Periosteal reaction
Periosteal reaction also known as periostitis, periosteitis or periosteal new bone formation, is a non specific radiographic finding that occurs with periosteal irritation can result from any of a large number of causes. The morphological appearance of periostitis can be helpful, but is usually not sufficiently specific to determine its cause. Establishing whether periosteal new bone formation is solitary versus multi-focal (or generalized) is useful in narrowing the diagnostic possibilities. Common causes of solitary periosteal new bone formation would include healing fractures, chronic stress injuries, subperiosteal hematomas (e.g., cephalohematoma), osteomyelitis, and bone tumors. The appearance of the adjacent bone will gives clues as to which of these is the most likely etiology.
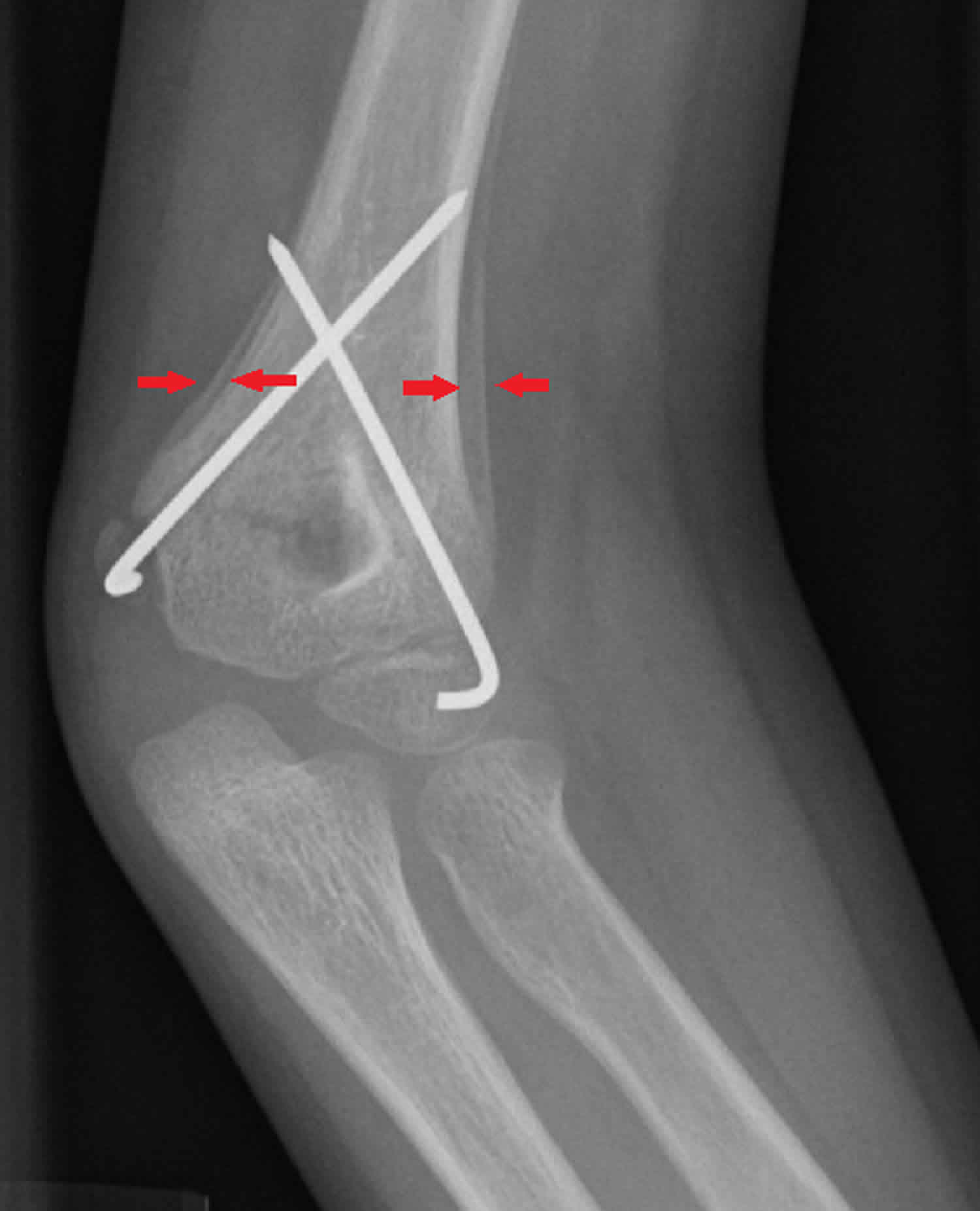
Figure 1. Schematic diagram of periosteal reactions
Footnote: Schematic diagram of periosteal reactions, regardless of their cause. On top of this, there are complex or disorganized periosteal reactions, which could be a combination of any of these.
