Spondylolysis
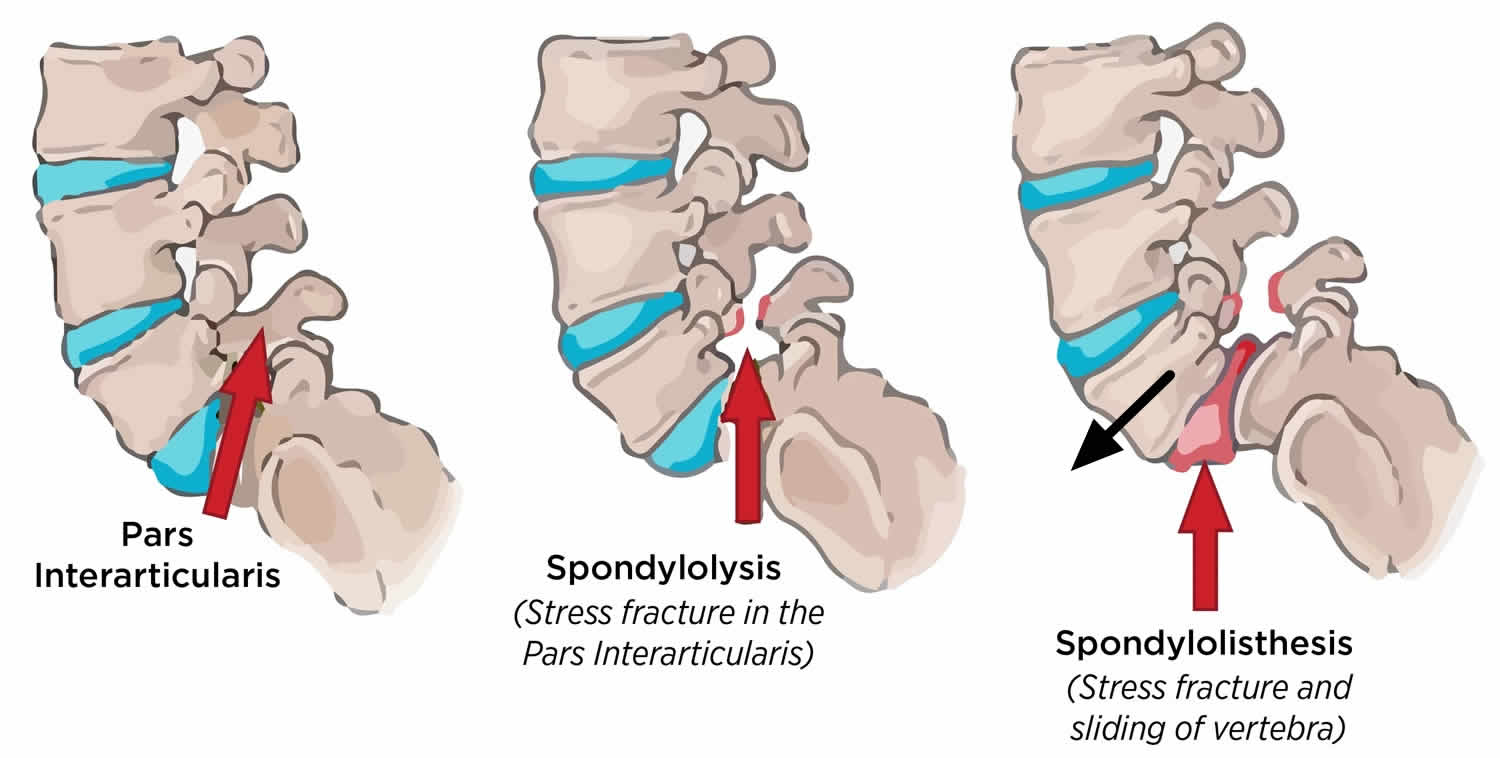
Spondylolysis also known as pars interarticularis defect, pars defect or pars fracture, is a unilateral or bilateral defect in the region of the pars interarticularis (a small thin portion of the vertebra that connects the upper and lower facet joints), which may or may not be accompanied by vertebral displacement, and is most commonly the result of repetitive trauma to the growing immature skeleton of a genetically susceptible individual 1. The pars interarticularis is the bony bridge between the junction of the pedicle, the lamina, the superior (upper) and the inferior (lower) articular processes (Figures 2, 3 and 4). The pars interarticularis is subject to a significant amount of force that is transmitted from the vertically oriented lamina to the horizontally oriented pedicle 2. Spondylolysis is considered a stress fracture of the pars interarticularis, that most often occurs in children and adolescents who participate in sports that involve repeated stress on the lower back, such as gymnastics, football, and weight lifting 3. In some cases, the stress fracture weakens the bone so much that it is unable to maintain its proper position in the spine and the vertebra starts to shift or slip out of place. This condition is called spondylolisthesis (see Figure 7). It is important to note unilateral spondylolysis rarely progress to spondylolisthesis 4, 5. However, in patients with bilateral spondylolysis, at the time of diagnosis, 50% to 75% will already have accompanying spondylolisthesis. These results suggest that the prognosis of unilateral spondylolysis is more favorable than that of bilateral spondylolysis. Lemoine et al. 6 reported that the prevalence of bilateral spondylolysis increased after children have learned to walk. However, Brooks et al. 7 reported that the prevalence of lumbar spondylolysis does not increase in patients older than 20 years. Therefore, it is generally recognized that spondylolysis occurs in adolescent under the age of 20 years. In contrast, the prevalence of spondylolisthesis would increase depending on age 8.
Slip progression is more common in adolescents compared to adults, and although the incidence of spondylolysis is more common in males, the slip progression of spondylolisthesis occurs more frequently in females. Roche and Rowe’s study 9 demonstrated between 20 and 80 years of age there is no evidence of increased incidence of pars defects, suggesting the highest risk is through adolescents, after which time the bones have fully ossified and risk plateaus.
Ninty percent of the cases of spondylolysis occur at the fifth lumbar vertebra (L5) vertebra with decreasing incidence at progressively higher lumbar levels 1 and may be observed as high as L2 10.
Lumbosacral spondylolysis (lumbar spondylolysis) occurs in 3-7% of the general population 11. The athletic population is believed to be more prone to the development of this condition 12, because the incidence of lumbosacral spondylolysis (lumbar spondylolysis) in competitive athletes is higher than the percentage reported for the nonsports population 13.
Lumbosacral spondylolysis (lumbar spondylolysis) is more commonly observed in males 14, but this difference may not be significant 11. The prevalence of spondylolysis is 4% by age 6 and 6% by age 14, a value that remains consistent into adulthood, with a mean age at diagnosis in athletes of about 15-16 years 14.
In the United States, a reported difference exists between the sexes and races, with an incidence of lumbosacral spondylolysis (lumbar spondylolysis) of 6.4% in white men, 2.8% in black men, 2.3% in white women, and 1.1% in black women. A pars defect is twice as common in boys than in girls, although high-grade slippage is 4 times more common in girls than in boys. Alaskan Eskimos (26%) have the highest incidence, with the highest rate in Eskimos from north of the Yukon River 15.
Spondylolysis is commonly asymptomatic. Approximately 25% of individuals with spondylolysis have symptoms at some time.
Spondylolysis is a common cause of low back pain in adolescents and may be the cause of low back pain in ~50% of adolescent athletes 16. Micheli and Wood 17 reported that spondylolysis was the most common cause of diagnosable low back pain, accounting for 47% of cases of low back pain in young athletes.
In teens, the main symptom is low back pain that worsens with activity (extension and/or rotation of the lumbar spine) and improves with avoiding the sport/activity that causes repeated back bending. Symptoms can progress to interfere with normal daily activities.
85% of patients with spondylolysis will progress to spondylolisthesis 18, which is seen radiographically in ~25% of patients with spondylolysis 19. In most patients this occurs before the age of 16.
Spondylolysis may also be associated with spina bifida occulta and idiopathic scoliosis: ~5% 20.
For most patients with spondylolysis and spondylolisthesis, back pain and other symptoms will improve with conservative treatment. This always begins with a period of rest from sports and other strenuous activities.
Spondylolysis nonsurgical treatment may include:
- Rest. Avoiding sports and other activities that place excessive stress on the lower back for a period of time can often help improve back pain and other symptoms.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs such as ibuprofen and naproxen can help reduce swelling and relieve back pain.
- Chiropractic care.
- Physical therapy. Specific exercises can help improve flexibility, stretch tight hamstring muscles, and strengthen muscles in the back and abdomen.
