TIA
TIA is short for transient ischemic attack is sometimes called a mini-stroke. TIA has similar symptoms to an ischemic stroke , such as speech and visual disturbance, and numbness or weakness in the face, arms and legs, but these only last a few minutes to a few hours and fully resolve within 24 hours and do not cause any permanent damage. A TIA is a warning that you may have a stroke – so if you think you have had a TIA, it is very important to take steps to prevent a stroke. If you suspect you are having a TIA, call your local emergency number for an ambulance, even if your symptoms disappear and you start to feel better.
Although the symptoms of a TIA resolve in a few minutes or hours, you’ll need treatment to help prevent another TIA or a full stroke happening in the future.
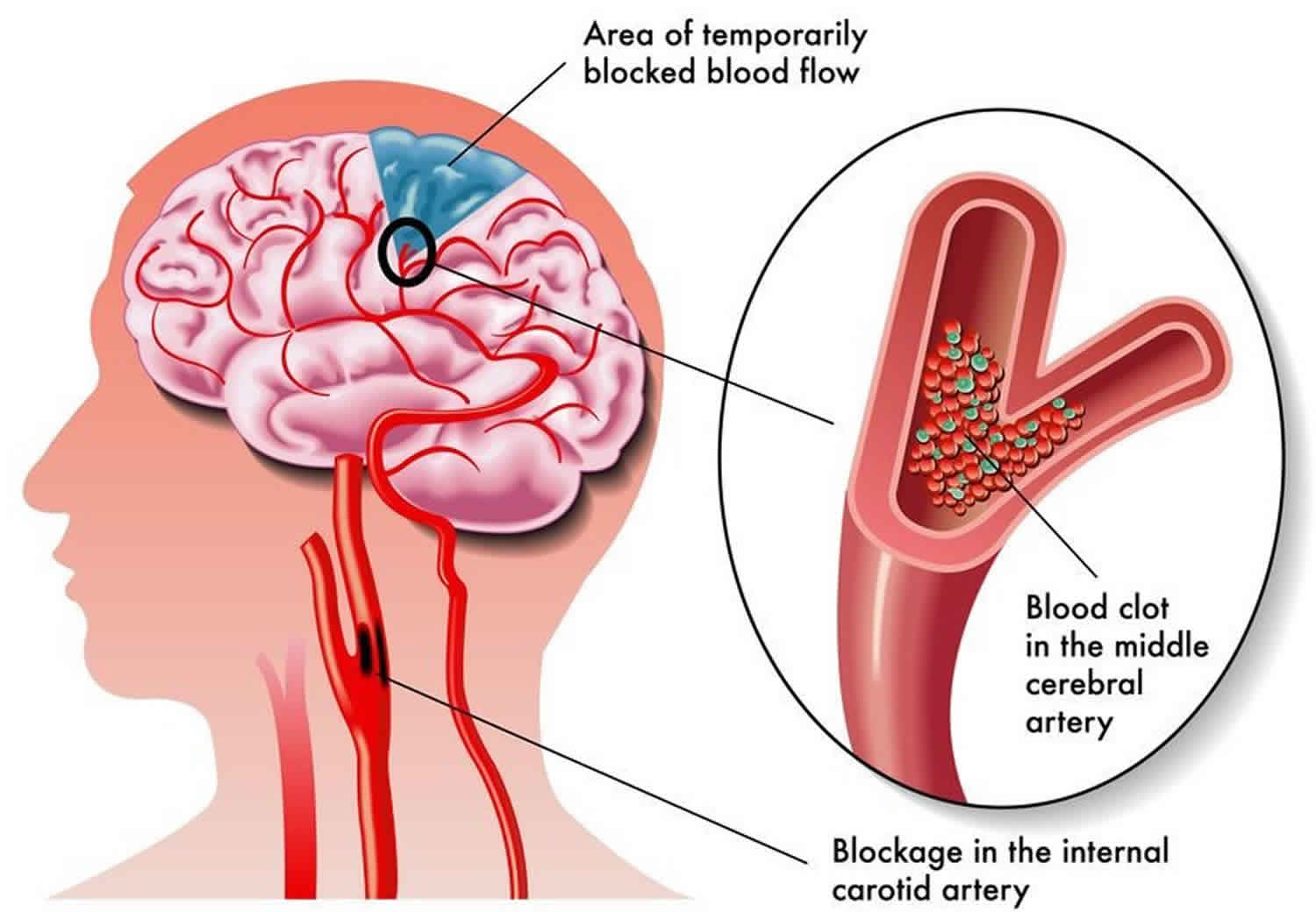
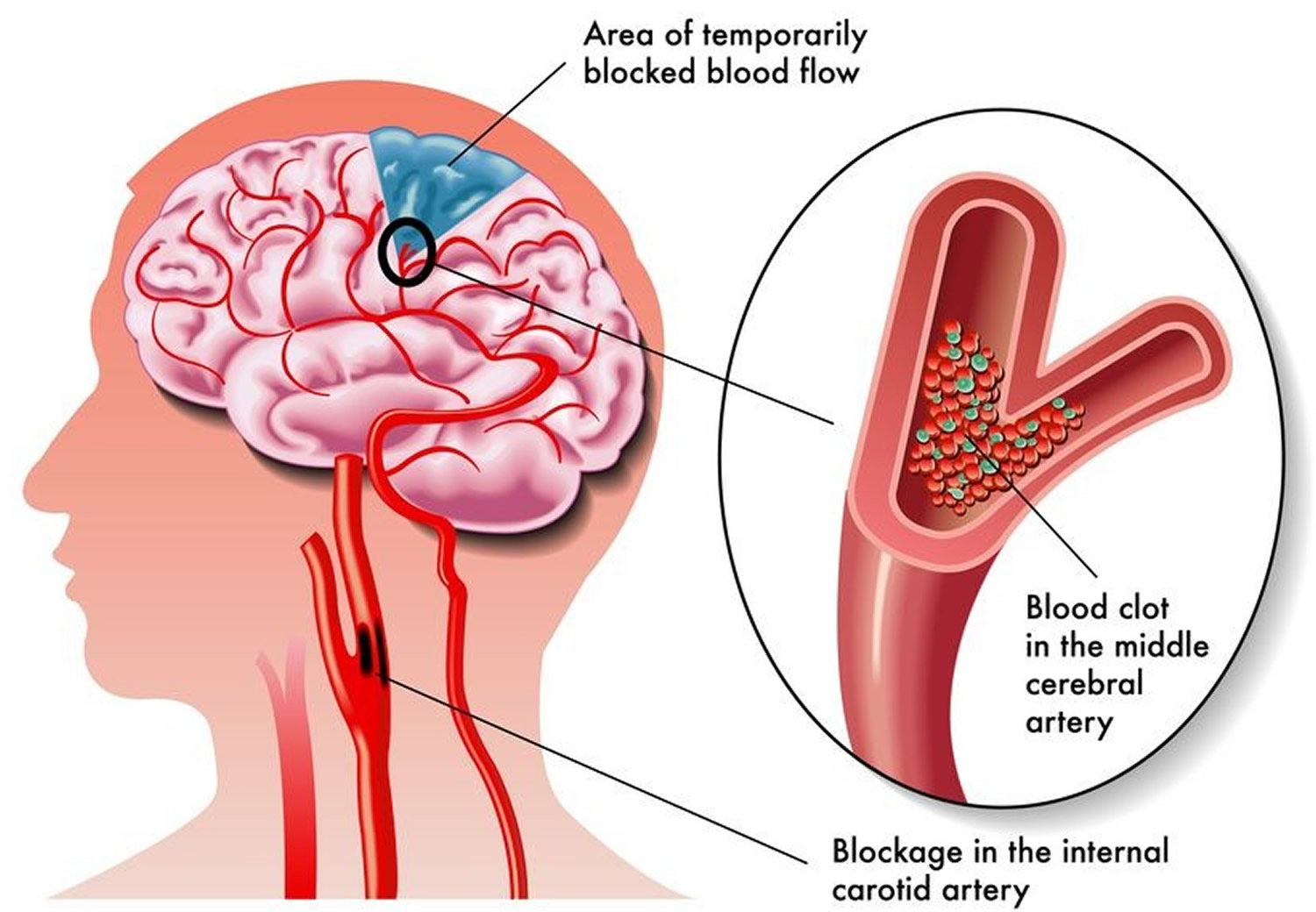
A TIA happens when the blood supply to your brain is temporarily blocked. This may happen because there is a build-up of fatty deposits in your blood vessels known as atherosclerosis leading to a reduced flow of blood to the brain, or because there is a blood clot.
