Superficial siderosis
Superficial siderosis of the central nervous system is a rare condition which results from the deposition of hemosiderin on the pial surfaces of the brain or spinal cord from recurrent or prolonged bleeding into the subarachnoid space (the area between the brain and the thin tissues that cover the brain), with eventual neurological dysfunction 1. The most common cause of intracranial superficial siderosis is secondary to subarachnoid hemorrhage. Rarely, superficial siderosis can also be caused by tumors. Superficial siderosis often present in adulthood with hearing loss and gait instability (ataxia) that progressively worsen. Superficial siderosis diagnosis is primarily made by magnetic resonance imaging (MRI); however, susceptibility-weighted imaging (SWI) and T2* gradient echo (GRE) sequences demonstrate the highest sensitivity in detecting this condition. On imaging, superficial siderosis is classically characterized on MRI as a rim of low signal coating the surface of the brain or spinal cord, particularly noted with the gradient echo or susceptibility-weighted sequences.
The literature is divided as to whether the term superficial siderosis should be confined to cases where there is no history of symptomatic subarachnoid hemorrhage or whether it is a blanket term referring to the superficial deposition of hemosiderin, irrespective of cause.
As there are many causes of recurrent or extensive subarachnoid hemorrhage, the demographics are ill-defined and represent those of the underlying cause. Cases have been reported in patients between 14 and 77 years of age 2. Overall, there is a male predilection (M:F 3:1) 3.
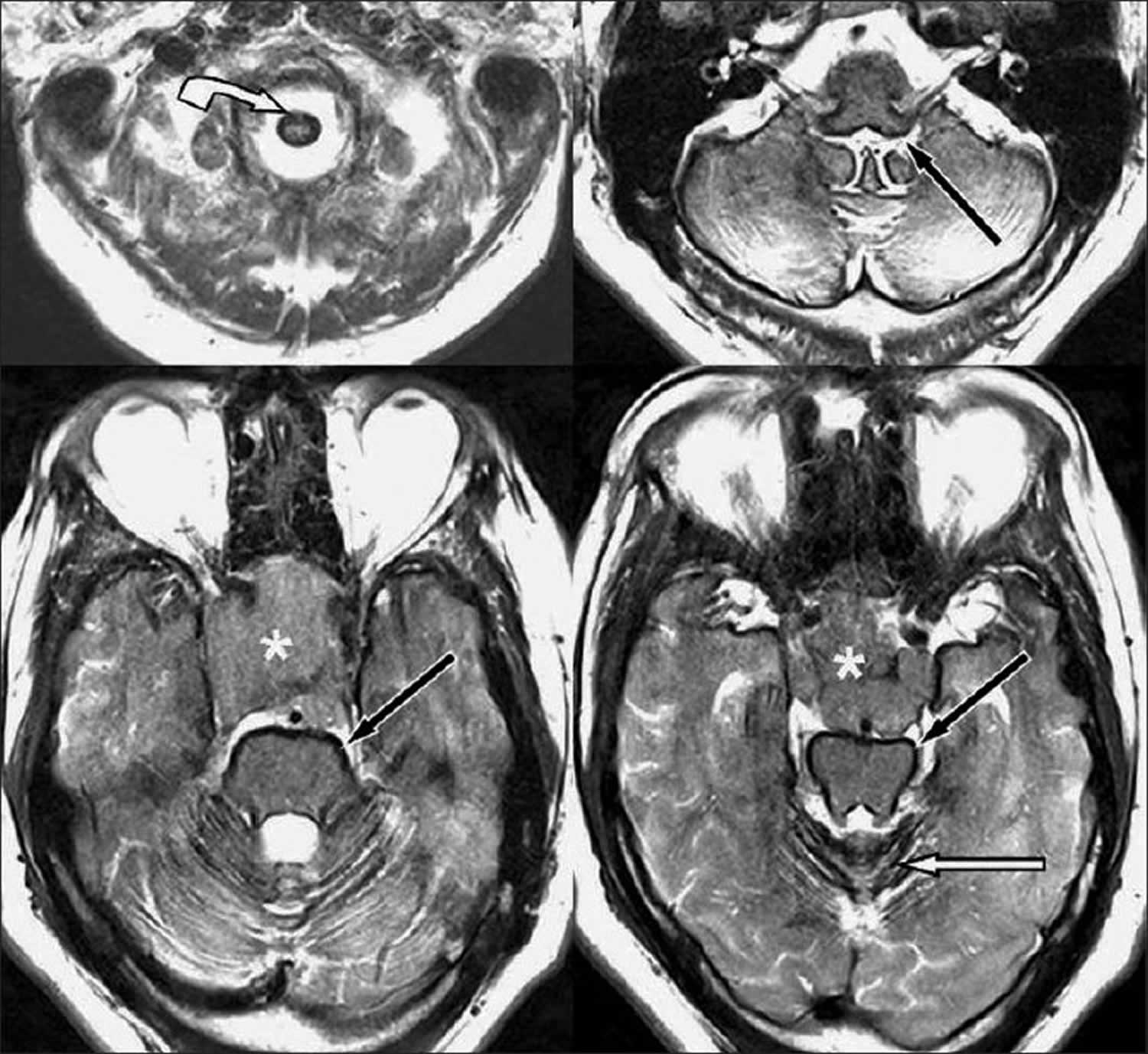
Figure 1. Superficial siderosis MRI
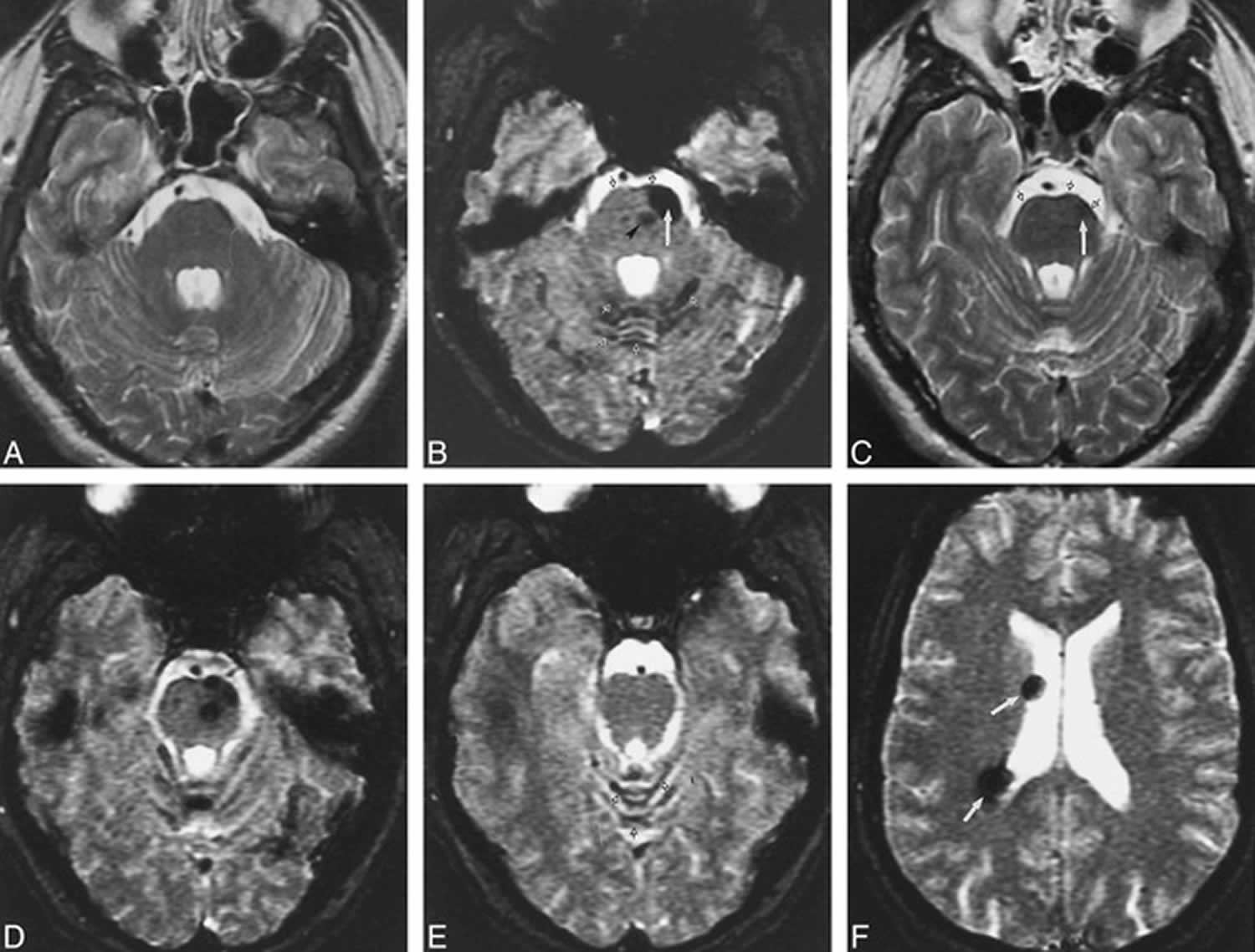
Footnote: Images of a 32-year-old male patient with superficial siderosis of the central nervous system associated with multiple cavernous malformations.