- Bracing. Some patients may need to wear a back brace for a period of time to limit movement in the spine and allow a recent pars fracture the opportunity to heal 21, 22. Although athletes with sudden or acute onset of pain are candidates for brace treatment, patients with longer-term pain are not. In these patients, the stress fracture will have a low chance of healing, even after several months in a brace. In some cases, patients resist accepting long-term conservative treatment because they do not want to stop playing sports. Thus, some patients abandon the treatment that could achieve bony union. As a result, the fracture does not heal and it becomes a pseudoarthrosis (pseudoarthrotic spondylolysis) 21. However, a recent meta-analysis found 83% of patients treated non-operatively improve clinically regardless of bracing.
Over the course of treatment, your child’s doctor will take periodic X-rays to determine whether the vertebra is changing position.
Surgery is only considered in rare circumstances as most cases respond to conservative management 18. Incomplete fractures demonstrate good healing rates with conservative management 16.
Vertebra anatomy
Your spine is made up of 24 small rectangular-shaped bones, called vertebrae, which are stacked on top of one another. These bones connect to create a canal that protects the spinal cord.
The five vertebrae in the lower back comprise the lumbar spine.
Each individual vertebra has unique features depending on the region in which it is found. Every vertebra, regardless of location, has three basic functional parts: (1) the drum-shaped vertebral body, designed to bear weight and withstand compression or loading; (2) the posterior (backside) arch, made of the lamina, pedicles and facet joints; and (3) the transverse processes, to which muscles attach.
Other parts of your spine include:
Spinal cord and nerves
These “electrical cables” travel through the spinal canal carrying messages between your brain and muscles. Nerve roots branch out from the spinal cord through openings in the vertebrae.
Facet joints
Between the back of the vertebrae are small joints that provide stability and help to control the movement of the spine. The facet joints work like hinges and run in pairs down the length of the spine on each side.
Intervertebral disks
In between the vertebrae are flexible intervertebral disks. These disks are flat and round and about a half inch thick. Intervertebral disks cushion the vertebrae and act as shock absorbers when you walk or run.
The vertebral body
The vertebral body is composed of hard cortical bone on the outside and less dense cancellous bone on the inside. The top and bottom of the vertebral body are called the end plates. The intervertebral disc, sandwiched between two vertebral bodies, is attached to the end plates. Changes in the disc may be accompanied by changes in the end plates.
The pedicle is a paired, strong, tubular bony structure made of hard cortical bone on the outside and cancellous bone on the inside. Each pedicle comes out of the side of the vertebral body and projects to the back. Pedicles act as the lateral (side) walls of the bony spinal canal that protects the spinal cord and cauda equina, or nerve roots, in the lumbar region. There is also a space created between the facet joints and pedicles of one vertebral body and the next, called the intervertebral foramen, through which the spinal nerves branch out to the rest of your body.
The lamina are shingle-like plates of bone coming from the pedicles to arch over the nerves and join at the midline. The lamina are shorter than the vertebral bodies so that there is a gap between any two laminae, bridged by soft tissue called the ligamentum flavum. This provides additional protection for the nerves that lie underneath it. Together, the lamina and pedicles form the vertebral arch.
As the lamina come together at the back of the spinal column, they join to form the spinous process, the bony part of the spine that you can feel at the midline when you rub your back. There is an interspinous ligament that runs between the spinous processes of the vertebrae and a supraspinous ligament that runs on top of them from the cervical region to the sacrum.
Each vertebral body has two articular processes at the top and bottom where the lamina and pedicle meet. These articular processes create a joint, called the facet joint, between the stacked vertebral bodies. There is a facet joint on each side of the vertebral body. The facet joint typically lies behind the spinal nerves as they emerge from the central spinal canal. The surfaces of the facet joint are capped with cartilage and the joint is contained in a capsule lined by synovium, much like the knee joint. The two facet joints and the intervertebral disc at each level allow for motion between the vertebral bodies.
The typical vertebral body has two transverse processes, or lateral projections, one on each side. These projections serve as points of attachment for muscles and ligaments in the spine. In the cervical spine, the transverse processes each have a foramen or canal through which the vertebral artery and vein travel. The intertransverse ligaments connect the transverse processes of the vertebrae on each side of the spinal column.
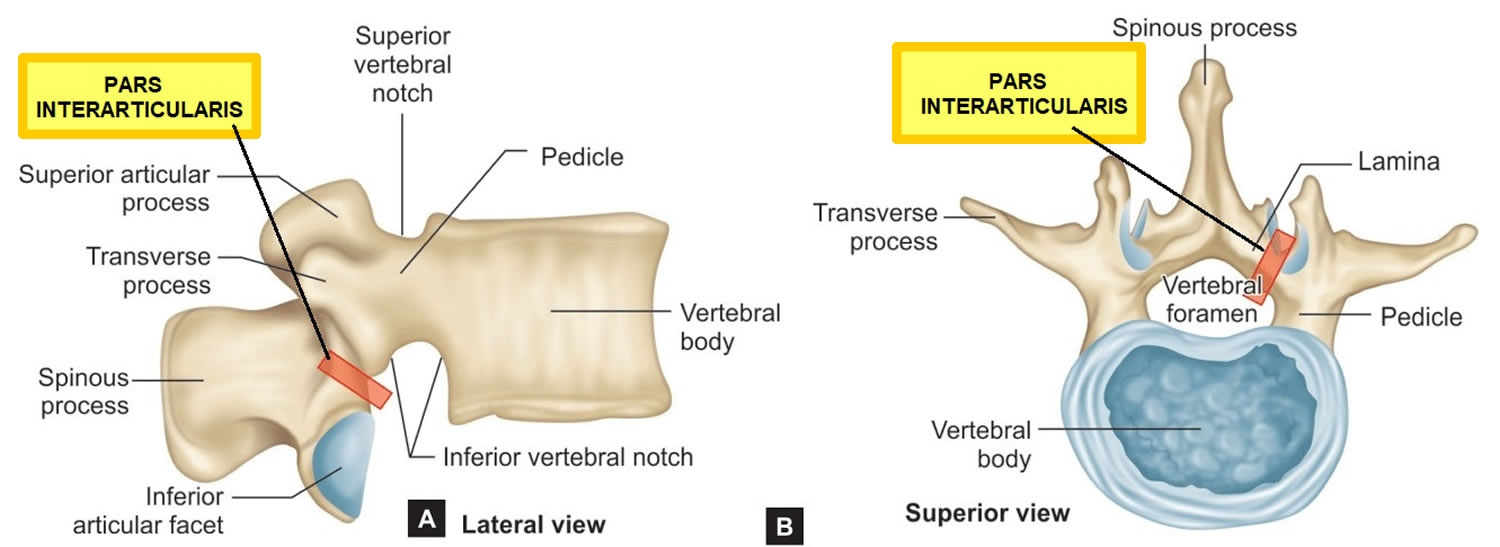
In the lumbar spine, identification of the pars interartcularis is important because it is the site of pathology related to spondylolisthesis, or “slipped vertebra.” This is another paired structure on the back side of the spine and it links the pedicle, transverse process, lamina and articular facets on each side of the vertebrae.