When blood flow to the brain is blocked, the brain is starved of oxygen and nutrients. This causes cells to start dying and you experience symptoms. In a TIA, the blockage clears, the oxygen and nutrients return to the brain, and the symptoms go away.
If you have a stroke, the cells die and the brain is permanently damaged.
About 1 in 3 people who have a TIA will go on to have a stroke, sometimes within the next few hours. The biggest risk is in the first year after the TIA. If you receive treatment, your risk of stroke after a TIA can be greatly reduced.
You must not drive for 2 weeks after experiencing a TIA.
To diagnose whether you have had a TIA, your doctor will ask about your symptoms and will order a series of tests including a brain scan. If it is a TIA, the brain scan will not show any signs of recent brain injury.
You may also need a series of other tests to diagnose why you had the TIA and your risk factors for a stroke. These may include imaging of your arteries with ultrasound, CT or MRI, a blood pressure check, heart tests and blood tests to assess your risks.
Once your doctor has determined the cause of your transient ischemic attack, the goal of treatment is to correct the abnormality and prevent a stroke. Depending on the cause of your TIA, your doctor may prescribe medication to lower your blood pressure, lower your blood cholesterol, thin your blood to prevent clots, or control atrial fibrillation (a type of irregular heart rhythm) or may recommend surgery or a balloon procedure (angioplasty). You may need to take medicine for the rest of your life.
Having a TIA is an opportunity to take action to reduce your risk of having a stroke.
- Eat a healthy diet with plenty of fruit and vegetables, whole grains, lean meats, poultry and fish, and reduced-fat dairy.
- Limit your intake of salt, sugar and saturated fats.
- Do at least 30 minutes of regular physical activity every day.
- Don’t smoke.
- Make sure your weight is healthy.
- If you have diabetes, make sure it is under control.
- Drink alcohol in moderation.
Figure 1. Transient ischemic attack (TIA) or mini stroke
In the early stages of a TIA, it’s not possible to tell whether you’re having a TIA or a full stroke.
It’s important to call your local emergency services number immediately and ask for an ambulance if you or someone else has symptoms of a TIA or stroke.
If a TIA is suspected, you should be offered aspirin to take straight away. This helps to prevent a stroke.
Even if your symptoms disappear while you’re waiting for an ambulance to arrive, you still need to be assessed in hospital.
You should be referred to see a specialist within 24 hours of the onset of your symptoms.
A TIA is a warning sign that you may be at risk of having a full stroke in the near future, and an assessment can help doctors determine the best way to reduce the chances of that happening.
If you think you may have had a TIA previously, but the symptoms have passed and you did not seek medical advice at the time, make an urgent appointment with a doctor.
They can determine whether to refer you for a hospital assessment, if appropriate.
What is a stroke
A stroke is a serious life-threatening medical condition that occurs when the blood supply to part of the brain is cut off. Within minutes, brain cells begin to die. If brain cells die or are damaged because of a stroke, symptoms occur in the parts of the body that these brain cells control. Examples of stroke symptoms include sudden weakness; paralysis or numbness of the face, arms, or legs (paralysis is an inability to move); trouble speaking or understanding speech; and trouble seeing.
- Strokes are a medical emergency and urgent treatment is essential.
- A stroke can cause lasting brain damage, long-term disability, or even death.
- Stroke is the no. 3 cause of death in the United States. More than 140,000 people die each year from stroke in the United States.
- Stroke is the leading cause of serious, long-term disability in the United States.
- Each year, approximately 795,000 people suffer a stroke. About 600,000 of these are first attacks, and 185,000 are recurrent attacks.
