inflammatory ureteral involvement [eg, tuberculosis and schistosomiasis]).
The widespread use of upper tract endoscopy has led to an increased frequency of iatrogenic ureteral stricture. Ureteral stricture has been reported with highly variable rates ranging from 0.2% to 24% 2. Early ureteroscopy studies reported ureteral stricture rates of 3%-11% in patients undergoing ureteroscopy for calculus management. More recent studies using smaller fiberoptic endoscopes; laser lithotripsy; and smaller, less traumatic instruments report a ureteral stricture rate of less than 1%.
In a review of 24 patients with highly impacted ureteral stones that were impacted for an average of 11 months, 24% of the patients developed postoperative ureteral strictures; therefore, impaction is a major risk factor. Ureteral perforation during these procedures has also been identified as a risk factor for stricture disease 3.
Factors associated with ureteral stricture development during ureteroscopy include the following:
- Large scope size
- Prolonged case duration
- Stone impaction
- Size
- Proximal location
- Perforation
- Use of intracorporeal lithotripsy
Ureteral strictures may complicate urinary diversions. The frequency of ureterointestinal anastomotic strictures during urinary diversion is 3%-5%. Ureteral injuries may result from any pelvic or retroperitoneal surgery, particularly abdominal hysterectomy and sigmoid colectomy. Gynecologic surgery is responsible for up to 75% of iatrogenic ureteral injuries.
Vakili et al 4 performed a prospective analysis of 479 patients undergoing hysterectomy for benign disease. Iatrogenic ureteral injury occurred in 8 patients (1.7%), comparable with previous ranges reported in the literature (0.02%-2.5%). Risk factors for urinary tract injury during hysterectomy include malignancy, pelvic radiation, endometriosis, prior surgery, and surgery for prolapse, although at least half of all ureteral injuries have no identifiable risk factors. Ureteral injuries or injury repairs may also result in strictures, although strictures of these causes are less common than strictures caused during endoscopy or anastomosis.
Iatrogenic benign ureteral strictures may result from various causes, including the following:
- Ureteroscopy
- Open or laparoscopic injury
- Radiation therapy
- Urinary diversions
- Renal transplantation
Ureteral stricture symptoms
Some patients with ureteral strictures are asymptomatic; others are symptomatic only during periods of diuresis or develop severe renal colic. The degree of symptoms correlates poorly with the degree of obstruction; at times, severe obstruction is asymptomatic or silent. Renal failure and azotemia may be due to bilateral strictures, such as in cases of bilateral ureteroenteric strictures, external compression due to retroperitoneal malignancy, or retroperitoneal fibrosis; recovery depends on the duration of ureteral obstruction.
Ureteral strictures are often found during routine follow-up imaging after ureteroscopy or intestinal urinary diversion. In this setting, asymptomatic hydroureteronephrosis proximal to the site of obstruction may occur. Most patients with significant strictures after ureteroscopy are symptomatic. They present with flank pain, flank fullness, or abdominal fullness.
In a review of 131 patients who underwent ureteroscopy and follow-up radiographic imaging, Karod et al 5 found no asymptomatic patients with residual obstruction. Thirteen of 21 patients with persistent flank pain had residual obstruction, one from a ureteral stricture.
Less frequently, persistent urinary tract infection or pyelonephritis is associated with unilateral ureteral obstruction. Patients with preexisting renal insufficiency or an abnormal contralateral kidney may present with an increased serum creatinine level or azotemia. Also, patients with strictures in solitary or functionally solitary kidneys (eg, renal transplant patients) may present with renal failure.
Ureteral stricture diagnosis
Important laboratory studies in ureteral strictures include the following:
- Urinalysis
- Urine culture and sensitivities
- Serum electrolytes with serum blood urea nitrogen and creatinine
Imaging studies
Imaging studies used for the assessment of ureteral stricture include the following:
- Renal ultrasonography
- Computed tomography
- Intravenous pyelography (IVP)
- Retrograde pyelography
- Nuclear medicine diuretic scan
- Intraluminal ultrasonography [7]
- Magnetic resonance imaging (MRI)
Renal ultrasonography
Renal ultrasonography is often the initial imaging study performed to evaluate for ureteral strictures because the findings are highly sensitive for hydronephrosis, the study is noninvasive, and the evaluation requires no intravenous contrast. Limitations of ultrasonography include fairly poor ureteral imaging, especially in patients who are obese, and the fact that this study is anatomic rather than functional.