Figure 1. Lumbar vertrebrum (looking from above)
Figure 2. Lumbar vertebrae anatomy (looking from behind and from the side)
Figure 3. Pars interarticularis
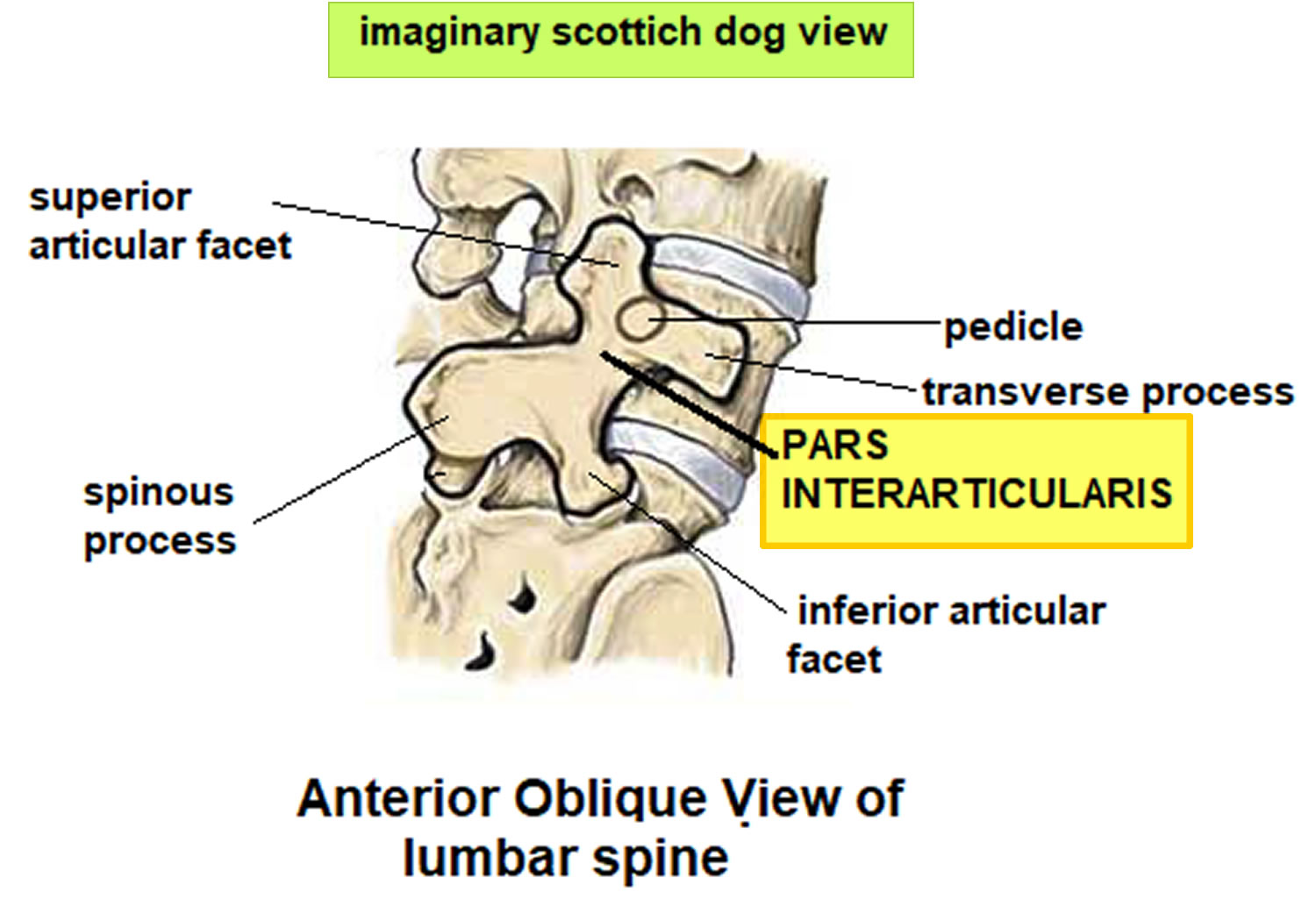
Figure 4. Pars interarticularis oblique view showing the imaginary “Scottish dog”
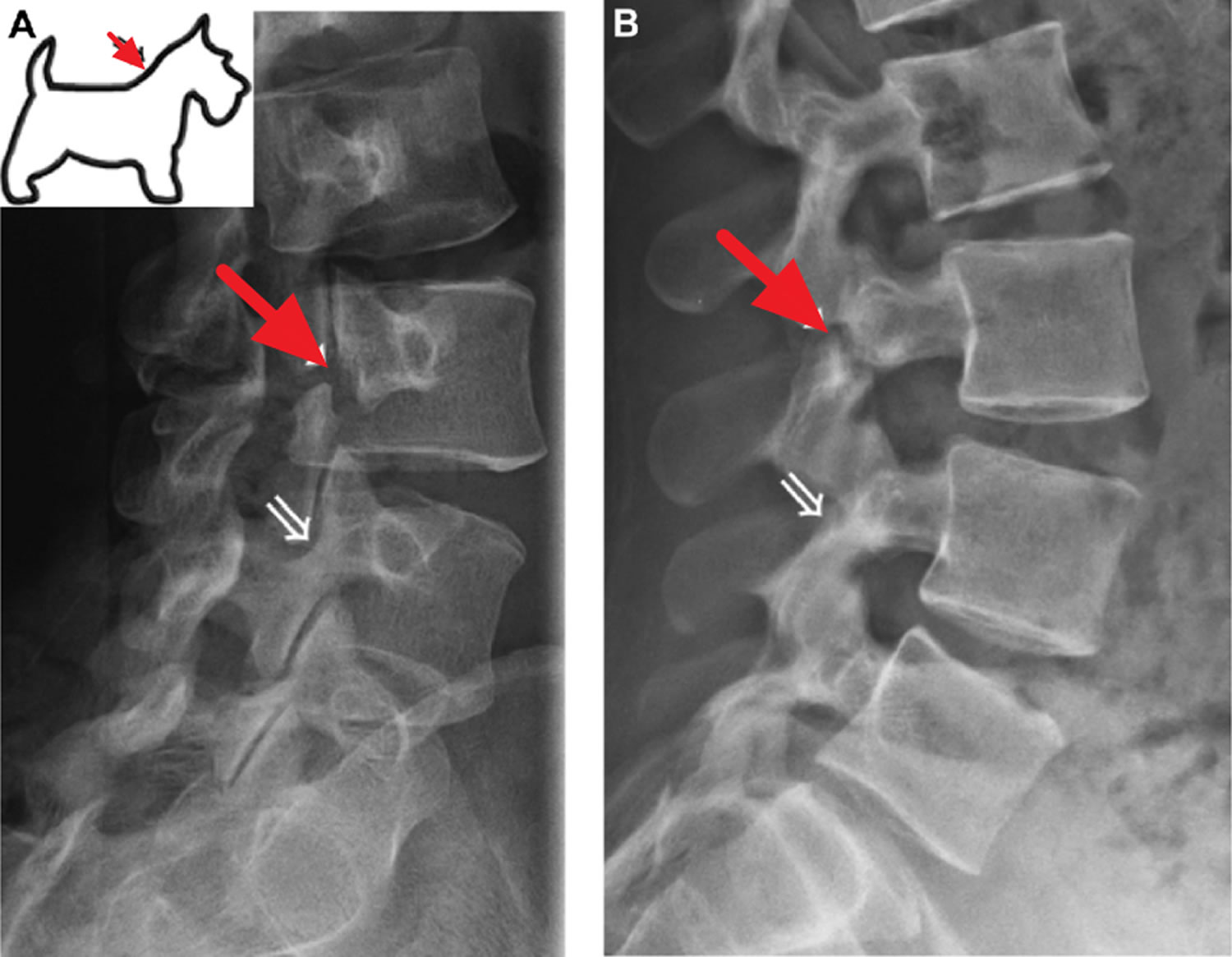
Figure 5. Pars interarticularis defect (the Collar sign in spondylolysis refers to a break in the pars interarticularis of the vertebra on oblique radiographs that can have the appearance of a collar around the Scotty dog’s neck)
Footnote: Right-sided pars interarticularis defect at L3 (red arrow) on oblique (A) and lateral (B) radiographs of the lumbar spine. A normal right L4 pars interarticularis is marked with white arrow on the radiographs and on a representative artistic rendition of the Scottie dog’s neck.
[Source 23 ]Figure 6. Spondylolysis
Footnote: There is a break in the left pars interarticularis of the L4 vertebra on the oblique radiograph that resembles a collar around the Scotty dog’s neck. A suspected break is also noted in the left pars interarticularis of the L5 vertebra.