Types of periosteal reaction
Periosteal reactions may be broadly characterized as benign or aggressive (not benign and malignant), or more specifically broken down by pattern and based on the time course of the initiating process.
Benign periosteal reaction
Low-grade chronic irritation allows time for the formation of normal or near-normal cortex. The cortex will be thick and dense and have a wavy or uniform appearance.
Benign periosteal reactions can be seen in callus formation in a fracture or with slowly growing tumors.
Aggressive periosteal reaction
Rapid irritative processes do not allow the periosteum time to lay down and consolidate new bone to form normal cortex. The cortex may appear lamellated, amorphous, or sunburst-like.
Aggressive periosteal reactions can not only be seen with malignant tumors, but also with more benign processes like infection, eosinophilic granuloma (Langerhans cell histiocytosis), aneurysmal bone cyst, osteoid osteoma, hemophilia 1 and trauma.
Morphological classification of periosteal reactions
More specific classification of periosteal reactions can be made to narrow the differential diagnosis:
- single layer
- multilayered
- solid
- spiculated
- perpendicular (hair-on-end)
- divergent (sunburst)
- sloping (velvet)
- disorganized/complex
- Codman triangle
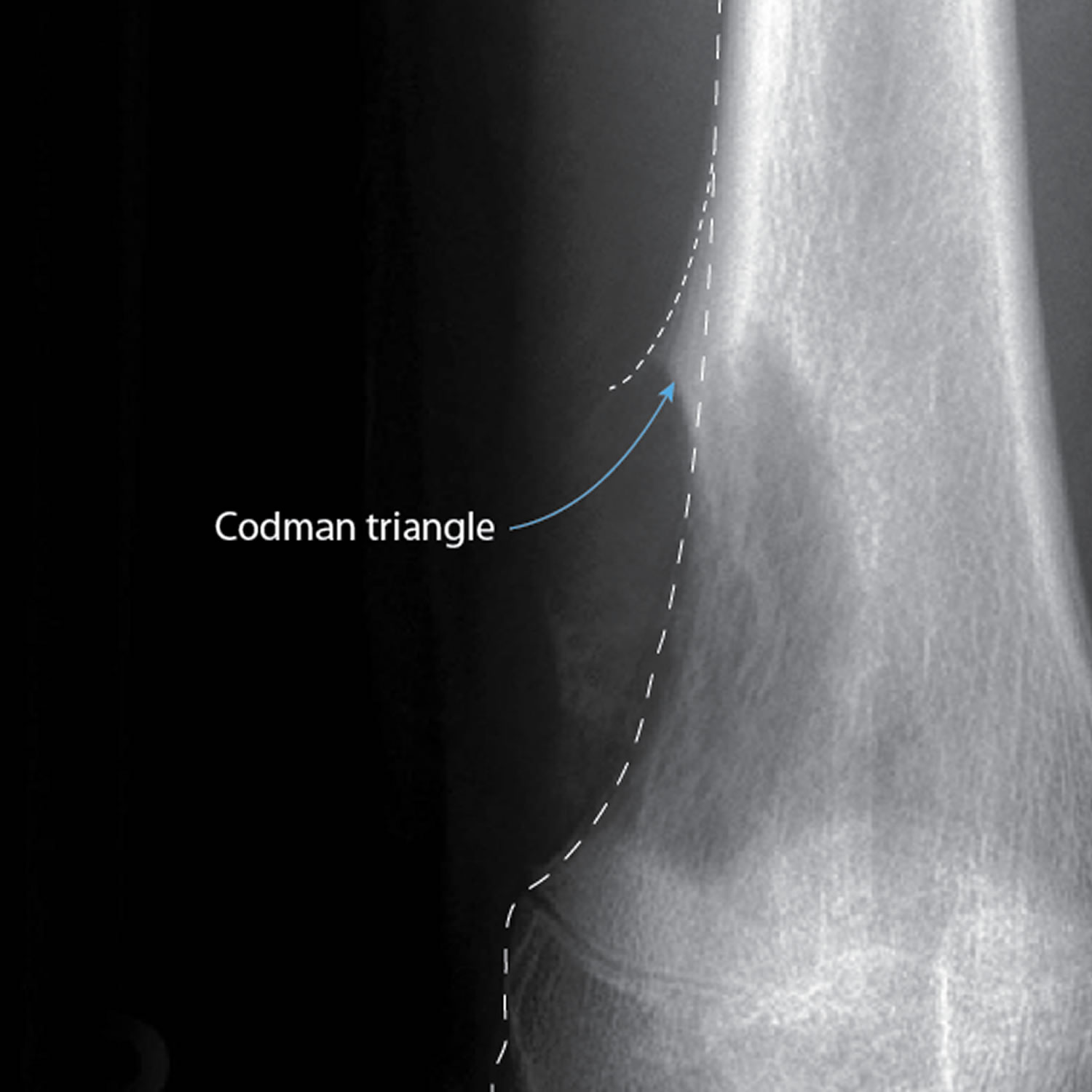
Codman triangle periosteal reaction
Codman triangle is a type of periosteal reaction seen with aggressive bone lesions. The periosteum does not have time to ossify with shells of new bone (e.g. as seen in a single layer and multilayered periosteal reaction) in aggressive lesions, so only the edge of the raised periosteum will ossify.