- Nearly three-quarters of all strokes occur in people over the age of 65. The risk of having a stroke more than doubles each decade after the age of 55.
- Strokes can and do occur at ANY age. Nearly one fourth of strokes occur in people under the age of 65.
- Stroke death rates are higher for African-Americans than for whites, even at younger ages.
- On average, someone in the United States has a stroke every 40 seconds.
- Stroke accounted for about one of every 17 deaths in the United States in 2006. Stroke mortality for 2005 was 137,000.
- The risk of ischemic stroke in current smokers is about double that of nonsmokers after adjustment for other risk factors.
- Atrial fibrillation (AF) is an independent risk factor for stroke, increasing risk about five-fold.
- High blood pressure is the most important risk factor for stroke.
The sooner a person receives treatment for a stroke, the less damage is likely to happen.
If you suspect that you or someone else is having a stroke, call your local emergency number immediately and ask for an ambulance.
The main symptoms of stroke can be remembered with the word F.A.S.T.:
- Face – the face may have dropped on one side, the person may not be able to smile, or their mouth or eye may have dropped.
- Arms – the person with suspected stroke may not be able to lift both arms and keep them there because of weakness or numbness in one arm.
- Speech – their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake.
- Time – it’s time to dial your local emergency number immediately if you see any of these signs or symptoms.
If you have any of these symptoms or if you suspect someone else is having a stroke, you must get to a hospital quickly to begin treatment. Acute stroke therapies try to stop a stroke while it is happening by quickly dissolving the blood clot or by stopping the bleeding.
Post-stroke rehabilitation helps individuals overcome disabilities that result from stroke damage. Drug therapy with blood thinners is the most common treatment for stroke.
TIA causes
A transient ischemic attack has the same origins as that of an ischemic stroke, the most common type of stroke. In an ischemic stroke, a clot blocks the blood supply to part of your brain. In a transient ischemic attack, unlike a stroke, the blockage is brief, and there is no permanent damage.
The underlying cause of a TIA often is a buildup of cholesterol-containing fatty deposits called plaques (atherosclerosis) in an artery or one of its branches that supplies oxygen and nutrients to your brain.
Plaques can decrease the blood flow through an artery or lead to the development of a clot. A blood clot moving to an artery that supplies your brain from another part of your body, most commonly from your heart, also may cause a TIA.
Certain things can increase your chances of having a TIA, including:
- smoking
- high blood pressure (hypertension)
- obesity
- high cholesterol levels
- regularly drinking an excessive amount of alcohol
- having a type of irregular heartbeat called atrial fibrillation
- having diabetes
People over 55 years of age and people of Asian, African or Caribbean descent are also at a higher risk of having a TIA.
Risk factors for TIA
Some risk factors for a transient ischemic attack and stroke can’t be changed. Others you can control.
Risk factors you can’t change
You can’t change the following risk factors for a transient ischemic attack and stroke. But knowing you’re at risk can motivate you to change your lifestyle to reduce other risks.
- Family history. Your risk may be greater if one of your family members has had a TIA or a stroke.
- Age. Your risk increases as you get older, especially after age 55.
- Sex. Men have a slightly higher risk of a TIA and a stroke. But as women age, their risk of a stroke goes up.
- Prior transient ischemic attack. If you’ve had one or more TIAs, you’re much more likely to have a stroke.
- Sickle cell disease. Stroke is a frequent complication of sickle cell disease. Another name for this inherited disorder is sickle cell anemia. Sickle-shaped blood cells carry less oxygen and also tend to get stuck in artery walls, hampering blood flow to the brain. However, with proper treatment of sickle cell disease, you can lower your risk of a stroke.
Risk factors you can control
You can control or treat a number of factors — including certain health conditions and lifestyle choices — that increase your risk of a stroke. Having one or more of these risk factors doesn’t mean you’ll have a stroke, but your risk increases if you have two or more of them.
Health conditions
- High blood pressure. The risk of a stroke begins to increase at blood pressure readings higher than 140/90 millimeters of mercury (mm Hg). Your doctor will help you decide on a target blood pressure based on your age, whether you have diabetes and other factors.