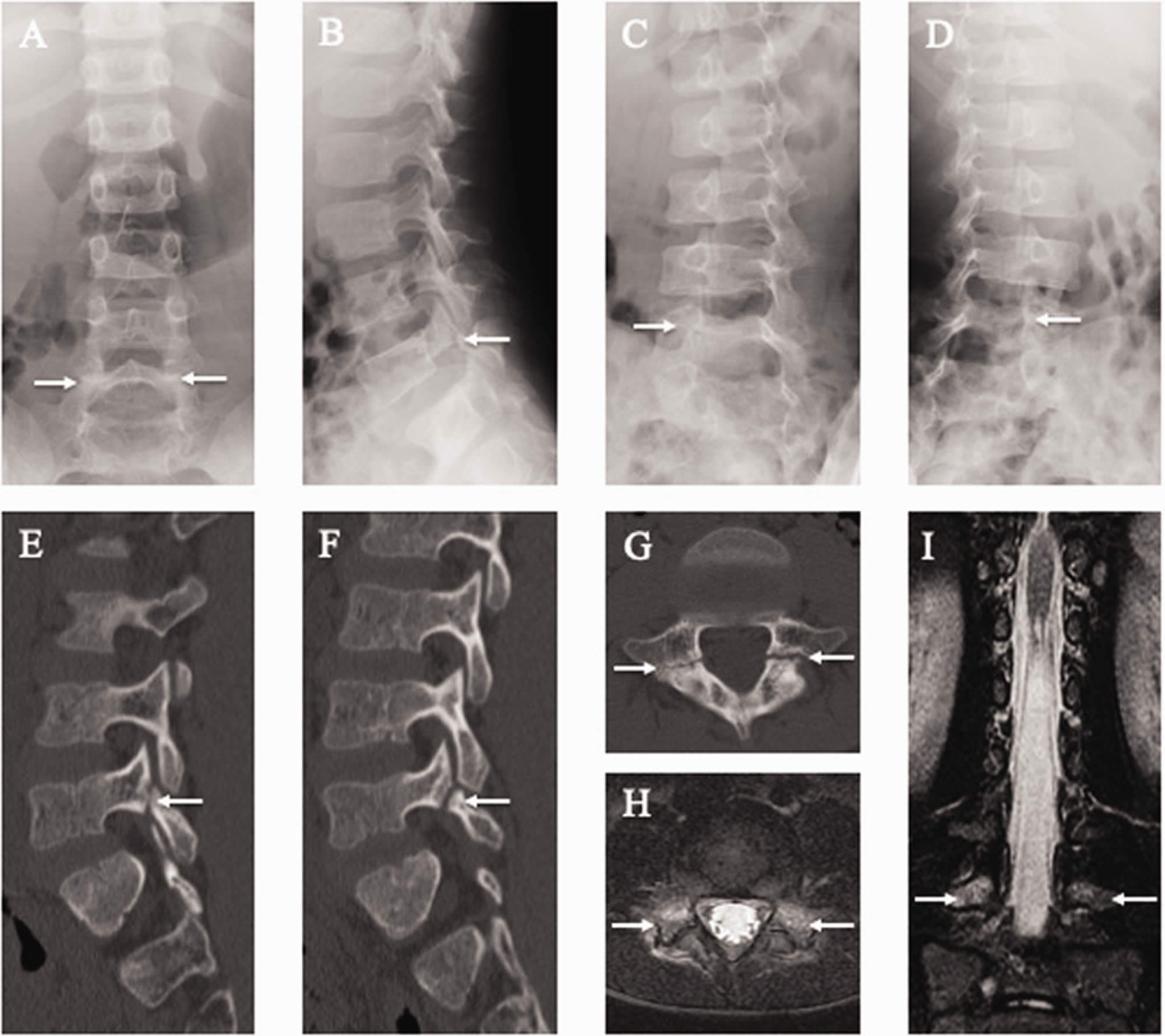
[Source 24 ]Figure 7. Spondylolysis and spondylolisthesis
Figure 8. Pars interarticularis stress fracture
Footnotes: Results of lumbar spine radiography, computed tomography (CT), and magnetic resonance imaging (MRI) of the 7-year-old boy. Spondylolysis (white arrows) is observed at the fifth lumbar vertebra (L5) on posteroanterior (a), lateral (b), 45° right anterior oblique (c), and 45° left anterior oblique (d) radiographs and right parasagittal (e), left parasagittal (f), and axial CT images parallel to the L5 vertebral arch (g). Axial short tau inversion recovery (STIR)-MRI parallel to the L5 vertebral arch (h) and coronal STIR-MRI (i). Note the signal hyperintensity (white arrows) in the pedicle, indicating marrow edema. This is a sign of an early-stage stress fracture of the pars interarticularis.
[Source 25 ]What is spondylolisthesis?
Spondylolisthesis denotes the slippage of one vertebra relative to the one below. Spondylolisthesis is used synonymously with anterolisthesis, which refers to anterior displacement (forward slip) of a vertebral body relative to the one below 26. In spondylolisthesis, the fractured pars interarticularis separates, allowing the injured vertebra to shift or slip forward on the vertebra directly below it. In children and adolescents, this slippage most often occurs during periods of rapid growth — such as an adolescent growth spurt.
Spondylolisthesis most commonly occurs in the lower back (lower lumbar spine) but can also occur in the cervical spine and rarely, except for trauma, in the thoracic spine. Spondylolisthesis most commonly occurs at the L5-S1 level with anterior translation of the L5 vertebral body on the S1 vertebral body 27. The L4-5 level is the second most common location for spondylolisthesis 27.
Doctors commonly describe spondylolisthesis as either low grade or high grade, depending upon the amount of slippage. A high-grade slip occurs when more than 50% of the width of the fractured vertebra slips forward on the vertebra below it. Patients with high-grade slips are more likely to experience significant pain and nerve injury and to need surgery to relieve their symptoms and prevent further deterioration.
Spondylolisthesis is classified according to the Meyerding Classification 28. This is a measure of the percent of antero (forward) or retro (backward) slippage/transitional displacement of one vertebral body on the vertebral body below observed on lateral radiographs.
- Spondylolisthesis grade 1: 0-25% displacement of the vertebral body. Grade 1 spondylolisthesis accounts for 75% of all cases.
- Spondylolisthesis grade 2: 26-50% displacement of the vertebral body.
- Spondylolisthesis grade 3: 51-75% displacement of the vertebral body.
- Spondylolisthesis grade 4: 76-100% displacement of the vertebral body.
- Spondylolisthesis grade 5 (spondyloptosis): >100% displacement of the vertebral body.
Pediatric patients are more likely to increase spondylolisthesis grade when going through puberty. Older patients with lower grade 1 or 2 spondylolisthesis are less likely to progress to higher grades over time.
Other doctors simply describe spondylolisthesis as either low grade or high grade, depending upon the amount of slippage. A high-grade slip occurs when more than 50 percent of the width of the fractured vertebra slips forward on the vertebra below it. Patients with high-grade slips are more likely to experience significant pain and nerve injury and to need surgery to relieve their symptoms.
For most patients with low-grade spondylolisthesis, back pain and other symptoms will improve with nonsurgical treatment.
Spondylolisthesis nonsurgical treatment may include:
- Rest. Avoiding sports and other activities that place excessive stress on the lower back for a period of time can often help improve back pain and other symptoms.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs such as ibuprofen and naproxen can help reduce swelling and relieve back pain.
- Chiropractic care.
- Physical therapy. Specific exercises can help improve flexibility, stretch tight hamstring muscles, and strengthen muscles in the back and abdomen.
- Bracing. Some patients may need to wear a back brace for a period of time to limit movement in the spine and allow a recent pars fracture the opportunity to heal. Although athletes wtih sudden or acute onset of pain are candidates for brace treatment, patients with longer-term pain are not. In these patients, the stress fracture will have a low chance of healing, even after several months in a brace.
Over the course of treatment, your child’s doctor will take periodic X-rays to determine whether the vertebra is changing position.
Surgery may be recommended for spondylolisthesis patients who have:
- Severe or high-grade slippage
- Slippage that is progressively worsening
- Back pain that has not improved after a period of nonsurgical treatment
Spinal fusion between the fifth lumbar vertebra and the sacrum is the surgical procedure most often used to treat patients with spondylolisthesis.
The goals of spinal fusion are to:
- Prevent further progression of the slip
- Stabilize the spine
- Alleviate significant back pain
Figure 9. Spondylolisthesis
What is spondylosis?
Spondylosis also known as osteoarthritis of the spine, is used as a broad descriptive term referring to a common progressive degenerative (wear and tear) disorder of the human spine from any cause; it is usually further qualified by the part of the spine affected, e.g. cervical spondylosis (neck), thoracic spondylosis (middle back) and lumbar spondylosis (lower back). The lumbar region the most affected, because of the exposure to mechanical stress. Spondylosis is usually caused by wear and tear to the facet joints (zygapophysial joints), intervertebral discs, muscles and bones in your spine resulting in pain and stiffness in your neck (cervical spondylosis), middle back (thoracic spondylosis) and lower back (lumbar spondylosis). Like the rest of your body, the intervertebral disks and facet joints in your spine slowly degenerate as you age. Intervertebral discs consist of three major components: an outer fibrous ring called the anulus fibrosus, which surrounds an inner gel-like center, the nucleus pulposus and the cartilaginous endplates that anchor the discs to adjacent vertebrae (Figure 6) 29. The intervertebral disc (intervertebral disk) is the connecting medium between the vertebrae for the transmission of external force in a physiological environment and is important in the normal functioning of the spine. The intervertebral disc is a cushion of fibrocartilage and the principal joint between two vertebrae in the spinal column. There are 23 discs in the human spine: 6 in the cervical region (neck), 12 in the thoracic region (middle back), and 5 in the lumbar region (lower back). From a biomechanical point of view, the intervertebral discs facilitates spinal mobility by allowing your spine to be flexible without sacrificing a great deal of strength 30. They also provide a shock-absorbing effect within the spine and prevent the vertebrae from grinding together. The intervertebral disc is innervated in the outer few millimeters of the annulus fibrosus 31. Only the outer third of the anulus fibrosus is vascular and innervated in a non-pathologic state. In ageing and states of inflammation, both nerve growth and granulation tissue growth are stimulated. Additionally, the granulation tissue secretes inflammatory cytokines, which further increases sensitivity to pain sensations 29. Spondylosis changes can also result in spinal stenosis (narrowing of the spinal canal) and foraminal stenosis (a condition that results when the spinal nerve roots are compressed at the small openings at every level of the spinal column called foramina).
