What is a spiral fracture
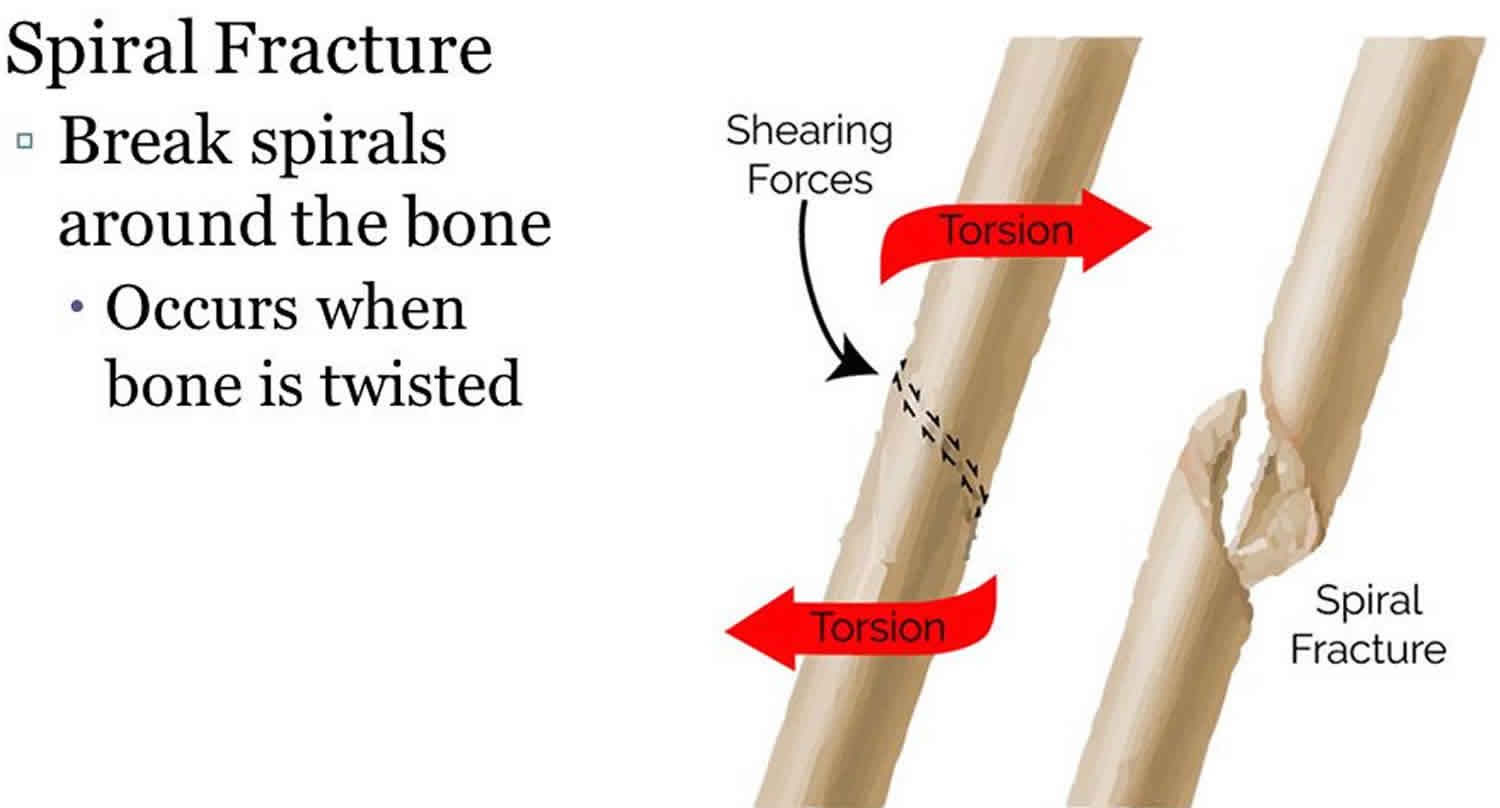
A spiral fracture occurs when a bone is twisted or torqued in one direction and subsequently fractures from the force, causing extreme pain. Spiral fractures are complete fractures of long bones that result from a rotational force applied to the bone. Spiral fractures are usually the result of high energy trauma and are likely to be associated with displacement. Spiral fractures often occur when the body is in motion while one extremity is planted. For example, a spiral fracture of the tibia (the shinbone) can occur in young children when they fall short on an extended leg while jumping. This occurrence is known as “toddler’s fracture”.