- High cholesterol. Eating less cholesterol and fat, especially saturated fat and trans fat, may reduce the plaques in your arteries. If you can’t control your cholesterol through dietary changes alone, your doctor may prescribe a statin or another type of cholesterol-lowering medication.
- Cardiovascular disease. This includes heart failure, a heart defect, a heart infection or an abnormal heart rhythm.
- Carotid artery disease. The blood vessels in your neck that lead to your brain become clogged.
- Peripheral artery disease. The blood vessels that carry blood to your arms and legs become clogged.
- Diabetes. Diabetes increases the severity of atherosclerosis — narrowing of the arteries due to accumulation of fatty deposits — and the speed with which it develops.
- High levels of homocysteine. Elevated levels of this amino acid in your blood can cause your arteries to thicken and scar, which makes them more susceptible to clots.
- Excess weight. Obesity, especially carrying extra weight in the abdominal area, increases stroke risk in both men and women.
Lifestyle choices
- Cigarette smoking. Quit smoking to reduce your risk of a TIA and a stroke. Smoking increases your risk of blood clots, raises your blood pressure and contributes to the development of cholesterol-containing fatty deposits in your arteries (atherosclerosis).
- Physical inactivity. Engaging in 30 minutes of moderate-intensity exercise most days helps reduce risk.
- Poor nutrition. Reducing your intake of fat and salt decreases your risk of a TIA and a stroke.
- Heavy drinking. If you drink alcohol, limit yourself to no more than two drinks daily if you’re a man and one drink daily if you’re a woman.
- Use of illicit drugs. Avoid cocaine and other illicit drugs.
TIA prevention
Knowing your risk factors and living healthfully are the best things you can do to prevent a TIA. Included in a healthy lifestyle are regular medical checkups. Also:
- Don’t smoke. Stopping smoking reduces your risk of a TIA or a stroke.
- Limit cholesterol and fat. Cutting back on cholesterol and fat, especially saturated fat and trans fat, in your diet may reduce buildup of plaques in your arteries.
- Eat plenty of fruits and vegetables. These foods contain nutrients such as potassium, folate and antioxidants, which may protect against a TIA or a stroke.
- Limit sodium. If you have high blood pressure, avoiding salty foods and not adding salt to food may reduce your blood pressure. Avoiding salt may not prevent hypertension, but excess sodium may increase blood pressure in people who are sensitive to sodium.
- Exercise regularly. If you have high blood pressure, regular exercise is one of the few ways you can lower your blood pressure without drugs.
- Limit alcohol intake. Drink alcohol in moderation, if at all. The recommended limit is no more than one drink daily for women and two a day for men.
- Maintain a healthy weight. Being overweight contributes to other risk factors, such as high blood pressure, cardiovascular disease and diabetes. Losing weight with diet and exercise may lower your blood pressure and improve your cholesterol levels.
- Don’t use illicit drugs. Drugs such as cocaine are associated with an increased risk of a TIA or a stroke.
- Control diabetes. You can manage diabetes and high blood pressure with diet, exercise, weight control and, when necessary, medication.
TIA signs and symptoms
Transient ischemic attack symptoms are similar to those of a stroke. But, unlike a stroke, most of the symptoms will disappear within an hour if it is a TIA.
The main symptoms of a TIA can be remembered with the word “FAST”:
- Face – the face may have dropped on one side, the person may not be able to smile, or their mouth or eye may have dropped.
- Arms – the person with suspected stroke may not be able to lift both arms and keep them there because of weakness or numbness in one arm.
- Speech – their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake.
- Time – it’s time to dial your local emergency number immediately if you see any of these signs or symptoms.
The symptoms in the FAST test identify most strokes and TIAs, but a TIA can occasionally cause different symptoms that typically appear suddenly (usually over a few seconds).
TIA signs and symptoms may also include:
- a severe, sudden headache
- temporary blindness or blurred vision
- vision disturbances (double vision or not being able to see to the left or right)
- speech disturbance (not being able to say what you’re thinking, or using the wrong words)
- slurred speech
- facial numbness or weakness
- difficulty swallowing (dysphagia)
- weakness or paralysis of the face, arm or leg
- complete paralysis of one side of the body
- vertigo (spinning sensation)
- being sick
- dizziness
- loss of balance and co-ordination
- nausea and vomiting
- confusion
- difficulty understanding what others are saying
However, there may be other causes for these symptoms.