The Codman triangle may be seen with the following aggressive lesions:
- Osteosarcoma
- Ewing sarcoma
- Osteomyelitis
- Active aneurysmal bone cyst
- Giant cell tumor
- Metastasis
- Chondrosarcoma (especially juxtacortical chondrosarcoma)
- Malignant fibrous histiocytoma
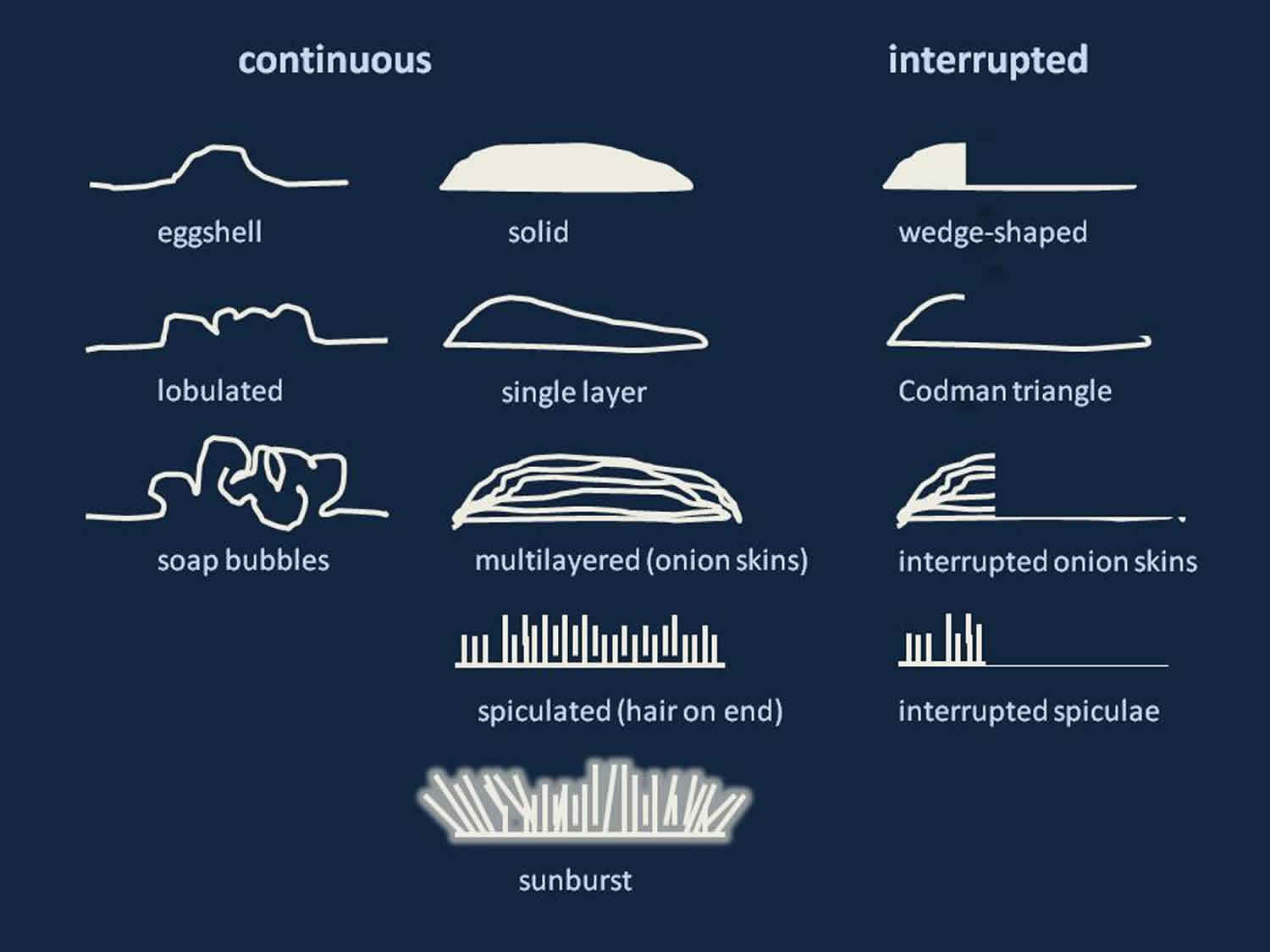
Figure 2. Codman triangle periosteal reaction
Footnote: Codman triangle is a type of periosteal reaction seen with aggressive bone lesions, in this case an osteosarcoma.