(A) Axial spin-echo 3500/98/1 (TR/TE/excitations) T2-weighted magnetic resonance imaging (MRI), centered at the level of the pons, suggests mild hypointensity along the ventral surface of the pons, particularly on the left.
(B) Axial gradient-echo 750/40/2 susceptibility MRI with a flip angle of 10°, obtained at the same level as that shown in A, shows focal regions of hypointensity in the ventral left pons (solid arrow) as well as the central pons (arrowhead), consistent with cavernous malformations. In addition, hypointensity along the ventral surface of the pons is better appreciated, as is hypointensity along the folia of the vermis of the cerebellum (open arrows).
(C) Axial spin-echo 3500/98/1 T2-weighted MR image, obtained at the level of the upper pons, raises the possibility of mild hypointensity along the surface of the brain stem (open arrows), as well as a small focal region of hypointensity within the left upper pons (solid arrow).
(D) Axial gradient-echo 750/40/2 susceptibility MR image with a flip angle of 10°, acquired at the identical level as that shown in C, shows “blooming” of the hypointensity within the left side of the brain stem, consistent with cavernous malformations that are superficial, as well as markedly improved visualization of hypointensity consistent with siderosis along the cerebellar folia and surface of the brain stem, as compared with the T2-weighted image shown in C.
(E) Axial gradient-echo 750/40/2 susceptibility MR image with a flip angle of 10°, obtained at a more cephalad level, shows hypointensity consistent with siderosis along the folia of the superior vermis (open arrows).
(F) Axial gradient-echo 750/40/2 susceptibility MR image with a flip angle of 10°, obtained at the level of the lateral ventricles, shows cavernous malformations along the ependymal/subependymal region (solid arrows) but no hemosiderin staining of the ependyma.
[Source 3 ]Superficial siderosis causes
There are many underlying causes of superficial siderosis which include, but are not limited to, idiopathic (unknown, no source of bleeding evident), trauma, arteriovenous malformations (AVMs), subarachnoid hemorrhage (SAH), amyloid angiopathy, brachial plexus or root injury, and brain tumors including intraventricular pilocytic astrocytoma 1. Pilocytic astrocytoma is a low-grade tumor that is most prevalent in the first two decades of life with an incidence rate of 4.8/1 million/year 4.
A cause of recurrent subarachnoid hemorrhage is present in ~50% of superficial siderosis cases 5:
- Spinal dural defects
- traumatic cervical nerve root avulsion
- dural defect with spinal CSF collections/spinal cyst 6
- post-operative pseudomeningocoele
- Intracranial neoplasms
- occult small ependymoma
- oligodendroglioma
- astrocytoma
- Vascular abnormalities
- arteriovenous malformation (AVM)
- micro-arteriovenous malformation
- aneurysm
- fragile capillary regrowth after brain surgery 3
- arteriovenous malformation (AVM)
- Cerebral amyloid angiopathy: seen in 60% of patients 7
- Idiopathic: up to 46% of cases 3
Superficial siderosis is thought to result from recurrent occult subarachnoid bleeds although the source of bleeding is not usually identified on imaging 8. Although it is common to see a small amount of hemosiderin deposition at the margins of a previous hemorrhage or surgical resection margin, a single episode of subarachnoid hemorrhage is usually not sufficient to result in this condition 3.
Animal models of superficial siderosis have shown that recurrent subarachnoid hemorrhage resulting in the prolonged contact of these tissues with iron is crucial to the development of the disorder 9. Within the cerebellum, microglia as well as Bergmann glia are uniquely sensitive to iron-mediated cell damage. The terminal processes of Bergmann glia that interface with the subarachnoid space mediate iron uptake from the CSF, inducing the synthesis of ferritin within these cells. Because ferritin sequesters iron and is thus thought to play a role in iron detoxification, intracellular iron may not cause toxicity until ferritin biosynthesis is overwhelmed by a large iron load. Excess free iron may then stimulate lipid peroxidation, leading to localized tissue necrosis 9.