Figure 1. Spiral fracture femur (there is a significantly displaced spiral fracture of the proximal femoral shaft with additional avulsion fracture of the lesser trochanter)
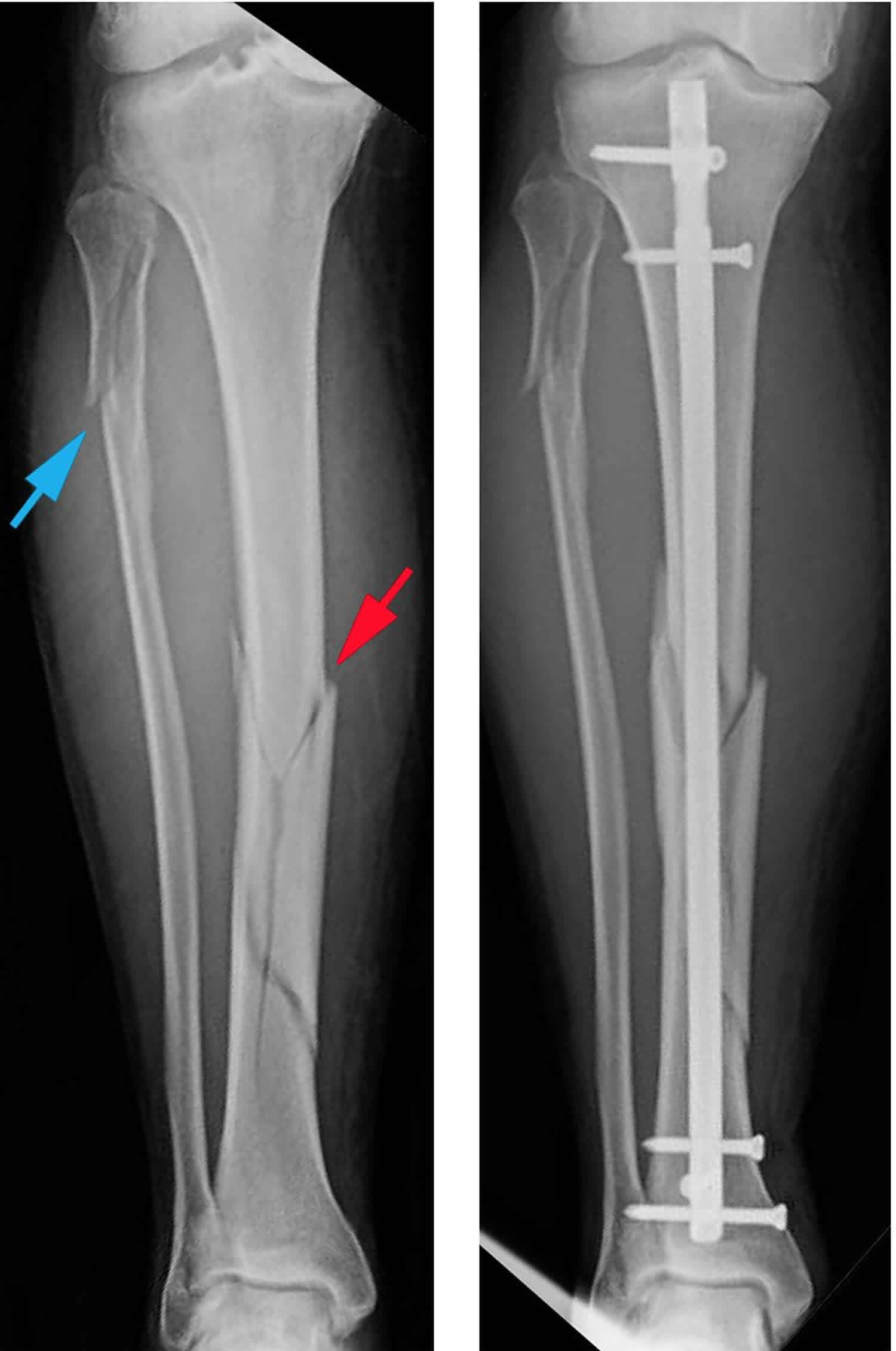
Figure 2. Spiral fracture tibia
Figure 3. Spiral fracture humerus
Figure 4. Spiral fracture fifth metatarsal shaft
Figure 5. Spiral fracture finger (4th and 5th metacarpal shaft)
Spiral fracture causes
The most common cause of spiral fractures is trauma. A fall, a motor vehicle accident, or a tackle during a football game can all result in fractures.