Computed tomography
Noncontrast helical computed tomography is now commonly used to evaluate patients with acute flank pain and is therefore often performed in patients with a history of calculus disease. Noncontrast helical computed tomography findings are highly sensitive and specific for helping reliably identify hydroureteronephrosis and the site of dilatation. In addition, ureteral wall thickness, imbedded or extruded calculi, and urinary extravasation can be appreciated.
Secondary signs of obstruction (eg, periureteral stranding) can also be appreciated and do not require intravenous contrast for detection; however, noncontrast helical computed tomography is not a functional study and cannot be used to reliably estimate the degree of obstruction or relative renal function.
The addition of intravenous contrast to the CT scan allows assessment of the degree of obstruction, and a delayed nephrogram is often present. Delayed views provide important information regarding anatomic relationship of the strictured ureter to the adjacent structures. Contrast use must be counterbalanced by the nephrotoxicity of the contrast and the risk of adverse contrast reaction. Contrast CT scanning may be the best test for evaluating extrinsic causes of obstruction and evaluating regional or metastatic disease when malignant ureteral obstruction is evaluated.
Intravenous pyelography
Intravenous pyelography (IVP) was once the traditional functional imaging study of choice. Since the widespread availability of CT scanning, IVP is rarely used.
Intravenous pyelography (IVP) is particularly valuable in patients who have partial obstruction with normal renal function, but this imaging study is impaired by the risks of intravenous contrast.
Retrograde pyelography
Retrograde pyelography is very useful because it yields excellent ureteral-mucosal detail in the absence of intravenous contrast and is often used in preparation for endoscopic or open surgery to repair a ureteral stricture. Limitations include relative invasiveness and a requirement for cystoscopy.
Nuclear medicine diuretic scan
Nuclear medicine diuretic scan is most widely used test to measure the degree of obstruction and to quantify relative renal function. The diuretic renal scan is used to measure clearance of the radiopharmaceutical over time and to calculate renal blood flow, which correlates with relative renal function.
The most common radiopharmaceuticals currently used to evaluate relative function and obstruction include technetium-99m (Tc 99m) mercaptoacetyltriglycine, which is primarily a tubular agent, and Tc 99m diethylenetriamine pentaacetic acid, which is primarily a glomerular agent. At the peak uptake of the radiopharmaceutical, intravenous furosemide, usually 20 mg, may be administered to induce diuresis and to allow the assessment of urinary clearance.
Relative disadvantages of nuclear medicine diuretic scans include the following:
- Its qualitative nature
- User dependence
- Lack of informative anatomic data
Magnetic resonance imaging
Magnetic resonance imaging (MRI) may be useful for evaluating patients with a renal transplant who have renal failure and in whom ultrasonographic findings are normal or equivocal.
Ureteral stricture treatment
No accepted medical treatment of ureteral strictures currently exists.Surgical procedures used in these patients include the following:
- Balloon dilation
- Endoureterotomy
- Placement of metal ureteral stents
- Open surgery
Laparoscopic and robot-assisted laparoscopic surgery are increasingly used to replicate the results offered by open surgery.
Ureteral stricture surgery
Ureteral stricture surgery contraindications
The major contraindication to ureteral stricture surgery (endoscopic or open) is an active and untreated urinary tract infection. A relative contraindication is uncorrected bleeding diathesis.
When ureteral stricture surgery (endoscopic or open) is contemplated, many patient factors should be considered.
If the patient has a terminal malignancy, is extremely elderly, or has a high surgical risk and tolerates internal stenting well, long-term stenting may be most appropriate. Chung et al analyzed 101 patients with extrinsic ureteral obstruction managed with indwelling ureteral stents 6. Within 1 year, the stents failed in 41% of the patients. Thirty percent of patients needed percutaneous nephrostomy tube placement at a mean of 40 days. Predictors of stent failure included cancer, a baseline creatinine level of greater than 1.3 mg/dL, and poststent systemic treatment.
If the affected kidney has less than 25% renal function, balloon dilation and endoureterotomy are more likely to fail 7. Therefore, the patient is at significant risk for eventually requiring open surgery or nephrectomy. Few data exist on the outcomes of open surgery based on preoperative renal function. Renal function may significantly improve in some patients with poor function due to obstruction after the obstruction is corrected. If the renal function is less than 10%, recovery is unlikely and initial nephrectomy may be most appropriate.