Stroke signs and symptoms
The main symptoms of stroke can be remembered with the word F.A.S.T.:
- Face – the face may have dropped on one side, the person may not be able to smile, or their mouth or eye may have dropped.
- Arms – the person with suspected stroke may not be able to lift both arms and keep them there because of weakness or numbness in one arm.
- Speech – their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake.
- Time – it’s time to dial your local emergency number immediately if you see any of these signs or symptoms.
If you have any of these symptoms or if you suspect someone else is having a stroke, you must get to a hospital quickly to begin treatment. Acute stroke therapies try to stop a stroke while it is happening by quickly dissolving the blood clot or by stopping the bleeding.
Post-stroke rehabilitation helps individuals overcome disabilities that result from stroke damage. Drug therapy with blood thinners is the most common treatment for stroke.
TIA diagnosis
A prompt evaluation of your symptoms is vital in diagnosing the cause of your TIA and deciding on a method of treatment. To help determine the cause of your TIA and to assess your risk of a stroke, your doctor may rely on the following:
- Physical exam and tests. Your doctor will perform a physical exam and a neurological exam. The doctor will test your vision, eye movements, speech and language, strength, reflexes, and sensory system. Your doctor may use a stethoscope to listen to the carotid artery in your neck. A whooshing sound (bruit) may indicate atherosclerosis. Or your doctor may use an ophthalmoscope to look for cholesterol fragments or platelet fragments (emboli) in the tiny blood vessels of the retina at the back of your eye. Your doctor may check for risk factors of a stroke, including high blood pressure, high cholesterol levels, diabetes and in some cases high levels of the amino acid homocysteine.
- Carotid ultrasonography. If your doctor suspects that the carotid artery may be the cause of your TIA, a carotid ultrasound may be considered. A wand-like device (transducer) sends high-frequency sound waves into your neck. After the sound waves pass through your tissue and back, your doctor can analyze images on a screen to look for narrowing or clotting in the carotid arteries.
- Computerized tomography (CT) or computerized tomography angiography (CTA) scanning. CT scanning of your head uses X-ray beams to assemble a composite 3D look at your brain or evaluate the arteries in your neck and brain. CTA scanning uses X-rays similar to a standard CT scan but may also involve injection of a contrast material into a blood vessel. Unlike a carotid ultrasound, a computerized tomography angiography scan can evaluate blood vessels in the neck and head.
- Magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA). These procedures, which use a strong magnetic field, can generate a composite 3D view of your brain. Magnetic resonance angiography uses technology similar to MRI to evaluate the arteries in your neck and brain but may include an injection of a contrast material into a blood vessel.
- Echocardiography. Your doctor may choose to perform a traditional echocardiography called transthoracic echocardiogram (TTE). A TTE involves moving an instrument called a transducer across your chest. The transducer emits sound waves that bounce off different parts of your heart, creating an ultrasound image. Or your doctor may choose to perform another type of echocardiography called a transesophageal echocardiogram (TEE). During a transthoracic echocardiogram, a flexible probe with a transducer built into it is placed in your esophagus — the tube that connects the back of your mouth to your stomach. Because your esophagus is directly behind your heart, clearer, detailed ultrasound images can be created. This allows a better view of some things, such as blood clots, that might not be seen clearly in a traditional echocardiography exam.
- Arteriography. This procedure gives a view of arteries in your brain not normally seen in X-ray imaging. A radiologist inserts a thin, flexible tube (catheter) through a small incision, usually in your groin. The catheter is manipulated through your major arteries and into your carotid or vertebral artery. Then the radiologist injects a dye through the catheter to provide X-ray images of the arteries in your brain. This procedure may be used in selected cases.
TIA treatment
Once your doctor has determined the cause of your transient ischemic attack, the goal of treatment is to correct the abnormality and prevent a stroke. Depending on the cause of your TIA, your doctor may prescribe medication to reduce the tendency for blood to clot or may recommend surgery or a balloon procedure (angioplasty).
