What is synovial chondromatosis
Synovial chondromatosis also called synovial osteochondromatosis, is a rare, benign (noncancerous) condition that involves the synovium, which is the thin layer of tissue that lines the joints. Synovial chondromatosis can arise in any joint in your body, but the knee is most common joint affected. However, synovial chondromatosis can affect any synovial joint such as the hip, the elbow, the shoulder, the temporal mandibular joint (TMJ), and the ankle may also be affected. Synovial chondromatosis most often occurs in the knee, followed by the hip, elbow, and shoulder. In most cases, only one joint in the body is affected.
Synovial chondromatosis most often occurs in patients between the ages of 30 and 50, it is rarely present before the age of 20, and it is very rare in children. Men are reported to be affected with synovial chondromatosis up to four times more commonly than women.
In synovial chondromatosis, the synovium grows abnormally and produces nodules made of cartilage. These nodules can sometimes break off from the synovium and become loose inside the joint. The size of the loose cartilage bodies inside the joint can vary—from a few millimeters (the size of a small pill) to a few centimeters (the size of a marble).
The synovial fluid nourishes the loose bodies and they may grow, calcify (harden), or ossify (turn into bone). When this occurs, they can roll around freely inside the joint space. As they roll around, the loose bodies can damage the smooth articular cartilage that covers the joint, causing osteoarthritis. In osteoarthritis, damaged cartilage becomes worn and frayed. Moving the bones along this exposed joint surface is painful.
In severe cases of synovial chondromatosis, the loose bodies may grow large enough to occupy the entire joint space or penetrate into adjacent tissues.
It is important to seek treatment for synovial chondromatosis as early as possible to help relieve painful symptoms and prevent the progression of osteoarthritis in the joint.
Although synovial chondromatosis is not cancerous, it can severely damage the affected joint and, eventually, lead to osteoarthritis. Early treatment is important to help relieve painful symptoms and prevent further damage to the joint.
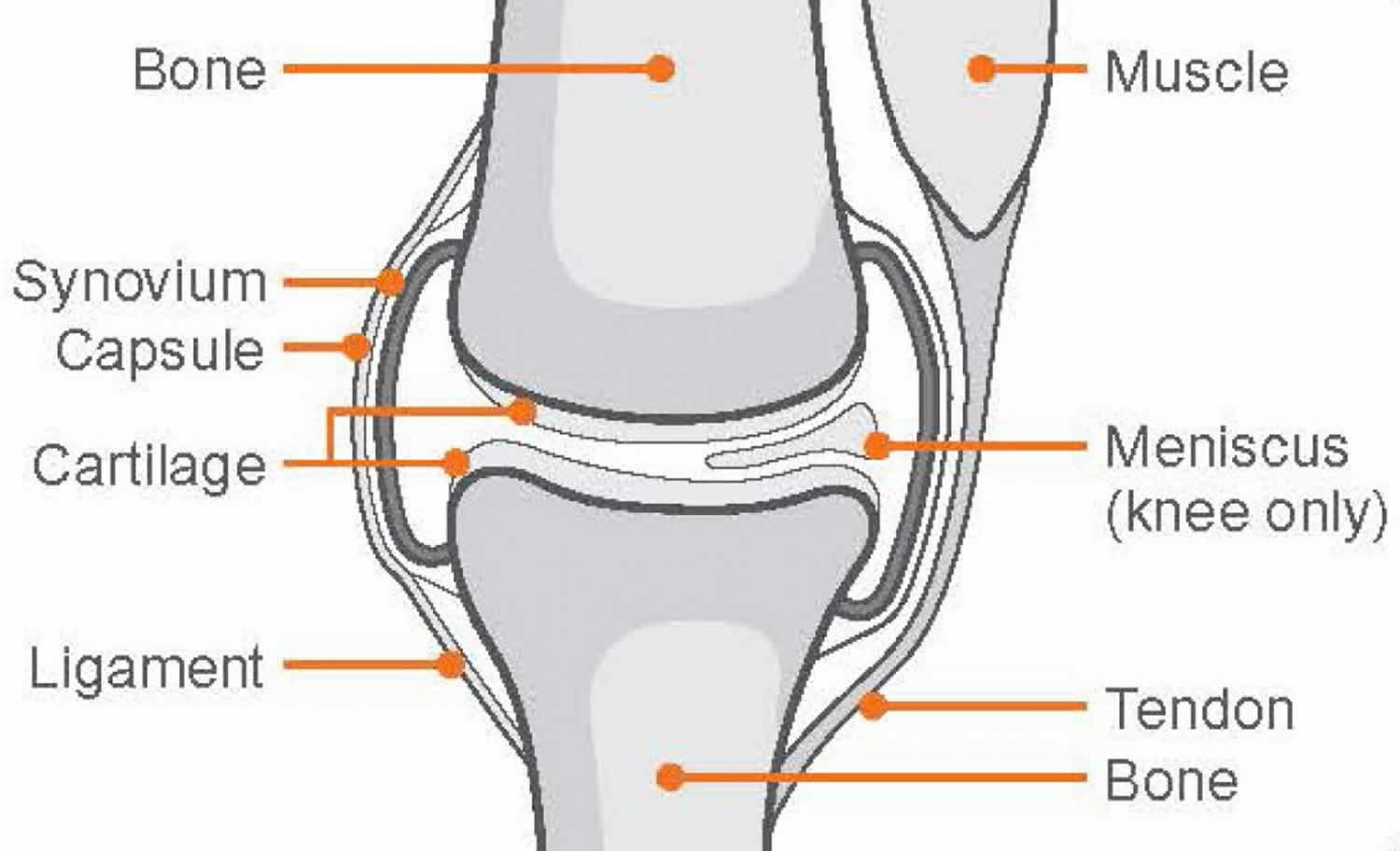
Joint anatomy
A joint is where the ends of two or more bones meet—such as your knee joint, shoulder joint, or ankle joint.