Spiral fracture femur
Femoral shaft fractures in young people are frequently due to some type of high-energy collision. The most common cause of femoral shaft fracture is a motor vehicle or motorcycle crash. Being hit by a car while walking is another common cause, as are falls from heights and gunshot wounds.
A lower-force incident, such as a fall from standing, may cause a femoral shaft fracture in an older person who has weaker bones.
The most common cause of femoral shaft fractures in infants under 1 year old is child abuse. Child abuse is also a leading cause of thighbone fracture in children between the ages of 1 and 4 years, but the incidence is much less in this age group.
In adolescents, motor vehicle accidents (either in cars, bicycles, or as a pedestrian) are responsible for the vast majority of femoral shaft fractures.
Events with the highest risk for pediatric femur fractures include:
- Falling hard on the playground
- Taking a hit in contact sports
- Being in a motor vehicle accident
- Child abuse
Complications from femoral shaft fractures
Femoral shaft fractures can cause further injury and complications.
- The ends of broken bones are often sharp and can cut or tear surrounding blood vessels or nerves, though this is very rare.
- Acute compartment syndrome may develop. This is a painful condition that occurs when pressure within the muscles builds to dangerous levels. This pressure can decrease blood flow, which prevents nourishment and oxygen from reaching nerve and muscle cells. Unless the pressure is relieved quickly, permanent disability may result. This is a surgical emergency. During the procedure, your surgeon makes incisions in your skin and the muscle coverings to relieve the pressure.
- Open fractures expose the bone to the outside environment. Even with good surgical cleaning of the bone and muscle, the bone can become infected. Bone infection is difficult to treat and often requires multiple surgeries and long-term antibiotics.
- Occasionally, the ligaments around the knee can be injured during a femoral shaft fracture. If you have knee pain after surgery, tell your doctor.
Spiral fracture tibia
Tibial shaft fractures are often caused by some type of high-energy collision, such as a motor vehicle or motorcycle crash. In cases like these, the bone can be broken into several pieces (comminuted fracture).
Sports injuries, such as a fall while skiing or a collision with another player during soccer, are lower-energy injuries that can cause tibial shaft fractures. These fractures are typically caused by a twisting force and result in an oblique or spiral fracture.
Complications from tibial shaft fractures
Tibial shaft fractures can cause further injury and complications, including the following:
- The ends of broken bones are often sharp and can cut or tear surrounding muscles, nerves, or blood vessels.
- Acute compartment syndrome may develop. This is a painful condition that occurs when pressure within the muscles builds to dangerous levels. This pressure can decrease blood flow, which prevents nourishment and oxygen from reaching nerve and muscle cells. Unless the pressure is relieved quickly, permanent disability may result. This is a surgical emergency. During the procedure, your surgeon makes incisions in your skin and the muscle coverings to relieve pressure.
- Open fractures expose the bone to the outside environment. Even with good surgical cleaning of the bone and muscle, the bone can become infected. Bone infection is difficult to treat and often requires multiple surgeries and long-term antibiotics.