The preferential involvement of vestibulocochlear nerve (CN 8) is partly because of its extensive lining with central myelin, which is supported by siderosis-susceptible microglia 10. In addition, its course through the pontine cistern exposes the nerve to an abundance of iron. Cranial nerve 1 also is affected similarly for the same reasons; therefore, it is speculated that anosmia is underreported in association with siderosis because this symptom often is not sought or documented clinically. It is not clear why symptoms of optic nerve involvement also are not found as often as hearing loss, but it is speculated that cranial nerve 2 (optic nerver) comes into contact with significant CSF volumes over only a short distance in its course 11.
Superficial siderosis symptoms
Superficial siderosis is characterized by the classic triad of sensorineural deafness (95%), cerebellar ataxia (88%), and pyramidal signs (76%) 1. Other symptoms that present less frequently include dementia (24%), bladder disturbance (24%), anosmia (17%), anisocoria (10%), and sensory signs (13%) 12.
The classic clinical presentation of superficial siderosis includes adult-onset slowly progressive gait (less commonly appendicular) ataxia with cerebellar dysarthria and sensorineural hearing impairment 13.
Symptoms can vary depending on the distribution of hemosiderin deposition. Typical symptoms include 3:
- sensorineural hearing loss
- most common, found in ~95% of patients
- bilateral and gradual
- cerebellar dysfunction (ataxia): ~90%
- pyramidal signs: ~75%
- other less common findings include
- dementia
- bladder incontinence
- other cranial nerve dysfunction
- sensory deficits
Superficial siderosis diagnosis
Superficial siderosis of the central nervous system should be highly suspected in patients with progressive sensorineural hearing loss, ataxia, and signs of pyramidal tracts. Commonly performed investigations during the work-up of superficial siderosis include MR imaging (MRI) of the brain and whole spinal cord, CT myelography, MR angiography (MRA), and cerebrospinal angiography. A prior history of trauma (at times trivial) or intradural surgery (commonly involving the posterior fossa) may be present 14. Often decades elapse between the presumed inciting event and the development of symptoms attributable to superficial siderosis.
Advanced MRI techniques such as susceptibility-weighted imaging (SWI) and enhanced susceptibility-weighted angiography (ESWAN) is the investigation of choice for the diagnosis of superficial siderosis of the central nervous system 15. However, the bleeding source may be not be detected despite extensive neuroimaging 16. It is also important to realize that the degree of imaging abnormality does not always correlate with the degree of clinical impairment 17. Some patients with diffuse findings revealed by imaging have minimal symptoms, whereas others with less severe findings may be debilitated significantly.
Cerebrospinal fluid examination commonly shows the presence of red blood cells or xanthochromia 18. Other reported CSF findings in superficial siderosis include the presence of erythrophages, siderophages, and elevated iron and ferritin levels 19. Because of the intermittent nature of the bleeding, these findings may be absent.
Superficial siderosis treatment
Unfortunately, no proven direct treatment exists for established superficial siderosis of the brain, and workup is focused on identifying the causative lesion, although often even this is not possible. There is no cure for superficial siderosis and treatment is still a matter of ongoing research. Iron chelating agents have been tried with limited anecdotal success 10. Treatment of superficial siderosis is primarily aimed at addressing the underlying cause of the bleed and preventing further progression of the disease 20. Management of superficial siderosis is aimed at eliminating the cause of recurrent subarachnoid hemorrhage either by surgical or endovascular treatment. Surgical treatment of superficial siderosis depends on early identification of the bleeding source. Surgical excision of the offending lesion (neoplasm or vascular malformation or pseudomeningoceles) and repair of dural defects are logical therapeutic strategies 16.
Iron chelators and antioxidants have been used to treat idiopathic superficial siderosis of the brain; however, there is little evidence to support their effectiveness 21.
One drug which has shown promising results is deferiprone. Deferiprone is a lipid-soluble iron chelator that is Food and Drug Administration (FDA) approved for thalassemia. In a case report published by Levy et al. 22, one patient showed complete resolution of his ataxia and hearing loss after 3 years of treatment with deferiprone.
When no correctable cause is identified, signs and symptoms are slowly progressive.
Superficial siderosis prognosis
If left untreated, superficial siderosis can lead to progressive worsening of hearing loss and gait instability with as many as 25% of patients being bedridden within a few years 1.
