Reactive gastropathy
Reactive gastropathy refers to a group of endoscopic and histologic findings caused by chemical injury to the gastric mucosa 1. The histologic picture is characterized by foveolar hyperplasia with edema, interfoveolar smooth muscle hyperplasia, erosions, and congestion of superficial capillaries in the lamina propria in the absence of significant inflammation 2. These features were originally described in biopsy specimens obtained from patients who had undergone gastric surgery and were felt to be specific for bile reflux 3. It has since become apparent, however, that the constellation of histologic features seen in reactive gastropathy is a nonspecific response to chemical injury of the gastric mucosa 4. Their respective occurrence in a set of gastric biopsies can be placed on a spectrum of diagnostic certainty that is never absolute because each of such changes can and does occur in other conditions. Although a correlation between histological evidence of chemical gastropathy and clinical manifestations, particularly risk of bleeding, is yet to be documented, reporting the suspicion of drug-induced gastric damage may help clinicians to identify patients that might benefit from change, reduction, or discontinuation of certain medications 5.
Reactive gastropathy has also been referred to as chemical gastropathy, reflux gastritis, and type C gastritis 6. The term “chemical gastropathy” was recommended by the Updated Sydney System 7, because it indicates an underlying chemical injury that is not associated with infection 8.
At present, reactive gastropathy is usually encountered in the clinical setting of chronic nonsteroidal anti-inflammatory drug (NSAID) use. The reported prevalence of reactive gastropathy among patients taking daily NSAIDs for at least 1 month ranges from 30% to 40% 9.
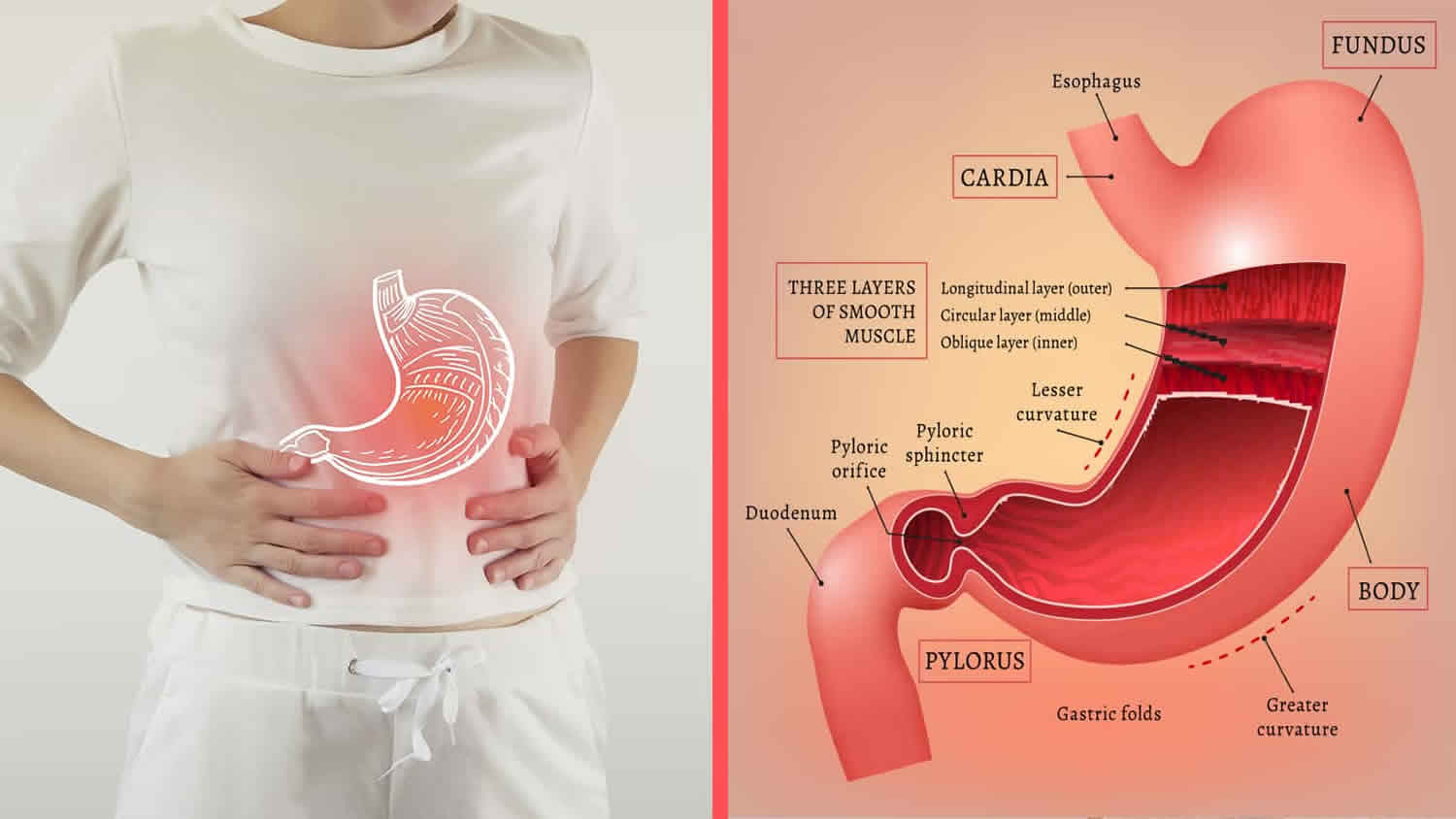
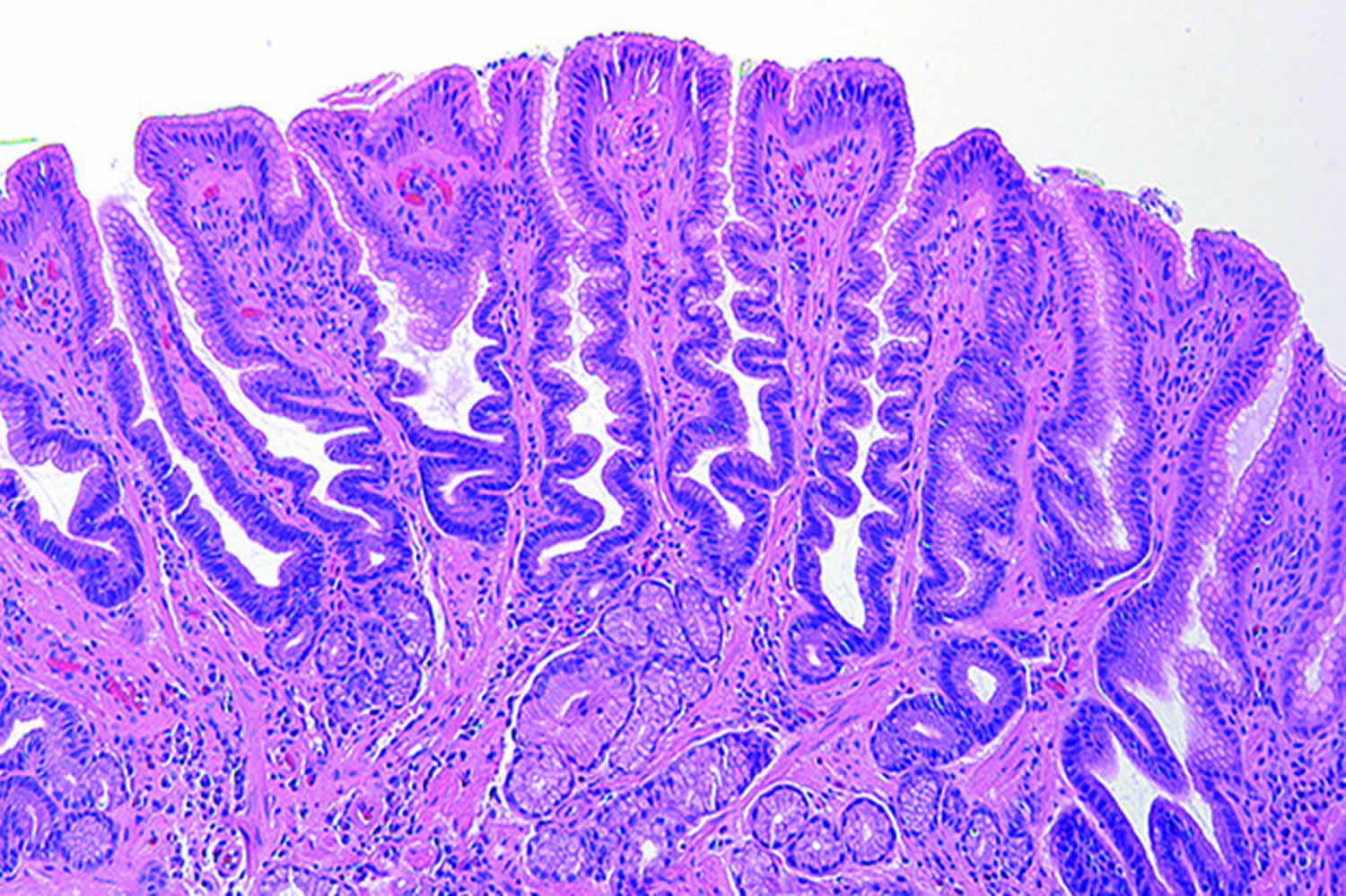
Figure 1. Reactive gastropathy
Footnote: Antral mucosa exhibiting the features of reactive gastropathy, including ‘corkscrew‐like’ foveolar hyperplasia, a mucin depleted epithelium and bundles of hyperplastic smooth muscle arranged perpendicular to the surface.
[Source 10 ]Reactive gastropathy causes
Reactive gastropathy most common causes:
- Ingested agents
- Alcohol
- Drugs
- Aspirin / nonsteroidal anti-inflammatory drugs (NSAIDs)
- Iron and potassium
- Corrosive agents
- Physical injury
- Radiation
- Instrumentation
- Hepatic artery chemotherapy
- Gastrointestinal motility problems
- Prolapse gastropathy
- Post-gastrectomy bile reflux
- Occasionally seen with intact stomach
- Ischemia
- Stress
- Idiopathic
The common underlying causes of reactive gastropathy include chronic bile reflux and long-term intake of nonsteroidal anti-inflammatory drugs (NSAIDs) 2. Bile reflux usually occurs in patients who have undergone a Billroth 2 partial gastrectomy; it is also recognized to occur in intact stomachs in individuals with alcohol abuse, cigarette smoking, chronic respiratory disease, or duodenal ulcer, and even in healthy subjects 11.
The duodenogastric reflux results in disruption of the protective mucus barrier and direct injury to the gastric mucosa, causing backflow of hydrogen ions and epithelial damage 12. The various bile acid species differ in their capacity to cause injury to the gastric mucosa 3. The secondary (deoxycholic and lithocholic) and deconjugated bile acids are more injurious to the gastric mucosa than the primary (colic and chenodeoxycholic) and conjugated bile acids.
In situations of upper gastrointestinal (GI) stasis, as is seen after gastric surgery, bacterial overgrowth occurs within the proximal small intestine. This increase in intraluminal bacteria leads to subsequent generation of relatively increased concentrations of deconjugated and secondary bile acids within the refluxate. The increased concentration of the more toxic forms of bile acid, coupled with the decreased gastric emptying time of the refluxed bile, results in gastric mucosal injury and subsequent reactive gastropathy (chemical gastropathy).
The predominant mechanism of NSAID-induced gastric injury involves decreased synthesis of mucosal prostaglandins 13. Prostaglandins are derived from arachidonic acid via the cyclooxygenase (COX) pathway. Thus, inhibition of COX by NSAIDs reduces prostaglandin synthesis, thereby diminishing mucosal blood flow and decreasing mucus and bicarbonate secretion.