Spiral fracture symptoms
Many fractures are very painful and may prevent you from moving the injured area. Other common symptoms include:
- Swelling and tenderness around the injury
- Bruising
- Deformity — a limb may look “out of place” or a part of the bone may puncture through the skin
A femoral shaft fracture usually causes immediate, severe pain. You will not be able to put weight on the injured leg, and it may look deformed—shorter than the other leg and no longer straight.
A tibial shaft fracture usually causes immediate, severe pain. Other symptoms may include:
- Inability to walk or bear weight on the leg
- Deformity or instability of the leg
- Bone “tenting” over the skin at the fracture site or bone protruding through a break in the skin
- Occasional loss of feeling in the foot
Spiral fracture diagnosis
Spiral fracture femur diagnosis
Medical History and Physical Examination
It is important that your doctor know the specifics of how you hurt your leg. For example, if you were in a car accident, it would help your doctor to know how fast you were going, whether you were the driver or a passenger, whether you were wearing your seat belt, and if the airbags went off. This information will help your doctor determine how you were hurt and whether you may be hurt somewhere else.
It is also important for your doctor to know if you have any other health conditions, such as high blood pressure, diabetes, asthma, or allergies. Your doctor will also ask you if you use tobacco products or are taking any medications.
After discussing your injury and medical history, your doctor will do a careful examination. He or she will assess your overall condition, and then focus on your leg. Your doctor will look for:
- An obvious deformity of the thigh/leg (an unusual angle, twisting, or shortening of the leg)
- Breaks in the skin
- Bruises
- Bony pieces that may be pushing on the skin
After the visual inspection, your doctor will feel along your thigh, leg, and foot looking for abnormalities and checking the tightness of the skin and muscles around your thigh. He or she will also feel for pulses. If you are awake, your doctor will test for sensation and movement in your leg and foot.
Imaging Tests
Imaging tests will provide your doctor with more information about your injury.
- X-rays. The most common way to evaluate a fracture is with x-rays, which provide clear images of bone. X-rays can show whether a bone is intact or broken. They can also show the type of fracture and where it is located within the femur.
- Computerized tomography (CT) scans. If your doctor still needs more information after reviewing your x-rays, he or she may order a CT scan. A CT scan shows a cross-sectional image of your limb. It can provide your doctor with valuable information about the severity of the fracture. For example, sometimes the fracture lines can be very thin and hard to see on an x-ray. A CT scan can help your doctor see the lines more clearly.
Spiral fracture tibia diagnosis
Medical History and Physical Examination
It is important that your doctor know the specifics of how you hurt your leg. For example, if you were in a car accident, it would help your doctor to know how fast you were going, whether you were the driver or the passenger, whether you were wearing your seatbelt, and if the airbags went off. This information will help your doctor determine how you were hurt and whether you may be hurt somewhere else.
It is also important for your doctor to know if you have any other health conditions like high blood pressure, diabetes, asthma, or allergies. Your doctor will also ask you if you use tobacco products or are taking any medications.
After discussing your injury and medical history, your doctor will perform a careful examination. He or she will assess your overall condition and then focus on your leg. Your doctor will look for:
- An obvious deformity of the tibia/leg (an unusual angle, twisting, or shortening of the leg)
- Breaks in the skin
- Bruises
- Swelling
- Bony pieces that may be pushing on the skin
- Instability (some patients may retain a degree of stability if the fibula is not broken or if the fracture is incomplete)
After the visual inspection, your doctor will feel along your tibia, leg, and foot looking for abnormalities. If you are awake and alert, your doctor will test for sensation and movement in your leg and foot.
Imaging Tests
Imaging tests will provide your doctor with more information about your injury.
- X-rays. The most common way to evaluate a fracture is with x-rays, which provide clear images of bones. X-rays can show whether the tibia is broken or intact. They can also show the type of fracture and where it is located within the tibia. X-rays are also useful for identifying the involvement of the knee or ankle joints and the presence of a fibula fracture.