Medications
Doctors use several medications to decrease the likelihood of a stroke after a transient ischemic attack. The medication selected depends on the location, cause, severity and type of TIA. Your doctor may prescribe:
- Anti-platelet drugs. These medications make your platelets, one of the circulating blood cell types, less likely to stick together. When blood vessels are injured, sticky platelets begin to form clots, a process completed by clotting proteins in blood plasma. The most frequently used anti-platelet medication is aspirin. Aspirin is also the least expensive treatment with the fewest potential side effects. An alternative to aspirin is the anti-platelet drug clopidogrel (Plavix). Your doctor might prescribe aspirin and clopidogrel to be taken together for about a month after the TIA. Research shows that taking these two drugs together in certain situations reduces the risk of a future stroke more than taking aspirin alone. There may be certain situations when the duration of taking both medications together may be extended, such as when the cause of the TIA is a narrowing of a blood vessel located in the head. Your doctor may consider prescribing Aggrenox, a combination of low-dose aspirin and the anti-platelet drug dipyridamole, to reduce blood clotting. The way dipyridamole works is slightly different from aspirin.
- Anticoagulants. These drugs include heparin and warfarin (Coumadin, Jantoven). They affect clotting-system proteins instead of platelet function. Heparin is used for a short time and is rarely used in the management of TIAs. These drugs require careful monitoring. If atrial fibrillation is present, your doctor may prescribe a direct oral anticoagulant such as apixaban (Eliquis), rivaroxaban (Xarelto), edoxaban (Savaysa) or dabigatran (Pradaxa).
Blood pressure medicines
If you have high blood pressure, you’ll be offered a type of medicine called an antihypertensive to control it. This is because high blood pressure increases your risk of having a TIA or stroke.
There are lots of different types of medicine that can help control blood pressure, including:
- thiazide diuretics
- angiotensin-converting enzyme (ACE) inhibitors
- calcium channel blockers
- beta-blockers
Your doctor will advise you about which antihypertensive is the most suitable for you. Some people may be offered a combination of 2 or more different medicines.
Statins
If you have high cholesterol, you’ll be advised to take a medicine known as a statin. Statins reduce the level of cholesterol in your blood by blocking an enzyme in the liver that produces cholesterol.
Statins may also help to reduce your risk of a stroke whatever your cholesterol level is. You may be offered a statin even if your cholesterol level is not particularly high.
Examples of statins often given to people who have had a TIA include atorvastatin, simvastatin and rosuvastatin.
Surgery
If you have a moderately or severely narrowed neck (carotid) artery, your doctor may suggest carotid endarterectomy. This preventive surgery clears carotid arteries of fatty deposits (atherosclerotic plaques) before another TIA or stroke can occur. An incision is made to open the artery, the plaques are removed, and the artery is closed.
Angioplasty
In selected cases, a procedure called carotid angioplasty, or stenting, is an option. This procedure involves using a balloon-like device to open a clogged artery and placing a small wire tube (stent) into the artery to keep it open.
Driving after a TIA
Although a TIA should not have a long-term impact on your daily activities, you must stop driving immediately.
If your doctor is happy that you have made a good recovery and there are no lasting effects after 1 month, you can start driving again.
You do not need to inform the Driver and Vehicle Licensing Agency (DVLA), but you should contact your car insurance company.
Lifestyle changes
There are several lifestyle changes you can make that may help to reduce your chances of having a stroke after a TIA.
These include:
- eating a healthy, balanced diet – a low-fat, reduced-salt, high-fibre diet is usually recommended, including plenty of fresh fruit and vegetables
- exercising regularly – for most people this means at least 150 minutes of moderate-intensity activity, such as cycling or fast walking, or 75 minutes of vigorous-intensity activity such as running, swimming, or riding a bike up a hill, every week. Plus, strength exercises on 2 days every week
- stopping smoking – if you smoke, stopping may significantly reduce your risk of having a stroke in the future
- cutting down on alcohol – men and women are advised to limit alcohol intake.