Patients with facet joint pain may present with symptoms of neck pain, back pain, and pain worsened with hyperextension, bending laterally, and rotation 32.
Many people with spondylosis that is seen on X-rays do not present any symptoms. In fact, lumbar spondylosis is present in 27%-37% of people without symptoms.
Approximately 90% of men ages 50 and older — and 90% of women ages 60 and older — have evidence of degenerative changes in the spine.
Some of the risk factors for spondylosis include:
- Repeated strains and sprains
- Occupation – such as jobs that require repetitive motions involving the neck or back
- Previous injuries
- Genetics
- Smoking
Symptoms of spondylosis may include:
- Tingling, numbness and weakness in the arms, hands, legs or feet
- Lack of coordination and difficulty walking
- Sciatica
- Radiculopathy
- Radiculitis
- Pinched nerves
- Localized pain and regional tenderness
- Muscle spasms
- Pain that worsens with prolonged standing, sitting and forward bending
- Numbness and tingling
- Weakness in one or more limbs
- Loss of bladder or bowel control
Seek immediate medical attention if you notice a sudden onset of numbness or weakness, or loss of bladder or bowel control.
As many people with spondylosis do not present symptoms, specific testing may be needed to get a medical diagnosis. If positive, a physician may use more specific terminology regarding your condition such as cervical degenerative disc disease, cervical spinal stenosis, or lumbar spinal stenosis as they describe the pain more effectively.
A doctor will begin with a physical examination to check your range of motion, reflexes, muscle strength and walk to observe if there are changes in your gait.
Imaging studies, such as an x-ray, MRI scan or CT myelography can provide detailed views of your spine. Electromyography (EMG) may also be performed to measure the electrical activity from your nerves to muscles.
The severity of your symptoms and diagnostic imaging results will determine the spondylosis treatment plan that is best for you. Often, conservative treatments will be suggested to relieve pain and help you get back to everyday life.
In severe cases or when non-surgical treatments for spondylosis fail to provide relief, surgical treatment may be recommended.
Non-surgical treatment
In mild to moderate cases of spondylosis, non-surgical treatment options can be effective. These options include:
- Lifestyle changes
- Rest
- Over-the-counter anti-inflammatory drugs
- Physical therapy
- Cortisone shots
- Chiropractic adjustments
- Prescription pain medication
Surgical treatment
Whether you have cervical (neck), lumbar (lower back), or thoracic (mid-back) spondylosis, surgery is NOT commonly recommended for spondylosis unless your doctor determines that:
- A spinal nerve is being pinched by a herniated disk or bone (cervical radiculopathy), or
- Your spinal cord is being compressed (cervical spondylotic myelopathy)
Patients who have progressive neurologic symptoms, such as arm weakness, numbness, unsteadiness while walking, or falling, are more likely to be helped by surgery.
Sometimes, surgery may be recommended if you have severe neck pain (without nerve compression) that has not been relieved by nonsurgical treatment. However, some patients with severe neck pain will not be candidates for surgery. This may be due to the widespread nature of their arthritis, other medical problems, or other causes for their pain, such as fibromyalgia.
Figure 10. Lumbar spondylosis
Spondylolysis causes
Spondylolysis may be congenital or acquired. Although the exact cause remains unknown in all cases, it is most commonly thought of as a fatigue or stress fracture of the pars interarticularis that persists as a non-union 1. It typically develops in genetically susceptible children and adolescents with faulty biomechanics and who also experience repetitive microtrauma on the pars interarticularis from repeated activities involving lumbar hyperextension with rotation 33. The mechanism of injury for spondylolysis is thought to be excessive and repetitive extension movements, particularly when combined with rotation 34. Risk of spondylolytic injury exists for all athletes, but athletes who perform repetitive extension and rotation motions, have an even higher risk 35. Sports such as baseball, throwing events in track and field, cricket, diving, gymnastics, soccer, wrestling, and weightlifting have a higher risk of spondylolysis 34, 36, 37, 38.
Numerous hypotheses have been proposed on the cause of lumbosacral spondylolysis (lumbar spondylolysis), as follows 39:
- Separate ossification centers
- Fracture during postnatal life
- Stress fracture 40
- Increased lumbar lordosis
- Impingement of the articular process on the pars articularis
- Weakness of supporting structures 41
- Growth 15
- Pathologic changes in the pars articularis
- Dysplasia of the pars interarticularis
However, mechanical factors are widely believed to be the cause or at least the trigger of the development of lumbosacral spondylolysis (lumbar spondylolysis), especially when congenital abnormalities are present 42. Moreover, lumbosacral spondylolysis (lumbar spondylolysis) is argued to be related to the human erect posture and lumbar curve 40.
There is a genetic predisposition with an increased incidence seen in:
- Male to female ratio of 2:1
- Alaskan Eskimo descent
- First-degree offspring of those patients with the condition
- Spina bifida occulta, Marfan syndrome, osteogenesis imperfecta, and osteopetrosis
Adolescents involved in sports have a higher prevalence than those not involved in sports. The mean age of diagnosis in athletes is 15 years of age.
There is an increased incidence in those who participate in certain higher-risk sports which involve repeated axial loading and/or lumbar hyperextension with rotation. These sports include gymnastics and dance as the highest prevalence with an increased incidence also seen in football (particularly linemen), rugby, wrestling, martial arts, soccer, basketball, cheerleading, pitching, golf, tennis, volleyball servers, weightlifting, and butterfly and breaststroke swimming 43.
The overall percentage of lumbosacral spondylolysis (lumbar spondylolysis) among athletes in a study by Soler et al 11 was about 8%, a figure not significantly higher than that among the general population. However, certain sporting events were found to contribute higher percentages when each sport was considered separately, with the highest percentages of lumbosacral spondylolysis (lumbar spondylolysis) occurring in throwing sports (26.67%), artistic gymnastics (16.96%), and rowing (16.88%) 11. In an earlier series, a high percentage of lumbosacral spondylolysis (lumbar spondylolysis) was been observed in diving (43.13%), wrestling (29.82%), and weight lifting (22.68%) 13.
Other sports with high incidence rates of lumbosacral spondylolysis (lumbar spondylolysis) are ballet, dancing, football, volleyball, and fast bowlers in cricket. In ballet, the higher incidence rate is due in part to an inability to reach or maintain proper turn-out and thus overcompensation with lordosis.
In general, the presence of the repetitive actions of flexion, extension, rotation, and torsion, either alone or in combination, that are often associated with resistance are the biomechanical movements that show the highest prevalence of lumbosacral spondylolysis (lumbar spondylolysis) 11.
Spondylolysis staging
Spondylolysis can be classified according to the Hollenberg classification that is based on MRI features 16:
- Grade 0: normal pars interarticularis; MRI: no signal abnormality, pars interarticularis intact
- Grade 1: stress reaction; MRI: marrow edema; intact cortical margins
- Grade 2: incomplete stress fracture; MRI: marrow edema; incomplete cortical fracture or fissure
- Grade 3: acute complete stress fracture; MRI: marrow edema; complete cortical fracture extending through pars interarticularis
- Grade 4: chronic stress fracture; MRI: no marrow edema. Fractures completely extending through pars interarticularis
Spondylolysis symptoms
In the majority of cases spondylolysis is asymptomatic and are sometimes found incidently when X-ray is taken for an unrelated injury or condition 18. Approximately 10% of affected individuals manifest symptoms consisting of insidious onset, recurrent, axial, low back pain that increases with activity, is exacerbated by lumbar spinal rotation or extension and may or may not radiate into the buttock or proximal lower limb. Some patients may also report a recent or old history of local trauma. The pain is intense and restricts everyday activities. Symptoms typically worsen acutely after a particular stressful event 44, 45, 19, 46.
When symptoms do occur, the most common symptom is lower back pain. This pain may:
- Feel similar to a muscle strain
- Radiate to the buttocks and back of the thighs
- Worsen with activity and improve with rest
The pain can range from mild to severe and is described as a dull, aching pain in the lower back, buttocks, and posterior thighs. If neurologic symptoms/signs are present, it is likely secondary to spondylolysis with spondylolisthesis and associated disc degeneration resulting in neuroforaminal narrowing and spinal nerve impingement. Since spondylolysis most commonly affects L5 on S1, it would be this dermatomal and myotomal distribution in which manifestations would occur. It is important to note if the patient’s spondylolysis has progressed to spondylolisthesis and they are presenting with pain, the degree of pain does not correlate with the degree of slippage, and this presents a diagnostic challenge and explains why the condition is often advanced prior to diagnosis.
Physical exam would be pertinent for increased lumbar lordosis, tight hamstrings, reduced trunk range of motion particularly with extension, tenderness to palpation overlying the pars fracture site, a positive stork test (single leg hyperextension and rotation of the spine which reproduces the patient pain and is diagnostic of spondylolysis until proven otherwise), and a general absence of signs of a radicular neuropathy. Again, radicular symptoms can occur, but they are not common 47.