- Computed tomography (CT) scans. If your doctor still needs more information after reviewing your x-rays, he or she may order a CT scan. A CT scan shows a cross-sectional image of your limb. It can provide your doctor with valuable information about the severity of the fracture. For example, sometimes the fracture lines can be very thin and hard to see on an x-ray. A CT scan can help your doctor see the lines more clearly.
Spiral fracture treatment
Spiral fracture femur treatment for adults
Nonsurgical Treatment
Most femoral shaft fractures require surgery to heal. It is unusual for femoral shaft fractures to be treated without surgery. Very young children are sometimes treated with a cast.
Surgical Treatment
Timing of surgery. Most femur fractures are fixed within 24 to 48 hours. On occasion, fixation will be delayed until other life-threatening injuries or unstable medical conditions are stabilized. To reduce the risk of infection, open fractures are treated with antibiotics as soon as you arrive at the hospital. The open wound, tissues, and bone will be cleaned during surgery.
For the time between initial emergency care and your surgery, your doctor may place your leg either in a long-leg splint or in traction. This is to keep your broken bones as aligned as possible and to maintain the length of your leg.
Skeletal traction is a pulley system of weights and counterweights that holds the broken pieces of bone together. It keeps your leg straight and often helps to relieve pain.
External fixation. In this type of operation, metal pins or screws are placed into the bone above and below the fracture site. The pins and screws are attached to a bar outside the skin. This device is a stabilizing frame that holds the bones in the proper position.
External fixation is usually a temporary treatment for femur fractures. Because they are easily applied, external fixators are often put on when a patient has multiple injuries and is not yet ready for a longer surgery to fix the fracture. An external fixator provides good, temporary stability until the patient is healthy enough for the final surgery. In some cases, an external fixator is left on until the femur is fully healed, but this is not common.
Intramedullary nailing. Currently, the method most surgeons use for treating femoral shaft fractures is intramedullary nailing. During this procedure, a specially designed metal rod is inserted into the canal of the femur. The rod passes across the fracture to keep it in position.
An intramedullary nail can be inserted into the canal either at the hip or the knee. Screws are placed above and below the fracture to hold the leg in correct alignment while the bone heals.
Intramedullary nails are usually made of titanium. They come in various lengths and diameters to fit most femur bones.
Plates and screws. During this operation, the bone fragments are first repositioned (reduced) into their normal alignment. They are held together with screws and metal plates attached to the outer surface of the bone.
Plates and screws are often used when intramedullary nailing may not be possible, such as for fractures that extend into either the hip or knee joints.
Complications from surgery
In addition to the risks of surgery in general, such as blood loss or problems related to anesthesia, complications of surgery may include:
- Infection
- Injury to nerves and blood vessels
- Blood clots
- Fat embolism (bone marrow enters the blood stream and can travel to the lungs; this can also happen from the fracture itself without surgery)
- Malalignment or the inability to correctly position the broken bone fragments
- Delayed union or nonunion (when the fracture heals slower than usual or not at all)
- Hardware irritation (sometimes the end of the nail or the screw can irritate the overlying muscles and tendons)
Spiral fracture femur treatment for children
To treat a child’s femoral shaft fracture, the pieces of bone are realigned and held in place for healing. Treatment depends on many factors, such as your child’s age and weight, the type of fracture, how the injury happened, and whether the broken bone pierced the skin.
Nonsurgical Treatment
In some thighbone fractures, the doctor may be able to manipulate the broken bones back into place without an operation (closed reduction). In a baby under 6 months old, a brace (called a Pavlik Harness) may be able to hold the broken bone still enough for successful healing.
Spica casting. In children between 7 months and 5 years old, a spica cast is often applied to keep the fractured pieces in correct position until the bone is healed.
There are different types of spica casts, but, in general, a spica cast begins at the chest and extends all the way down the fractured leg. The cast may also extend down the uninjured leg, or stop at the knee or hip. Your doctor will decide which type of spica cast is most effective for treating your child’s fracture.