Balloon dilation
The most common initial management of benign ureteral strictures is balloon dilation, followed by stent placement for 4-6 weeks. Hafez and Wolf 8 reviewed 8 published series of ureteral strictures managed with balloon dilation. Success rates ranged from 48%-88%. Of the 280 ureteral strictures treated, the overall mean success rate was 55%. They found balloon dilation best suited for very short nonischemic strictures.
Goldfischer and Gerber 9 summarized the results of balloon dilation in a large series and found this procedure to yield a success rate of 50%-76%. Factors associated with a good outcome included short duration (< 3 months) and short length of stricture. Given the frequent need for multiple procedures and the higher success rate associated with endoureterotomy, most urologists recommend endoscopic incision as the initial minimally invasive management of ureteral stricture disease 10.
Endoureterotomy
This procedure is also commonly performed for benign strictures and boasts a higher success rate than balloon dilation. Hafez and Wolf 8 reviewed 8 published series of endoureterotomy for benign stricture disease and found success rates of 55-85%. The overall success rate was 78% in the 156 patients. Goldfischer and Gerber 9 found that an endoureterotomy has a success rate of 62-100%. In a large review assessing endoureterotomy and factors associated with success, Wolf et al 7 found a success rate of 82% for benign strictures. Poor renal function (< 25% overall function), long strictures (>1 cm), and tight stricture lumen (< 1 mm) are associated with a poorer outcome. Wolf et al 7 found that the use of triamcinolone injection into the stricture bed and large stents (>12F) are useful for long strictures (>1 cm). Recent long-term studies indicate a success rate of closer to 50% after 5-year follow-up.
Ureteral metal stents
Metal stents, which have been used to treat end-stage malignant disease, provide proximal decompression, although recurrence of the obstruction is possible. Stent removal is extremely difficult, and stent migration has been reported. Some attempts to apply them to benign ureteral strictures and ureteropelvic junction obstruction and ureterovesical obstruction have been made. Liatsikos et al 11 reported on their experience of 102 patients with a total of 142 ureters stented. The primary stent patency rate was 66%. They did not report on the time interval in which the stents became occluded.
Liatsikos and colleagues 12 also reported on their experience using self-expandable metal stents for ureteroileal anastomotic strictures. They treated a total of 24 ureteroileal conduits with a technical success of 100% and an immediate postoperative clinical success rate of 70.8%. The 1- and 4-year primary patency rates were 37.8% and 22.7%, respectively. Despite the high occlusion rates, the authors contend that the placement of metal stents is appropriate in patients who may not be candidates for open surgery.
Innovations in the materials and design of ureteric stents will likely continue. A number of metallic microcoiled stents coated with polymers that retard stone growth are currently on the market. These stents can be used in patients who require long-term stent changes or in those with malignant obstruction due to terminal illness. The stents can be changed every 6-12 months. Periodic cystoscopy to rule out stent encrustations has been recommended.
Open surgical management
Open surgical management includes various treatment options such as psoas hitch, Boari flap, ureteroneocystostomy, transureteroureterostomy, intestine interposition, renal mobilization, and autotransplant. All open procedures carry an increased risk of morbidity, increased recovery time, and increased hospitalization time compared with endoscopic approaches.
The surgical approach used depends primarily on the location of the ureteral stricture. Distal strictures that require open repair are best managed with ureteroneocystostomy or a psoas hitch, depending on the proximity to the ureteral orifice. If more length is required, a Boari flap can bridge a 10- to 15-cm defect and may reach the mid ureter.
For midureteral strictures, a primary ureteroureterostomy may be appropriate for short benign strictures with minimal tension. Transureteroureterostomy may be used if the donor ureter is of adequate length and the recipient ureter is not diseased. Relative contraindications to transureteroureterostomy include conditions that may affect both ureters (eg, transitional cell carcinoma, urolithiasis, radiation, chronic infection, retroperitoneal fibrosis).
Proximal ureteral strictures may be managed with ureteropyelostomy if length allows. Also, ureterocalicostomy is useful if the renal pelvis is scarred or intrarenal in location.
Long, complex upper tract ureteral strictures have traditionally been managed with nephrectomy, bowel interposition, and autotransplantation. For long, extensive ureteral strictures that are not amenable to repair with urothelium, ileal ureteral substitution may be a satisfactory solution. Franke and Smith have stated that contraindications to ileal ureter substitution include renal insufficiency (serum creatinine level >2 mg/dL), bladder outlet obstruction, inflammatory bowel disease, and radiation enteritis.