Healthy joints are covered with articular cartilage—a slippery substance that helps the bones glide smoothly over each other during movement.
Thick bands of tissue surround the joint, forming a capsule that holds it together. The undersurface of the joint capsule is lined by a thin membrane called the synovium. The synovium produces a fluid that lubricates the joint.
Synovial chondromatosis causes
The cause of synovial chondromatosis is unknown. Synovial chondromatosis occurs spontaneously. Synovial chondromatosis is not inherited. Reference to both primary form (no evidence of concurrent joint pathology) and secondary form (occurring in the setting of joint degeneration) is made in the literature. The secondary form occurs more common and usually, in older individuals.
Primary synovial chondromatosis also known as Reichel syndrome or Reichel-Jones-Henderson syndrome, is a benign monoarticular disorder of unknown origin that is characterized by synovial metaplasia and proliferation resulting in multiple intra-articular cartilaginous loose bodies of relatively similar size, not all of which are ossified. Hence, the term synovial chondromatosis is preferred over primary synovial osteochondromatosis. It is distinct from secondary synovial chondromatosis that is the result of a degenerative change in the joint.
Secondary synovial chondromatosis is a disorder that results in intra-articular loose bodies as a result of trauma, osteoarthrosis, or neuropathic arthropathy. It is quite distinct to primary synovial chondromatosis. Pathologically concentric rings of growth may be seen.
Elevated levels of bone morphogenic protein in the loose body lesions and the affected synovial joints of patients with primary synovial chondromatosis have been documented 1. However, the etiological importance of this has not been determined. Similarly, elevated levels of interleukin-6 and vascular endothelial growth factor-A have been found in these joints, but the importance of these findings is not certain. Secondary synovial chondromatosis is felt to occur ar a result of mechanical changes in a joint due to arthropathy. The formation of loose chondral bodies is thought to be part of the degenerative process in these joints.
Synovial chondromatosis pathophysiology
X-ray examination reveals irregularly shaped loose bodies within a synovial joint. This number varies anywhere from two or three loose bodies to several dozens. They present in varied sizes and several loose bodies may combine to form larger bodies. The number of intraarticular lesions is greater in the primary type than the secondary type. The gross and microscopic evaluation of the loose bodies reveals lobulated masses of hyaline cartilage surrounded by a layer of synovial tissue. The hyaline cartilage is hypercellular, and the cells are often atypical. These atypical changes are multinucleated cells, myxoid degeneration of matrix, crowding of cell nuclei and large nuclei. In long-standing disease, the lobules can undergo peripheral ossification. High levels of bone morphogenic protein have been found in the loose cartilaginous bodies and synovial tissue. The loose bodies may create pathological mechanical wear on joint surfaces and result in various types of erosion of articular surfaces. The process is classified as a benign neoplastic rather than a metaplastic lesion.
Synovial chondromatosis symptoms
Patients typically present with joint pain as a chief complaint. This usually is coupled with complaints of joint swelling. It most frequently is monoarticular in the primary form and may be multi-articular in the secondary form. Occasionally the patient will experience locking or catching in the joint. Pain is increased with weight bearing and may also be present at rest. In the secondary form, a history of osteoarthritis, post-traumatic arthritis, or rheumatoid arthritis may be present. Joint effusion may increase with increased activity. With increased joint effusions, pain can also increase.