In patients with spondylolisthesis, muscle spasms may lead to additional signs and symptoms, including:
- Back stiffness
- Tight hamstrings (the muscles in the back of the thigh)
- Difficulty standing and walking
Spondylolisthesis patients who have severe or high-grade slips may have tingling, numbness, or weakness in one or both legs. These symptoms result from pressure on the spinal nerve root as it exits the spinal canal near the fracture.
Spondylolysis complications
In the majority of patients with spondylolysis, the condition is occult and remains asymptomatic throughout the patients’ lifetimes. However, degenerative disc disease and resultant spondylosis that typically occurs as a normal part of the aging process has a propensity to be accelerated in patients with spondylolysis and may lead to spinal stenosis and lumbar radiculopathy. These deleterious effects may also occur secondary to vertebral slip progression that may occur in patients with spondylolisthesis which as stated previously is present in 50% to 75% of patients with bilateral spondylolysis. Potential surgical complications would include a failed fusion, infection, chronic pain, and neurologic damage 48.
Spondylolysis diagnosis
Your child’s doctor will begin by taking a medical history and asking about your child’s general health and symptoms. They will want to know if your child participates in sports. Children who participate in sports that place excessive stress on the lower back are more likely to have a diagnosis of spondylolysis or spondylolisthesis.
Your child’s doctor will carefully examine your child’s back and spine, looking for:
- Areas of tenderness
- Limited range of motion
- Muscle spasms
- Muscle weakness
The doctor will also observe your child’s posture and gait (the way they walk). In some cases, tight hamstrings may cause a patient to stand awkwardly or walk with a stiff-legged gait.
Based on the literature, the only possible pathognomonic finding during physical examination, is the reproduction of pain by performing the one legged hyperextension manoeuvre (the patient stands on one leg and leans backwards). Interestingly, unilateral lesions often produce pain when standing on the ipsilateral leg (Figure 10) 49, 50, 51.
As a general diagnostic rule, a patient’s neurologic exam, as well as all laboratory evaluation including inflammatory markers, will be largely unremarkable.
There is no universally accepted consensus for an imaging protocol, but the initial imaging studies of choice when the condition is suspected are plain radiographs in the posteroanterior, lateral, and oblique views of the lumbosacral region in the standing position. When present, the lesion is most typically visible in the oblique view which shows the classic “collar on the Scotty dog” and represents the bony defect between the inferior articular surface and the superior articular surface of a single vertebra. As with any stress fracture, plain films may miss the lesion within the first 2 weeks of the injury. Additionally, it is reported plain radiographs only have a sensitivity of 33% in detecting spondylolysis. Due to its superiority of magnetic resonance imaging (MRI) in detecting osseous detail, some authorities advocate for axial computed tomography (CT)-imaging as the test of choice for spondylolysis; however, due to the high prevalence of spondylolysis in the pediatric population and concerns regarding unnecessary radiation, the next advanced imaging modality typically is chosen if plain films are negative is the MRI. MRI is excellent at detecting bone marrow edema associated with acute pars interarticularis stress injury as well as detailing neural and soft tissue pathologies. The single-photon emission computed tomography (SPECT) scan is a suitable alternative to MRI for detecting acute stress fractures, having high sensitivity in detecting spondylolysis when plain films are negative, and is useful in determining the acuity of a fracture but once again carries with it a radiation burden which is preferably avoided in pediatrics 43.
Figure 10. One legged hyperextension manoeuvre
[Source 18 ]Imaging tests
Imaging tests will help confirm the diagnosis of spondylolysis or spondylolisthesis.
- X-rays. X-rays provide images of dense structures, such as bone. The doctor may order X-rays of your child’s lower back from a number of different angles to look for a stress fracture and to view the alignment of the vertebrae.
- If x-rays show a crack or stress fracture in the pars interarticularis portion of the fourth or fifth lumbar vertebra, it is an indication of spondylolysis.
- If the fracture gap at the pars interarticularis has widened and the vertebra has shifted forward, it is an indication of spondylolisthesis. An X-ray taken from the side will help your doctor determine the amount of forward slippage.
- Computed Tomography (CT) Scans. Computed tomography combines X-ray with computer technology to produce more detailed images than plain X-rays. CT scans can help your child’s doctor learn more about the fracture or slippage and can be helpful in planning treatment. Because there is more radiation exposure with CT scans than with regular X-rays, however, your child’s doctor may not routinely order this test. In some cases, a spondylolysis may be discovered in the spine of some teenagers and children when they undergo a CT scan for unrelated reasons, such as abdominal pain or after an accident.
- Single Photo Emission Computed Tomography (SPECT) scans. A SPECT scn uses a small amount of radioactive material to identify areas of increased bone activity. When CT scans are not available, a SPECT scan can identify a spondylolysis. This test is no longer used very often, however.
- Magnetic Resonance Imaging (MRI) Scans. An MRI scan provides better images of the body’s soft tissues than an X-ray. An MRI can help your child’s doctor determine if there is early degeneration of the intervertebral disks between the vertebrae or if a slipped vertebra is pressing on spinal nerve roots. It can also help the doctor determine if there is injury to the pars interarticularis before it can be seen on X-ray.
Spondylolysis treatment
Most patients with spondylolysis, including athletes, can be managed conservatively. In fact, patients who are asymptomatic and their condition is discovered incidentally on imaging may maintain their current level of physical activity without modification including high-level athletic competition. However, if the patient presents with acute symptomatic spondylolysis as confirmed by single-photon emission computed tomography (SPECT)-scan or MRI, conservative treatments are warranted and would include:
- Rest. Avoiding sports and other activities that place excessive stress on the lower back for a period of time can often help improve back pain and other symptoms.
- Bracing. Some patients may need to wear a back brace (Corset versus TLSO) for a period of time (6 to 12 weeks) to limit movement in the spine and allow a recent pars fracture the opportunity to heal. Although athletes wtih sudden or acute onset of pain are candidates for brace treatment, patients with longer-term pain are not. In these patients, the stress fracture will have a low chance of healing, even after several months in a brace. Over the course of treatment, your child’s doctor will take periodic X-rays to determine whether the vertebra is changing position. In some cases, patients resist accepting long-term conservative treatment because they do not want to stop playing sports. Thus, some patients abandon the treatment that could achieve bony union. As a result, the fracture does not heal and it becomes a pseudoarthrosis (pseudoarthrotic spondylolysis) 21. However, a recent meta-analysis found 83% of patients treated non-operatively improve clinically regardless of bracing.
- Activity modification including cessation of athletics activities with a particular emphasis placed on avoidance of pain eliciting maneuvers especially those involving hyperextension of the spine. Athletic activities may be gradually resumed as pain subsides.
- Physical therapy emphasizing spinal stabilization via emphasis on stretching the hip flexors, hamstrings, quadriceps, and gastrocnemius-soleus complex and strengthening the abdominal and back muscles utilizing a pain-free range of motion progressive resistance training protocol such as William’s flexion exercises.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs such as ibuprofen and naproxen can help reduce swelling and relieve back pain.
Adjunctive treatments including ice/heat therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), epidural steroid injections, massage, osteopathic or chiropractic manipulation, and cognitive-behavioral therapy (CBT) are generally well-tolerated, may be of benefit, and should be considered.
With these conservative treatments, 75% of adolescents will have their symptoms improve, and lytic defects heal. Unilateral defects are more likely to heal than bilateral defects. In cases of spondylolysis with concomitant spondylolisthesis, the bony defects are unlikely to heal but the implementation of the same conservative treatment principles typically results in an abatement of the patients’ symptomatology and return to athletic competition. A recent randomized control trial found there to be no difference in treatment outcomes among patients with spondylolisthesis between those subjects treated conservatively and those treated surgically which is important to note considering the cost and potential complications associated with surgical treatments. Additionally, it should be noted there is currently no evidence indicating that spinal bracing will help prevent vertebral slippage in patients’ with spondylolysis with spondylolisthesis.
Orthopedic surgery consultation is warranted if the patient has failed conservative management trial of at least 6 months or has progressive neurologic symptoms, saddle anesthesia, bowel/bladder dysfunction, fever, night pain, rest pain, constant pain, extremes of age, or spondylolysis with spondylolisthesis grade 3 or higher. The most commonly performed surgical treatments of spondylolysis include a direct repair of the pars interarticularis for defects between L1-L4 and an inter-transverse fusion for defects at the L5 level 48.