In a retrospective review of 51 patients who underwent renal autotransplantation, kidney function was preserved postoperatively and 2 graft losses occurred. Complication rates compared favorably with those of other major urological operations and cold ischemia time was the only predictor of postoperative complications 13.
Laparoscopic and robot-assisted laparoscopic repair
Laparoscopic and robot-assisted laparoscopic surgery are increasingly used to replicate the results offered by open ureteral stricture surgery. Simmons and colleagues 14 retrospectively compared 12 patients who underwent laparoscopic surgery with 34 patients who underwent open ureteroureterostomy, ureteroneocystostomy, and Boari flap procedures. The average operative blood loss was 258 mL in the open group versus 86 mL in the laparoscopic group; the hospital stay was a median of 5 days in the open group versus 3 days in the laparoscopic group. The overall complication rate was higher in the open group (15%) than in the laparoscopic group (8%). No significant differences were found in the patency or duration of follow-up between the two groups.
Tran et al 15, reviewed analyzed the results of 52 patients who underwent laparoscopic nephrectomy with autotransplantation for complex ureteral and renal conditions included ureteral stricture disease. The study found a greater than 90% success rate with longer than 6-year median followup.
Fugita and colleagues 16 reported 3 successful cases of distal ureteral stricture treated with laparoscopic Boari flap creation. Modi et al 17 reported the successful use of laparoscopic ureteroneocystostomy with psoas hitch in 6 patients with ureterovaginal fistula in whom endoscopic management initially failed. The first reported use of laparoscopic ureteroureterostomy was published in 1998 and detailed 9 patients with symptomatic endometriosis of the ureter treated with resection and primary repair 18. One patient had recurrent stricture that responded to endoscopic dilation.
With the increasing availability of the da Vinci robot system, this technology has been successfully applied to ureteral stricture disease. It offers the advantage of easier intracorporal suturing and knot tying. Multiple centers have reported small case series documenting successful treatment of distal ureteral stricture with robot-assisted laparoscopic reimplantation, with and without psoas hitch or Boari flap 19.
Follow-up
Early follow-up imaging studies are typically performed 2-4 weeks after stent removal and include renal ultrasonography, IVP, or renal scintigraphy. A serum creatinine evaluation and urine culture are often performed.
If the patient is asymptomatic, imaging is performed at 3 months and then at 6-month intervals for the first 2 years. Most stricture recurrences are identified within the first year after surgery.
For excellent patient education resources, see eMedicineHealth’s patient education articles Intravenous Pyelogram, Magnetic Resonance Imaging (MRI), and CT Scan.
Ureteral stricture surgery complications
Balloon dilation
- Infection
- Failure to successfully dilate
- Loss of renal access
- Subsequent need for percutaneous nephrostomy drainage
Endoureterotomy
- Infection
- Failure to successfully dilate
- Loss of renal access
- Subsequent need for percutaneous nephrostomy drainage
- Direct injury to adjacent structures (eg, bowel or vascular structures, urinoma formation)
- Vascular injury: Yamada et al reported that 1 of 20 patients treated with a cold-knife ureterotomy had a major vascular injury that required an immediate laparotomy 20.
Open surgical repair
- Prolonged ileus
- Urinoma
- Prolonged urine leak from repair
- Bowel injury
- Sepsis
- Late adhesion formation
- Small bowel obstruction
- Risks of major surgery (eg, deep venous thrombosis, myocardial infarction, surgical mortality)
- Impaired bladder function: Patients who undergo psoas hitch or Boari flap may develop impaired bladder function.
Ureteral stricture prognosis
The success rate of balloon dilation is 48%-88%, with a mean of approximately 55%. The length and location of the stricture are important factors, with short and distal strictures responding best.
The success rate of endoureterotomy used to manage benign strictures is 78%. Higher success rates are achieved in nonischemic strictures, those shorter than 1 cm, and those treated less than 24 months from the etiologic event. In addition, the use of a large stent (>12F) is associated with a better outcome, as is stenting for less than 4 weeks.
The success rate of endoureterotomy used to manage ureteroenteric strictures is 32% at 3 years. Right ureteroenteric strictures tend to have better outcomes compared with left ureteroenteric strictures. Large stents (>12F) are associated with better outcomes, as is longer stenting, ie, over weeks 7.
The success rate of balloon dilation used to manage ureteral strictures after renal transplantation is 45%-79%. Antegrade or retrograde cold-knife incision has a success rate of 82% at 26 months.