The most common symptoms of synovial chondromatosis are similar to those of osteoarthritis. These include:
- Joint pain
- Joint swelling
- Limited range of motion in the affected joint
Other signs and symptoms of synovial chondromatosis may include:
- Fluid in the joint
- Tenderness
- A creaking, grinding, or popping noise during movement (crepitus)
The nodules can sometimes be felt in joints that are close to the skin, such as the knee, ankle, and elbow joints.
Synovial chondromatosis diagnosis
Your doctor will talk with you about your general health and medical history and ask about your symptoms. He or she will then carefully examine the affected joint, looking for:
- Swelling
- Tenderness
- Limited range of motion
- Creaking or grinding noises during movement, an indication of bone-on-bone friction
Synovial chondromatosis radiology
Your doctor will order imaging studies to help diagnose synovial chondromatosis. Imaging studies will also help your doctor differentiate synovial chondromatosis from osteoarthritis.
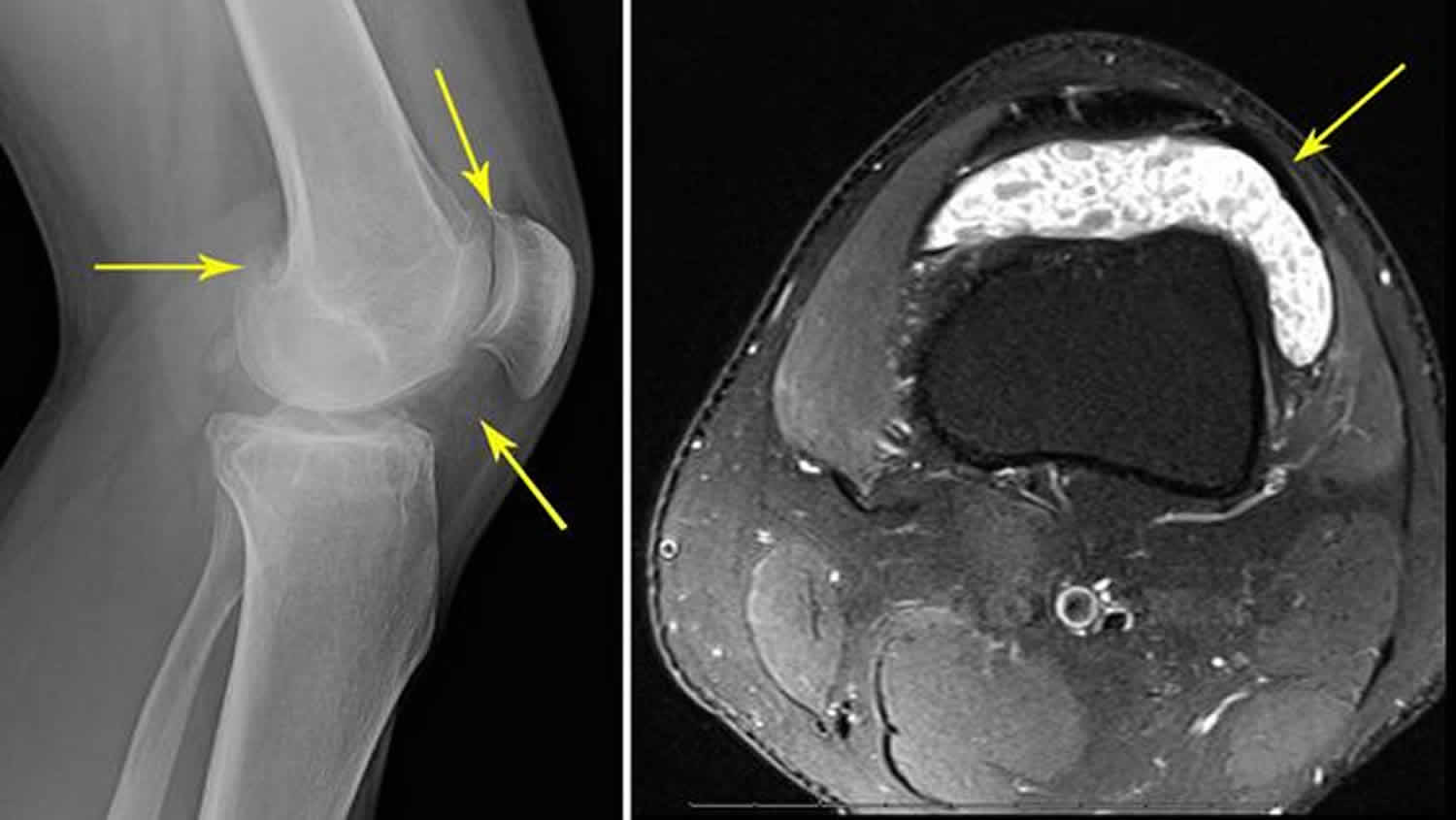
- X-rays. X-rays provide images of dense structures, such as bone. Larger loose bodies are usually calcified or ossified and can be seen on x-ray. Smaller loose bodies and those that are not calcified or ossified may not show up.