Your doctor will sedate your child for the closed reduction, and apply a spica cast immediately (or within 24 hours of hospitalization) to keep the fractured pieces in correct position until healing occurs.
When a bone breaks and is displaced, the pieces often overlap and shorten the normal length of the bone. Because children’s bones grow quickly, your doctor may not need to manipulate the pieces back into perfect alignment. While in the cast, the bones will grow and heal back into a more normal shape.
In general, for the best results, the broken pieces should not overlap more than 2 cm when in the cast. The growth of the thighbone may be temporarily increased by the trauma. The mild shortening from the overlap will resolve.
Traction. If the shortening of the bones is too much (more than 3 cm) or if the bone is too crooked in the cast, it may be helpful to put the leg in a weight and counterweight system (traction) to make sure the bones are properly realigned.
Surgical treatment
Doctors generally agree that displaced femur fractures that have shortened more than 3 cm are not acceptable and require treatment to correct at least a portion of the shortening.
In some more complicated injuries, the doctor may need to surgically realign the bone and use an implant to stabilize the fracture.
Doctors are treating pediatric thighbone fractures more often with surgery than in previous years due to the benefits that have been recognized. These include earlier mobilization, faster rehabilitation, and shorter time spent in the hospital.
In children between 6 and 10 years old, flexible intramedullary (inside the bone) nails are often used to stabilize the fracture. Over the past decade, this treatment method has gained great acceptance.
Occasionally, the broken bone has too many pieces and cannot be treated successfully with flexible nails. Other options that can lead to successful outcomes in this situation include:
- A plate with screws that “bridges” the fractured segments
- An external fixator — this is often used if there has been a large open injury to the skin and muscles
- Prolonged traction with a pin temporarily placed into the thighbone
As the child nears the teenage years (11 years to skeletal maturity), the most common treatment choices include either flexible intramedullary nails or a rigid locked intramedullary nail. The rigid nail is particularly useful when the fracture is unstable. Both types of nails allow for the child to begin walking immediately.
Spiral fracture tibia treatment
In planning your treatment, your doctor will consider several things, including:
- Your overall health
- The cause of your injury
- The severity of your injury
- The extent of soft tissue damage
Nonsurgical treatment
Nonsurgical treatment may be recommended for patients who:
- Are poor candidates for surgery due to their overall health problems
- Are less active, so are better able to tolerate small degrees of angulation or differences in leg length
- Have closed fractures with minimal movement of the fracture ends
Initial treatment. Most injuries cause some swelling for the first few weeks. Your doctor may initially apply a splint to provide comfort and support. Unlike a full cast, a splint can be tightened or loosened to allow swelling to occur safely. Once the swelling goes down, your doctor will consider a range of treatment options.
Casting and bracing. Your doctor may immobilize the fracture in a cast for initial healing. After several weeks, the cast can be replaced with a functional brace made of plastic and fasteners. The brace will provide protection and support until healing is complete. The brace can be taken off for hygiene purposes and for physical therapy.
Surgical treatment
Surgery may be recommended for certain types of fractures, including:
- Open fractures with wounds that need monitoring
- Fractures that have not healed with nonsurgical treatment
- Fractures with many bone fragments and a large degree of displacement
Intramedullary nailing. Currently, the method most surgeons use for treating tibia fractures is intramedullary nailing. During this procedure, a specially designed metal rod is inserted into the canal of the tibia. The rod passes across the fracture to keep it in position.
The intramedullary nail is screwed to the bone at both ends. This keeps the nail and the bone in proper position during healing.
Intramedullary nails are usually made of titanium. They come in various lengths and diameters to fit most tibia bones.
Intramedullary nailing is not ideal for fractures in children and adolescents because care must be taken to avoid crossing the bone’s growth plates.
Plates and screws. During this operation, the bone fragments are first repositioned (reduced) into their normal alignment. They are held together with screws and metal plates attached to the outer surface of the bone.
Plates and screws are often used when intramedullary nailing may not be possible, such as for fractures that extend into either the knee or ankle joints.