The success rate of open surgical repair of ureteral strictures is over 90%.
References- Ureteral stricture. https://emedicine.medscape.com/article/442469-overview
- Darwish AE, Gadelmoula MM, Abdelkawi IF, Abdellatif AM, Abdel-Moneim AM, Hammouda HM. Ureteral stricture after ureteroscopy for stones: A prospective study for the incidence and risk factors. Urol Ann. 2019;11(3):276–281. doi:10.4103/UA.UA_110_18 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6676818
- Tas S, Tugcu V, Mutlu B, Karadag S, Bitkin A, Yücel M, et al. Incidence of ureteral stricture after ureterorenoscopic pneumatic lithotripsy for distal ureteral calculi. Arch Ital Urol Androl. 2011 Sep. 83(3):141-6.
- Vakili B, Chesson RR, Kyle BL, Shobeiri SA, Echols KT, Gist R, et al. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. Am J Obstet Gynecol. 2005 May. 192(5):1599-604.
- Karod JW, Danella J, Mowad JJ. Routine radiologic surveillance for obstruction is not required in asymptomatic patients after ureteroscopy. J Endourol. 1999 Jul-Aug. 13(6):433-6.
- Chung SY, Stein RJ, Landsittel D, Davies BJ, Cuellar DC, Hrebinko RL, et al. 15-year experience with the management of extrinsic ureteral obstruction with indwelling ureteral stents. J Urol. 2004 Aug. 172(2):592-5.
- Wolf JS Jr, Elashry OM, Clayman RV. Long-term results of endoureterotomy for benign ureteral and ureteroenteric strictures. J Urol. 1997 Sep. 158(3 Pt 1):759-64.
- Hafez KS, Wolf JS Jr. Update on minimally invasive management of ureteral strictures. J Endourol. 2003 Sep. 17(7):453-64.
- Goldfischer ER, Gerber GS. Endoscopic management of ureteral strictures. J Urol. 1997 Mar. 157(3):770-5.
- Kwak S, Leef JA, Rosenblum JD. Percutaneous balloon catheter dilatation of benign ureteral strictures: effect of multiple dilatation procedures on long-term patency. AJR Am J Roentgenol. 1995 Jul. 165(1):97-100.
- Liatsikos EN, Kagadis GC, Barbalias GA, Siablis D. Ureteral metal stents: a tale or a tool?. J Endourol. 2005 Oct. 19(8):934-9.
- Liatsikos EN, Kagadis GC, Karnabatidis D, Katsanos K, Papathanassiou Z, Constantinides C, et al. Application of self-expandable metal stents for ureteroileal anastomotic strictures: long-term results. J Urol. 2007 Jul. 178(1):169-73.
- Cowan NG, Banerji JS, Johnston RB, Duty BD, Bakken B, Hedges JC, et al. Renal Autotransplantation: 27-Year Experience at 2 Institutions. J Urol. 2015 Nov. 194 (5):1357-61.
- Simmons MN, Gill IS, Fergany AF, Kaouk JH, Desai MM. Laparoscopic ureteral reconstruction for benign stricture disease. Urology. 2007 Feb. 69(2):280-4.
- Tran G, Ramaswamy K, Chi T, Meng M, Freise C, Stoller ML. Laparoscopic Nephrectomy with Autotransplantation: Safety, Efficacy and Long-Term Durability. J Urol. 2015 Sep. 194 (3):738-43.
- Fugita OE, Dinlenc C, Kavoussi L. The laparoscopic Boari flap. J Urol. 2001 Jul. 166(1):51-3.
- Modi P, Goel R, Dodiya S. Laparoscopic ureteroneocystostomy for distal ureteral injuries. Urology. 2005 Oct. 66(4):751-3.
- Nezhat CH, Nezhat F, Seidman D, Nezhat C. Laparoscopic ureteroureterostomy: a prospective follow-up of 9 patients. Prim Care Update Ob Gyns. 1998 Jul 1. 5(4):200.
- Glinianski M, Guru KA, Zimmerman G, Mohler J, Kim HL. Robot-assisted ureterectomy and ureteral reconstruction for urothelial carcinoma. J Endourol. 2009 Jan. 23(1):97-100.
- Yamada S, Ono Y, Ohshima S, Miyake K. Transurethral ureteroscopic ureterotomy assisted by a prior balloon dilation for relieving ureteral strictures. J Urol. 1995 May. 153(5):1418-21.