References- Jetty SN, Badar Z, Drumsla D, Mangla R. Clinical Significance of T2*gradient-recalled Echo/susceptibility-weighted Imaging Sequences in Evaluating Superficial Siderosis in the Setting of Intracerebral Tumors: Pilocytic Astrocytoma. J Clin Imaging Sci. 2018;8:36. Published 2018 Aug 24. doi:10.4103/jcis.JCIS_60_17 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6118113
- Bradley WG, Brant-Zawadzki M, Cambray-Forker J. MRI of the brain. Surendra Kumar. (2001) ISBN:0781725682
- Hsu WC, Loevner LA, Forman MS, Thaler ER. Superficial siderosis of the CNS associated with multiple cavernous malformations. AJNR Am J Neuroradiol. 1999;20(7):1245-1248. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7055971
- Burkhard C, Di Patre PL, Schüler D, Schüler G, Yaşargil MG, Yonekawa Y, et al. A population-based study of the incidence and survival rates in patients with pilocytic astrocytoma. J Neurosurg. 2003;98:1170–4.
- Kumar N. Neuroimaging in superficial siderosis: an in-depth look. AJNR Am J Neuroradiol. 2010 Jan;31(1):5-14. doi: 10.3174/ajnr.A1628. Epub 2009 Sep 3. https://doi.org/10.3174/ajnr.A1628
- Webb AJ, Flossmann E, Armstrong RJ. Superficial siderosis following spontaneous intracranial hypotension. Pract Neurol. 2015 Oct;15(5):382-4. http://dx.doi.org/10.1136/practneurol-2015-001169
- Linn J, Halpin A, Demaerel P, et al. Prevalence of superficial siderosis in patients with cerebral amyloid angiopathy. Neurology. 2010;74(17):1346-1350. doi:10.1212/WNL.0b013e3181dad605 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2875936
- Kumar N. Neuroimaging in superficial siderosis: an in-depth look. AJNR Am J Neuroradiol. 2010 Jan;31(1):5-14. https://doi.org/10.3174/ajnr.A1628
- Koeppen AH, Dickson AC, Chu RC, Thach RE. The pathogenesis of superficial siderosis of the central nervous system. . Ann Neurol 1993;34:646-653
- Rowland LP, Pedley TA. Merritt’s Neurology. Lippincott Williams & Wilkins. (2009) ISBN:0781791863
- Fearnley JM, Stevens JM, Rudge P. Superficial siderosis of the central nervous system. . Brain 1995;118:1051-1066
- Fearnley JM, Stevens JM, Rudge P. Superficial siderosis of the central nervous system. Brain. 1995;118(Pt 4):1051–66.
- Kumar N. Superficial siderosis: associations and therapeutic implications. Arch Neurol 2007; 64: 491–96
- Kumar N, Cohen-Gadol AA, Wright RA, et al. Superficial siderosis. Neurology 2006; 66: 1144–52
- Chen H, Raza HK, Jing J, Ye X, Zhang Z, Hua F, Cui G. Superficial siderosis of central nervous system with unknown cause: report of 2 cases and review of the literature. Br J Neurosurg. 2019 Jun;33(3):305-308. doi: 10.1080/02688697.2017.1406452. Epub 2017 Nov 21. https://doi.org/10.1080/02688697.2017.1406452
- Neuroimaging in Superficial Siderosis: An In-Depth Look. N. Kumar. American Journal of Neuroradiology Jan 2010, 31 (1) 5-14. https://doi.org/10.3174/ajnr.A1628
- Swartz JD. Pathology of the vestibulocochlear nerve. Neuroimaging Clin N Am. 2008 May;18(2):321-46, x-xi. https://doi.org/10.1016/j.nic.2008.02.001
- Kumar N. Superficial Siderosis: Associations and Therapeutic Implications. Arch Neurol. 2007;64(4):491–496. doi:10.1001/archneur.64.4.491 https://jamanetwork.com/journals/jamaneurology/fullarticle/793672
- Fearnley JM, Stevens JM, Rudge P. Superficial siderosis of the central nervous system. Brain. 1995 Aug;118 ( Pt 4):1051-66. doi: 10.1093/brain/118.4.1051
- Calvo M, de Miguel C, Pinel A, Ortega J, Aladro Y. Diffuse superficial siderosis of the central nervous system: Four case reports and review of the literature. Rev Neurol. 2014;59:354–8.
- Bracchi M, Savoiardo M, Triulzi F, et al. Superficial siderosis of the CNS. MR diagnosis and clinical findings. AJNR Am J Neuroradiol 1993;14:227-236
- Levy, M., Turtzo, C. & Llinas, R. Superficial siderosis: a case report and review of the literature. Nat Rev Neurol 3, 54–58 (2007). https://doi.org/10.1038/ncpneuro0356