External fixation. In this type of operation, metal pins or screws are placed into the bone above and below the fracture site. The pins and screws are attached to a bar outside the skin. This device is a stabilizing frame that holds the bones in the proper position so they can heal.
Complications from surgery
In addition to the risks of surgery in general, such as blood loss and problems related to anesthesia, complications of surgery may include:
- Infection
- Injury to nerves and blood vessels
- Blood clots (these may also occur without surgery)
- Malalignment or the inability to correctly position the broken fragments
- Delayed union or nonunion (when the fracture heals slower than usual or not at all)
- Angulation (with treatment by external fixation).
Spiral fracture finger treatment
Nonsurgical treatment
Your doctor will put your broken bone back into place, usually without surgery. You will get a splint or cast to hold your finger straight and protect it from further injury while it heals. Sometimes your doctor may splint the fingers next to the fractured one to provide additional support. Your doctor will tell you how long to wear the splint. Usually a splint on a fractured finger is worn for about 3 weeks. You may need more x-rays over this time so that your doctor can monitor the progress of your finger as it heals.
Surgical treatment
Depending on the type and severity of the fracture, you may need surgery to put the bones into alignment. Small devices, such as pins, screws, or wire, will be used to hold your fractured bones together.
Rehabilitation
You may begin using your hand again as soon as your doctor determines it is okay to move your finger. Doing simple rehabilitation exercises each day will help reduce the finger’s stiffness and swelling. You may be required to see a physical therapist to assist you in these exercises.
Spiral fracture recovery time
Spiral fracture femur recovery time
Most femoral shaft fractures take 3 to 6 months to completely heal. Some take even longer, especially if the fracture was open or broken into several pieces or if the patient uses tobacco products.
Generally, children who sustain a thighbone fracture will heal well, regain normal function, and have legs that are equal in length. The intramedullary nails may need to be removed following healing if they cause irritation of the skin and tissues underneath.
Occasionally, children will require further treatment, either early on or in subsequent years, if they have a significant difference in the length of the legs, unacceptable angulation of the healed bone, abnormal rotation of the healed bone, infection, or (rarely) if a thighbone fracture persists (nonunion).
These problems can nearly always be resolved with further treatment.
Weight bearing
Many doctors encourage leg motion early on in the recovery period. It is very important to follow your doctor’s instructions for putting weight on your injured leg to avoid problems.
In some cases, doctors will allow patients to put as much weight as possible on the leg right after surgery. However, you may not be able to put full weight on your leg until the fracture has started to heal. Be sure to follow your doctor’s instructions carefully.
When you begin walking, you will probably need to use crutches or a walker for support.
Physical Therapy
Because you will most likely lose muscle strength in the injured area, exercises during the healing process are important. Physical therapy will help to restore normal muscle strength, joint motion, and flexibility. It can also help you manage your pain after surgery.
A physical therapist will most likely begin teaching you specific exercises while you are still in the hospital. The therapist will also help you learn how to use crutches or a walker.
Spiral fracture tibia recovery time
Most tibial shaft fractures take 4 to 6 months to heal completely. Some take even longer, especially if the fracture was open or broken into several pieces or if the patients uses tobacco products.
Weight bearing
Many doctors encourage leg motion early in the recovery period. It is very important to follow your doctor’s instructions for putting weight on your injured leg to avoid problems.
In some cases, doctors will allow patients to put as much as weight as possible on the leg right after surgery. However, you may not be able to put full weight on your leg until the fracture has started to heal. Be sure to follow your doctor’s instructions carefully.
When you begin walking, you will probably need to use crutches or a walker for support.
Physical therapy
Because you will likely lose muscle strength in the injured area, exercises during the healing process are important. Physical therapy will help to restore normal muscle strength, joint motion, and flexibility. It can also help you manage your pain after surgery.
A physical therapist will most likely begin teaching you specific exercises while you are still in the hospital. The therapist will also help you learn how to use crutches or a walker.