Disorganized periosteal reaction
Disorganized or complex periosteal reaction has spicules with random orientation and appearance. It can be seen in highly aggressive processes:
- osteosarcoma
- metastasis
- osteomyelitis
- chondrosarcoma
- Ewing sarcoma
- stress fracture
- malignant fibrous histiocytoma
- spindle cell sarcoma
Sunburst periosteal reaction
Sunburst appearance is a type of periosteal reaction giving the appearance of a sunburst secondary to an aggressive periostitis. It should not be confused with the sunburst sign of meningioma vascularity.
The sunburst appearance occurs when the lesion grows too fast and the periosteum does not have enough time to lay down a new layer and instead the Sharpey’s fibers stretch out perpendicular to the bone. It is frequently associated with osteosarcoma but can also occur with other aggressive bony lesions such as an Ewing sarcoma or osteoblastic metastases (e.g. prostate, lung or breast cancer)
Figure 3. Sunburst periosteal reaction
Footnote: Case of osteosarcoma. A malignant bone tumor accounting for 20% of primary bone tumors. An ill-defined sclerotic area affecting the metaphysis of distal fibula with an aggressive periosteal reaction (sunburst type). This lesion involves the adjacent posterior aspect of the tibia and the calcaneum inferiorly. It is associated with a moderately large soft tissue swelling.
Multilayered periosteal reaction
Multilayered periosteal reaction, also known as a lamellated or onion skin periosteal reaction, demonstrates multiple concentric parallel layers of new bone adjacent to the cortex, reminiscent of the layers on an onion. The layers are thought to be the result of periods of variable growth 2.
Multilayered periosteal reaction has been associated with:
- osteosarcoma
- acute osteomyelitis
- Ewing sarcoma
- Langerhans cell histiocytosis
- hypertrophic osteoarthropathy
Figure 4. Multilayered periosteal reaction
Footnote: Osteoblastic metastases from prostate cancer presenting as knee pain in a 70 year old man. The distal femur and proximal tibia show a diffuse increase in density with a patchy texture. A lamellated periosteal reaction is observed circumferentially around the distal femoral metaphysis, however no focal area of cortical violation or associated soft-tissue mass is observed. It is a bit unusual to see a periosteal reaction with protate mets, or in any older individual for that matter because the periosteum is tightly adhered to bone and limited in its ability to react quickly or robustly to an underlying pathology. The blastic changes in this case however are none-the-less characteristic, and blastic mets from prostatic carcinoma must be the #1 differential diagnosis in an elderly male with patchy sclerotic bone changes.
Single layer periosteal reaction
Single layer periosteal reaction is a uniformly dense, single thin layer of new bone about 1-2 mm from the cortical surface. Passive hyperemia causes increased osteoblastic activity and production of new bone. It is seen in:
- premature infants for up to 6 months
- early fracture healing
- osteosarcoma
- osteomyelitis
- Langerhans cell histiocytosis
- metastasis
- osteoid osteoma
- aneurysmal bone cyst
- Ewing sarcoma
- giant cell tumor
- chronic venous insufficiency
Figure 5. Single layer periosteal reaction
Footnote: This leg x-ray shows periosteal reaction around tibia and fibula. There is also soft tissue calcification medial to the tibia. This patient had chronic venous disease of the lower limbs, and the soft tissue calcification probably represents phleboliths within varicose veins. Periosteal reaction due to venous stasis is typically solid and undulating, and initially separated from the cortex, as in this case.
Solid periosteal reaction
Solid periosteal pattern is thought to evolve from single layer and multilayered periosteal reactions, forming a solid layer of new bone adjacent to the cortex.