- Other imaging studies. If the loose bodies are not visible on x-ray, your doctor may order a magnetic resonance imaging (MRI) scan or computerized tomography (CT) scan to better evaluate the joint. Loose bodies can typically be seen on both MRI and CT scans.
In addition to showing the loose bodies, imaging tests can also help your doctor determine whether you have any additional problems, such as fluid in the joint or signs of osteoarthritis (narrowing of the joint space and bone spurs).
Figure 1. Synovial chondromatosis knee
Footnote: (Left) In this x-ray of a knee joint, the small loose bodies are barely visible (arrows). (Right) This MRI scan shows a cross-section image of the same knee. The loose bodies show up clearly (arrow).
Figure 2. Synovial chondromatosis elbow
Footnote: (Left) X-ray of an elbow joint shows two large ossified loose bodies (arrows). (Right) MRI scan shows a cross-section image of the same elbow.
Figure 3. Synovial chondromatosis hip (right hip synovial chondromatosis)
Footnote: Apple core appearance as can be seen in right hip synovial chondromatosis.
Figure 4. Synovial chondromatosis shoulder (multiple intra-articular loose bodies are seen in the left shoulder)
Figure 5. Synovial chondromatosis TMJ (primary synovial chondromatosis of the tempormandibular joint)
Footnote: Large left temporomandibular joint (TMJ) effusion with multiple small foci of low signal predominantly within the posterior joint recess suggestive of cartiliginous bodies. The disc is abnormal with loss of biconcavity, thinning of the anterior band and abnormal signal intensity. The disc overlies the mandibular condyle, with normal anterior translation of the disc and mandibular condyle to the articular eminence on mouth opening. Mandibular condyle maintains a rounded contour. Findings are suggestive of left TMJ synovial chondromatosis.
Synovial chondromatosis treatment
Management of primary synovial chondromatosis is surgery. Current arthroscopic surgical techniques allow for arthroscopic surgical management, however, occasionally open procedures may be necessary. Removal of loose bodies with partial synovectomy of the involved joints results in decreased pain, improved mechanical function, and decreased swelling in most cases. Open procedures have similar results, but surgical morbidity is greater. Post-operative management includes a progressive range of motion and strengthening of peri-articular muscle groups. The use of post-operative non-steroidal anti-inflammatory medication is not confirmed as being beneficial. Rare re-occurrence is reported following surgical management with partial synovectomy.
Secondary synovial chondromatosis is managed by anti-inflammatory medication with the additional management of the inflammatory joint symptoms until or unless mechanical symptoms prohibit adequate function. At this point, surgical management is indicated. Surgical management should address improving long-term function and prognoses. As such, joint reconstruction or arthroplasty in addition to removal of loose bodies is indicated.
Nonsurgical treatment
Observation. Depending on your symptoms, simple observation can sometimes be a treatment option. Your doctor will carefully consider a number of factors in determining whether observation is appropriate in your case.
During this time, your doctor will closely monitor the affected joint to check for the progression of osteoarthritis.
Surgical treatment
Treatment for synovial chondromatosis typically involves surgery to remove the loose bodies of cartilage. In some cases, the synovium is also partially or fully removed (synovectomy) during surgery.
Surgery can be done using either an open procedure or an arthroscopic procedure. The technique your doctor uses will depend upon a number of factors, including:
- The number of loose bodies
- The size of the loose bodies
- The condition of the synovium
In a traditional open procedure, the doctor will usually make one or two large incisions.
In an arthroscopic procedure, the doctor will make smaller incisions and use miniature surgical tools to remove the loose bodies.
The end results of both open and arthroscopic procedures are the same. Your doctor will talk with you about which surgical technique is best in your case.
Recovery from surgery
How long it takes to return to your daily activities will vary, depending on the type of procedure you have. Your doctor will provide you with specific instructions to guide your rehabilitation.
Synovial chondromatosis may return in up to 20 percent of patients. For a period of time after surgery, your doctor will schedule regular follow-up visits to check for any recurrence.
Your doctor will also monitor the joint for any progression of osteoarthritis. The amount of damage synovial chondromatosis has already done to the joint will influence your chance of developing osteoarthritis.
Synovial chondromatosis prognosis
There is rarely reoccurrence of primary synovial chondromatosis after surgical management with the removal of the loose bodies and partial synovectomy. Reoccurrence has been reported in a case involving the temporal mandibular joint.
References