If surgical correction is necessary the postoperative rehabilitative care should include protection of the surgical site until wound closure (bracing is typically surgeon dependent), proper analgesia, physical therapy, and education on proper biomechanics with an emphasis on posture and sleeping positioning. An integral part of the postoperative rehabilitative care of athletes is a physical therapy graded return to sports protocol consisting of education on proper biomechanics at first and gradually progressing to sport specific activities as tolerated 48.
Surgery
Surgical treatment is used only for symptomatic spondylolysis cases where all conservative methods failed to show any effect 18. Approximately 9-15% of cases of symptomatic spondylolysis undergo surgery 18.
The main indications for surgery include:
- intractable pain,
- progressive slip,
- Low-grade spondylolisthesis (Myerding grade 1 & 2) that fails conservative treatment, is progressive, has neurologic deficits, or likely to progress
- High-grade spondylolisthesis (Myerding grade 3, 4 and 5)
- development of neurological deficits and segmental spine instability.
Surgical procedures typically attempt a direct repair of the pars interarticularis which is sometimes accompanied by a spinal fusion procedure. Specific surgical techniques, such as translaminar screw fixation, cerclage wiring loop and pendiculolaminar hook screws, preserve segmental motion by repairing the isthmic defect 52.
Spinal fusion between the fifth lumbar vertebra and the sacrum is the surgical procedure most often used to treat patients with spondylolisthesis. Spinal fusion is essentially a welding process. The basic idea is to fuse together the affected vertebrae so that they heal into a single, solid bone. Fusion eliminates motion between the damaged vertebrae and takes away some spinal flexibility. The theory is that if the painful spine segment does not move, it should not hurt.
The goals of spinal fusion are to:
- Prevent further progression of the slip
- Stabilize the spine
- Alleviate significant back pain
During the spinal fusion procedure, the doctor will first realign the vertebrae in the lumbar spine. Small pieces of bone — called bone graft — are then placed into the spaces between the vertebrae to be fused. Over time, the bones grow together — similar to how a broken bone heals.
Prior to placing the bone graft, your doctor may use metal screws and rods to further stabilize the spine and improve the chances of successful fusion.
In some cases, patients with high-grade slippage will also have compression of the spinal nerve roots. If this is the case, your doctor may perform a procedure to open up the spinal canal and relieve pressure on the nerves before performing the spinal fusion.
Spondylolysis prognosis
The prognosis in patients with spondylolysis is excellent. The overwhelming majority of cases are asymptomatic, estimated at 80% 53. Asymptomatic individuals require no specific treatments or modifications to activities of daily living or athletic activities. The majority of these asymptomatic cases will not lead to a progressive lesion. Seitsalo et al. 54 found that 23% of their 272 children/adolescents demonstrated slip progression greater than 10% at approximately 16 years follow up. Another study, Danielson et al. 55, found 3% of their 311 patients demonstrated slip progression greater than 20% at approximately four years follow up. Patients are likely most vulnerable to slip progression during growth spurts 56. Beutler et al. 57 studied the natural history of spondylolysis with a 45-year follow-up evaluation. They reported that 19 of 22 patients with bilateral spondylolysis developed spondylolisthesis 57. Their report is the only prospective study to document the long-term prognosis of spondylolysis over 40 years. Although previous studies demonstrated that spondylolysis patients have higher future incidences of disc degeneration and spondylolisthesis when spondylolysis becomes a pseudoarthrosis 4, 58, 59, 5, 60, it is unknown whether the risk for developing severe lumbar degenerative disease requiring surgery increases in these patients.
Even patients’ who present with symptomatic spondylolysis have a very positive prognosis as indicated by a recent meta-analysis which demonstrated adolescent athletes could return to athletic competition 92% of the time when they are treated conservatively and 90% of the time when treated surgically 48.
In the case of symptomatic isthmic pars defect in adolescent patients, roughly 75% to 95% will improve with appropriate conservative management 61, 62.
Estimates are that 9% to 15% of symptomatic pars defects will eventually require surgical intervention 18. Radiographically visualized spondylolysis is associated with spondylolisthesis approximately 25% of the time 63.
References- McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2019 Sep 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333
- Ang, E.C., Robertson, A.F., Malara, F.A. et al. Diagnostic accuracy of 3-T magnetic resonance imaging with 3D T1 VIBE versus computer tomography in pars stress fracture of the lumbar spine. Skeletal Radiol 45, 1533–1540 (2016). https://doi.org/10.1007/s00256-016-2475-7
- Micheli LJ, Wood R. Back pain in young athletes. Significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995 Jan;149(1):15-8. doi: 10.1001/archpedi.1995.02170130017004
- Aoki Y, Takahashi H, Nakajima A, Kubota G, Watanabe A, Nakajima T, Eguchi Y, Orita S, Fukuchi H, Yanagawa N, Nakagawa K, Ohtori S. Prevalence of lumbar spondylolysis and spondylolisthesis in patients with degenerative spinal disease. Sci Rep. 2020 Apr 21;10(1):6739. doi: 10.1038/s41598-020-63784-0
- Sakai T, Sairyo K, Takao S, Nishitani H, Yasui N. Incidence of lumbar spondylolysis in the general population in Japan based on multidetector computed tomography scans from two thousand subjects. Spine (Phila Pa 1976). 2009 Oct 1;34(21):2346-50. doi: 10.1097/BRS.0b013e3181b4abbe
- Lemoine T, Fournier J, Odent T, Sembély-Taveau C, Merenda P, Sirinelli D, Morel B. The prevalence of lumbar spondylolysis in young children: a retrospective analysis using CT. Eur Spine J. 2018 May;27(5):1067-1072. doi: 10.1007/s00586-017-5339-5
- Brooks BK, Southam SL, Mlady GW, Logan J, Rosett M. Lumbar spine spondylolysis in the adult population: using computed tomography to evaluate the possibility of adult onset lumbar spondylosis as a cause of back pain. Skeletal Radiol. 2010 Jul;39(7):669-73. doi: 10.1007/s00256-009-0825-4
- Floman Y. Progression of lumbosacral isthmic spondylolisthesis in adults. Spine (Phila Pa 1976). 2000 Feb 1;25(3):342-7. doi: 10.1097/00007632-200002010-00014
- Roche, M.B. and Rowe, G.G. (1951), The incidence of separate neural arch and coincident bone variations. A survey of 4,200 skeletons. Anat. Rec., 109: 233-252. https://doi.org/10.1002/ar.1091090207
- Liu X, Wang L, Yuan S, Tian Y, Zheng Y, Li J. Multiple-level lumbar spondylolysis and spondylolisthesis. J Neurosurg Spine. 2015 Mar. 22 (3):283-7.
- Soler T, Calderon C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med. 2000 Jan-Feb. 28(1):57-62.
- Congeni J, McCulloch J, Swanson K. Lumbar spondylolysis. A study of natural progression in athletes. Am J Sports Med. 1997 Mar-Apr. 25(2):248-53.
- Rossi F, Dragoni S. Lumbar spondylolysis: occurrence in competitive athletes. Updated achievements in a series of 390 cases. J Sports Med Phys Fitness. 1990 Dec. 30(4):450-2.
- Patel DR, Nelson TL. Sports injuries in adolescents. Med Clin North Am. 2000 Jul. 84(4):983-1007, viii.
- Lonstein JE. Spondylolisthesis in children. Cause, natural history, and management. Spine. 1999 Dec 15. 24(24):2640-8.