Furthermore, NSAIDs, being weak organic acids, can freely diffuse into the gastric epithelium. As a result of the neutral pH within the surface epithelial cells, the NSAID compound dissociates into its ionized form, contributing to direct cell injury 14.
Although it is known that NSAIDs that selectively inhibit COX-2 cause significantly fewer gastrointestinal complications than nonselective COX inhibitors do, it is still unclear whether administration of selective inhibitors results in less severe reactive gastropathy (chemical gastropathy) 15. However, most of these COX-2 inhibitors have been withdrawn from the market or have had their indications drastically limited in view of their potential serious cardiovascular side effects 16.
The epithelial injury results in excessive exfoliation of the surface epithelial cells, which gives rise to a reactive foveolar hyperplasia 17. The accompanying histamine-mediated vascular response leads to edema and hyperemia. Persistent epithelial damage may result in the release of platelet-derived growth factor (PDGF), which stimulates smooth muscle proliferation, followed by fibroblastic proliferation 12.
The mucosal changes seen in reactive gastropathy are usually most prominent in the antrum and prepyloric region. When associated with bile reflux secondary to partial gastrectomy, the lesions develop near the surgical stoma 18, but the more proximal oxyntic mucosa may also be affected.
To date, no specific genetic predisposing factors for the development of reactive gastropathy have been identified.
Reactive gastropathy symptoms
The clinical features associated with reactive gastropathy are determined by its underlying cause.
Patients with reactive gastropathy secondary to bile reflux typically have an enterogastric anastomosis and most commonly present with continuous burning midepigastric pain that is often exacerbated by food and recumbency. Nausea, bilious vomiting, and other dyspeptic symptoms may also be present 19. Although the findings are not specific, several authors claim that weight loss and a hypochromic microcytic anemia are also associated features 3.
The most common complaint associated with NSAID-induced reactive gastropathy is mild dyspepsia. Chronic consumption of these drugs, however, can lead to the development of erosions and ulcers, increasing the risk for complications such as obstruction, perforation, and bleeding 14.
Reactive gastropathy diagnosis
The endoscopic findings of reactive gastropathy are mostly nonspecific. The mucosa may be normal or may exhibit erythema, congestion, edema, or erosions 8. The bile reflux may be visible 20.
Reactive gastropathy diagnosis is by examination of tissue, e.g. a stomach biopsy.
Reactive gastropathy is characterized, histologically, by 21:
- foveolar hyperplasia with gland tortuosity and dilation,
- smooth muscle hyperplasia in the lamina propria, and
- scant or minimal inflammation, i.e. lack of large numbers of neutrophils and plasma cells.
Reactive gastropathy treatment
If long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) leads to reactive gastropathy, your doctor may recommend that you stop taking NSAIDs, take a lower dose, or take a different medicine for pain. Doctors may also recommend taking a proton pump inhibitor (PPI) and prostaglandin analogues along with NSAIDs to prevent or treat reactive gastropathy and its possible complications.
If bile reflux is causing reactive gastropathy, doctors may prescribe ursodiol, a medicine that contains bile acids and can help heal the stomach lining, or surgery to stop flow of bile into the stomach.
Reactive gastropathy prognosis
Stump carcinoma has been reported in postgastrectomy stomachs. Bile reflux is thought to play a key role in the development of dysplasia and carcinoma in the gastric remnant 22. In fact, some studies have reported improvement of preneoplastic changes after diversion of the enteric reflux 23. Regular endoscopic surveillance starting 10 to 15 years after surgery is recommended.
With the advent of highly effective medical treatment for Helicobacter pylori infection, there has been a decline in such surgical procedures, paralleled by a reduction in the incidence of stump carcinoma 12.
Despite the occasional development of stump carcinomas in postgastrectomy stomachs, reactive gastropathy is not a major risk factor for the development of gastric carcinoma.
References- Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996 Oct. 20(10):1161-81
- Pathology of Reactive Gastropathy. https://emedicine.medscape.com/article/1962893-overview
- Ritchie WP Jr. Alkaline reflux gastritis. Gastroenterol Clin North Am. 1994 Jun. 23(2):281-94.
- Quinn CM, Bjarnason I, Price AB. Gastritis in patients on non-steroidal anti-inflammatory drugs. Histopathology. 1993 Oct. 23(4):341-8.
- Differential diagnosis of reactive gastropathy. Seminars in Diagnostic Pathology Volume 22, Issue 4, November 2005, Pages 273-283
- Sobala GM, King RF, Axon AT, Dixon MF. Reflux gastritis in the intact stomach. J Clin Pathol. 1990 Apr. 43(4):303-6.
- Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol 1996; 20: 1161–81.
- El-Zimaity HM, Genta RM, Graham DY. Histological features do not define NSAID-induced gastritis. Hum Pathol. 1996. 27:1348-54.
- Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999 Jun 17. 340(24):1888-99.
- Reactive gastropathy is associated with inflammatory conditions throughout the gastrointestinal tract. I. Maguilnik W. L. Neumann A Sonnenberg R. M. Genta. Aliment Pharmacol Ther2012;36:736–743 https://doi.org/10.1111/apt.12031
- Maguilnik I, Neumann WL, Sonnenberg A, Genta RM. Reactive gastropathy is associated with inflammatory conditions throughout the gastrointestinal tract. Aliment Pharmacol Ther. 2012 Oct. 36(8):736-43.
- Genta RM. Differential diagnosis of reactive gastropathy. Semin Diagn Pathol. 2005 Nov. 22(4):273-83.
- Iijima K, Iwabuchi T, Ara N, et al. Reactive increase in gastric mucus secretion is an adaptive defense mechanism against low-dose aspirin-induced gastropathy. Dig Dis Sci. 2013 Aug. 58(8):2266-74.
- Schoenfeld P, Kimmey MB, Scheiman J, Bjorkman D, Laine L. Review article: nonsteroidal anti-inflammatory drug-associated gastrointestinal complications–guidelines for prevention and treatment. Aliment Pharmacol Ther. 1999 Oct. 13(10):1273-85.
- Owen DA. Gastritis and carditis. Mod Pathol. 2003 Apr. 16(4):325-41.
- Waxman HA. The lessons of Vioxx–drug safety and sales. N Engl J Med. 2005 Jun 23. 352(25):2576-8.
- Dixon MF, O’Connor HJ, Axon AT, King RF, Johnston D. Reflux gastritis: distinct histopathological entity?. J Clin Pathol. 1986 May. 39(5):524-30.
- Sepulveda AR, Patil M. Practical approach to the pathologic diagnosis of gastritis. Arch Pathol Lab Med. 2008 Oct. 132(10):1586-93.
- Malagelada JR, Phillips SF, Shorter RG, et al. Postoperative reflux gastritis: pathophysiology and long-term outcome after Roux-en-Y diversion. Ann Intern Med. 1985 Aug. 103(2):178-83.
- Vere CC, Cazacu S, Comanescu V, Mogoanta L, Rogoveanu I, Ciurea T. Endoscopical and histological features in bile reflux gastritis. Rom J Morphol Embryol. 2005. 46(4):269-74.
- Genta RM. Differential diagnosis of reactive gastropathy. Semin Diagn Pathol 2005; 22: 273–83.
- Johannesson KA, Hammar E, Stael von Holstein C. Mucosal changes in the gastric remnant: long-term effects of bile reflux diversion and Helicobacter pylori infection. Eur J Gastroenterol Hepatol. 2003 Jan. 15(1):35-40.
- Watt PC, Sloan JM, Spencer A, Kennedy TL. Histology of the postoperative stomach before and after diversion of bile. Br Med J (Clin Res Ed). 1983 Nov 12. 287(6403):1410-2.