Solid periosteal reaction can be seen in:
- osteoid osteoma
- osteomyelitis
- osteosarcoma
- chondrosarcoma
- fibrous dysplasia
- non-ossifying fibroma
- osteoblastoma
- osteofibrous dysplasia
- stress fracture
- Brodie abscess
- chondroblastoma
- giant cell tumor
- skeletal metastasis
- Ewing sarcoma
- simple bone cyst
Spiculated periosteal reaction
Spiculated periosteal reaction represents spicules of new bone forming along vascular channels and the fibrous bands that anchor tendons to bone (Sharpey fibers). A spiculated periosteal reaction signifies a rapid underlying process that prevents formation of new bone under the raised periosteum.
The orientation of the spicules reflects the direction of tumor growth. Spiculated periosteal reactions can be divided into subtypes based on the orientation of the spicules:
Perpendicular (hair-on-end)
- Ewing sarcoma
- osteosarcoma
- metastasis
Divergent (sunburst)
- osteosarcoma
- hemangioma
- osteoblastic metastasis
- prostatic
- bronchoalveolar
- carcinoid
- breast
- neuroblastoma (pediatric age group)
- osteoblastoma
Focal slopping (velvet)
- chondrosarcoma
Figure 6. Spiculated periosteal reaction
Symmetrical periosteal reaction
There are a large number of causes for a symmetrical periosteal reaction 3:
- chronic venous insufficiency
- hypertrophic osteoarthropathy
- physiologic periostitis, most common cause before 6 months old
- Caffey disease
- juvenile idiopathic arthritis
- pachydermoperiostosis
- congenital syphilis
- fluorosis
- thyroid acropachy
- dysproteinemia
Figure 7. Symmetrical periosteal reaction
Footnote: 5 month baby with irritable, mild fever, tenderness left thigh with visible swelling, was undergoing treatment for osteomyelitis. Lamellated to fusiform periosteal reaction along the shaft of left femur is evident with minimal soft tissue swelling. A subtle finding of periostitis along the right lower ribs is also seen, and child cried everytime he was held due to chest pain.
Generalized periosteal reaction
The list of causes of a generalized periosteal reaction overlaps that of symmetrical periosteal reaction, and includes 3:
- vascular stasis (common)
- congenital syphilis
- fluorosis
- Gaucher disease
- hypertrophic osteoarthropathy
- pachydermoperiostosis
- hypervitaminosis A
- infantile cortical hyperostosis (Caffey disease)
- thyroid acropachy
- tuberous sclerosis
Figure 8. Generalized periosteal reaction
Footnote: Radiographs showing an extensive bilateral periosteal reaction, more on the right side, associated with subcutaneous calcifications. This is a 67 year old female patient with a known history of diabetes mellitus, chronic kidney disease stage 5, and venous insufficiency. She was admitted by nephrology for dialysis and has a history of chronic lower limbs ulcers for more than four years.
Periosteal reaction causes
Periosteal reaction may be seen with the following lesions:
- Osteosarcoma
- Ewing sarcoma
- Osteomyelitis
- Active aneurysmal bone cyst
- Giant cell tumor
- Metastasis
- Chondroblastoma
- Chondrosarcoma (especially juxtacortical chondrosarcoma)
- Malignant fibrous histiocytoma
- Stress fracture
- Spindle cell sarcoma
- Langerhans cell histiocytosis
- Hypertrophic osteoarthropathy
- Early fracture healing
- Osteoid osteoma
- Aneurysmal bone cyst
- Chronic venous insufficiency
- Chondrosarcoma
- Fibrous dysplasia
- Non-ossifying fibroma
- Osteoblastoma
- Osteofibrous dysplasia
- Brodie abscess
- Simple bone cyst
- Chronic venous insufficiency
- Physiologic periostitis, most common cause before 6 months old
- Caffey disease (infantile cortical hyperostosis)
- Juvenile idiopathic arthritis
- Pachydermoperiostosis
- Congenital syphilis
- Fluorosis
- Thyroid acropachy
- Dysproteinemia
- Vascular stasis (common)
- Congenital syphilis
- Gaucher disease
- Hypervitaminosis A
- Tuberous sclerosis
Periosteal reaction treatment
Periosteal reaction treatment involves treating the underlying causes.
References- Wolfgang Dähnert. Radiology Review Manual. (2011) ISBN: 9781609139438
- Selections from the buffet of food signs in radiology. Radiographics. 2002 Nov-Dec;22(6):1369-84. https://doi.org/10.1148/rg.226025521
- Rana RS, Wu JS, Eisenberg RL. Periosteal reaction. AJR Am J Roentgenol. 2009;193 (4): W259-72. doi:10.2214/AJR.09.3300