- Dunn AJ, Campbell RS, Mayor PE, Rees D. Radiological findings and healing patterns of incomplete stress fractures of the pars interarticularis. Skeletal Radiol. 2008 May;37(5):443-50. doi: 10.1007/s00256-008-0449-0
- Micheli LJ, Wood R. Back pain in young athletes. Significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995 Jan;149(1):15-8. doi:10.1001/archpedi.1995.02170130017004
- Syrmou E, Tsitsopoulos PP, Marinopoulos D, Tsonidis C, Anagnostopoulos I, Tsitsopoulos PD. Spondylolysis: a review and reappraisal. Hippokratia. 2010 Jan;14(1):17-21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2843565
- Standaert CJ, Herring SA. Spondylolysis: a critical review. Br J Sports Med. 2000 Dec;34(6):415-22. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1724260/pdf/v034p00415.pdf
- Mukhopadhyay S, Kamath S, Mukherjee K, Batraa S, Ahuja S. Incidence of pars defects in adolescent idiopathic scoliosis: an MRI study. Acta Orthop Traumatol Turc. 2011;45(4):209-14. doi: 10.3944/AOTT.2011.2555
- Sairyo K, Sakai T, Yasui N, Dezawa A. Conservative treatment for pediatric lumbar spondylolysis to achieve bone healing using a hard brace: what type and how long?: Clinical article. J Neurosurg Spine. 2012 Jun;16(6):610-4. doi: 10.3171/2012.2.SPINE10914
- Fujii K, Katoh S, Sairyo K, Ikata T, Yasui N. Union of defects in the pars interarticularis of the lumbar spine in children and adolescents. The radiological outcome after conservative treatment. J Bone Joint Surg Br. 2004 Mar;86(2):225-31. doi: 10.1302/0301-620x.86b2.14339
- Mushtaq, Raza & Porrino, Jack & Guzmán Pérez-Carrillo, Gloria. (2018). Imaging of Spondylolysis: The Evolving Role of Magnetic Resonance Imaging. PM&R. 10. 10.1016/j.pmrj.2018.02.001
- Collar sign in spondylolysis. https://radiopaedia.org/cases/collar-sign-in-spondylolysis
- Kinshi Kato, Michiyuki Hakozaki, Ryosuke Mashiko, and Shin-ichi Konno. Familial development of lumbar spondylolysis: a familial case report of 7- and 4-year-old brothers and their father. J Int Med Res. 2021 May; 49(5): 03000605211015559. https://doi.org/10.1177/0300060521101555
- Spondylolisthesis. https://radiopaedia.org/articles/spondylolisthesis-1?lang=us
- Tenny S, Gillis CC. Spondylolisthesis. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767
- McClellan JW 3rd, Vernon BA, White MA, Stamm S, Ryschon KL. Should 25-hydroxyvitamin D and bone density using DXA be tested in adolescents with lumbar stress fractures of the pars interarticularis? J Spinal Disord Tech. 2012 Dec;25(8):426-8. doi: 10.1097/BSD.0b013e31823f324f
- Waxenbaum JA, Reddy V, Futterman B. Anatomy, Back, Intervertebral Discs. [Updated 2021 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470583
- Patwardhan A, Havey R, Meade K, Lee B, Dunlap B. A follower load increases the load-carrying capacity of the lumbar spine in compression. Spine 1999;4( 10): 1003-9.
- Roberts S, Evans H, Trivedi J, Menage J. Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am. 2006 Apr;88 Suppl 2:10-4. doi: 10.2106/JBJS.F.00019
- Le DT, Alem N. Facet Joint Injection. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572125
- Yamashita K, Sakai T, Takata Y, Hayashi F, Tezuka F, Morimoto M, Kinoshita Y, Nagamachi A, Chikawa T, Yonezu H, Higashino K, Sakamaki T, Sairyo K. Utility of STIR-MRI in Detecting the Pain Generator in Asymmetric Bilateral Pars Fracture: A Report of 5 Cases. Neurol. Med. Chir. (Tokyo). 2018 Feb 15;58(2):91-95.
- Rossi F Dragoni S. The prevalence of spondylolysis and spondylolisthesis in symptomatic elite athletes: radiographic findings. Radiography. 2001;7(1):37-42.
- Selhorst M, Allen M, McHugh R, MacDonald J. REHABILITATION CONSIDERATIONS FOR SPONDYLOLYSIS IN THE YOUTH ATHLETE. Int J Sports Phys Ther. 2020 Apr;15(2):287-300. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7134351
- Selhorst M, Fischer A, MacDonald J. Prevalence of Spondylolysis in Symptomatic Adolescent Athletes: An Assessment of Sport Risk in Nonelite Athletes. Clin J Sport Med. 2019 Sep;29(5):421-425. doi: 10.1097/JSM.0000000000000546
- Soler T, Calderón C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med. 2000 Jan-Feb;28(1):57-62. doi: 10.1177/03635465000280012101
- Gregory PL, Batt ME, Kerslake RW. Comparing spondylolysis in cricketers and soccer players. Br J Sports Med. 2004 Dec;38(6):737-42. doi: 10.1136/bjsm.2003.008110
- Lumbosacral spondylolysis. https://emedicine.medscape.com/article/95691-overview
- Arriaza BT. Spondylolysis in prehistoric human remains from Guam and its possible etiology. Am J Phys Anthropol. 1997 Nov. 104(3):393-7.
- Aihara T, Takahashi K, Yamagata M, Moriya H, Tamaki T. Biomechanical functions of the iliolumbar ligament in L5 spondylolysis. J Orthop Sci. 2000. 5(3):238-42.
- DeLisa JA, Gans BM, eds. Rehabilitation Medicine: Principles and Practice. 3rd ed. Philadelphia, Pa: Lippincott-Raven; 1998. 1646.
- Mushtaq R, Porrino J, Guzmán Pérez-Carrillo GJ. Imaging of Spondylolysis: The Evolving Role of Magnetic Resonance Imaging. PM R. 2018 Jun;10(6):675-680.
- Standaert CJ. Spondylolysis in the adolescent athlete. Clin J Sport Med. 2002 Mar;12(2):119-22. doi: 10.1097/00042752-200203000-00009
- Ralston S, Weir M. Suspecting lumbar spondylolysis in adolescent low back pain. Clin Pediatr (Phila). 1998 May;37(5):287-93. doi: 10.1177/000992289803700502
- Morita T, Ikata T, Katoh S. Pathogenesis of spondylolysis and spondylolisthesis in young athletes based on a radiological and MRI study. Maui, Hawai: North American Spine Society/Japanese Spine Research Society Spine across the Sea meeting; 1994.
- Roy SL, Shaw PC, Beattie TF. Low back pain in the paediatric athlete. Eur J Emerg Med. 2015 Oct;22(5):348-54.
- Overley SC, McAnany SJ, Andelman S, Kim J, Merrill RK, Cho SK, Qureshi SA, Hecht AC. Return to Play in Adolescent Athletes With Symptomatic Spondylolysis Without Listhesis: A Meta-Analysis. Global Spine J. 2018 Apr;8(2):190-197.
- Logroscino G, Mazza O, Aulisa G, Pitta L, Pola E, Aulisa L. Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Childs Nerv Syst. 2001 Nov;17(11):644-55. doi: 10.1007/s003810100495
- Standaert CJ, Herring SA, Halpern B, King O. Spondylolysis. Phys Med Rehabil Clin N Am. 2000 Nov;11(4):785-803.
- Houglum P. Therapeutic exercise for musculoskeletal injuries. Champaign: Human Kin; 2005.
- Starkey C, Ryan J. Evaluation of Orthopaedic and athletic injuries. Philadelphia: FA Davis Co; 2002.
- Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984 Jun;66(5):699-707
- Seitsalo S, Osterman K, Hyvãrinen H, Tallroth K, Schlenzka D, Poussa M. Progression of spondylolisthesis in children and adolescents. A long-term follow-up of 272 patients. Spine (Phila Pa 1976). 1991 Apr;16(4):417-21. doi: 10.1097/00007632-199104000-00004
- Danielson BI, Frennered AK, Irstam LK. Radiologic progression of isthmic lumbar spondylolisthesis in young patients. Spine (Phila Pa 1976). 1991 Apr;16(4):422-5. doi: 10.1097/00007632-199104000-00005
- Blackburne JS, Velikas EP. Spondylolisthesis in children and adolescents. J Bone Joint Surg Br. 1977 Nov;59-B(4):490-4. doi: 10.1302/0301-620X.59B4.925059
- Beutler WJ, Fredrickson BE, Murtland A, Sweeney CA, Grant WD, Baker D. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine (Phila Pa 1976). 2003 May 15;28(10):1027-35; discussion 1035. doi: 10.1097/01.BRS.0000061992.98108.A0
- Sonne-Holm S, Jacobsen S, Rovsing HC, Monrad H, Gebuhr P. Lumbar spondylolysis: a life long dynamic condition? A cross sectional survey of 4.151 adults. Eur Spine J. 2007 Jun;16(6):821-8. doi: 10.1007/s00586-006-0250-5
- Sakai T, Sairyo K, Suzue N, Kosaka H, Yasui N. Incidence and etiology of lumbar spondylolysis: review of the literature. J Orthop Sci. 2010 May;15(3):281-8. doi: 10.1007/s00776-010-1454-4
- Seitsalo S, Schlenzka D, Poussa M, Osterman K. Disc degeneration in young patients with isthmic spondylolisthesis treated operatively or conservatively: a long-term follow-up. Eur Spine J. 1997;6(6):393-7. doi: 10.1007/BF01834066
- Morita T, Ikata T, Katoh S, Miyake R. Lumbar spondylolysis in children and adolescents. J Bone Joint Surg Br. 1995 Jul;77(4):620-5.
- Kurd MF, Patel D, Norton R, Picetti G, Friel B, Vaccaro AR. Nonoperative treatment of symptomatic spondylolysis. J Spinal Disord Tech. 2007 Dec;20(8):560-4. doi: 10.1097/BSD.0b013e31803dcddd
- Libson E, Bloom RA, Dinari G. Symptomatic and asymptomatic spondylolysis and spondylolisthesis in young adults. Int Orthop. 1982;6(4):259-61. doi: 10.1007/BF00267148