Tinea manuum
Tinea manuum is a ringworm fungus (tinea) or dermatophyte infection affecting the palm and interdigital spaces, which typically presents as a diffuse white scaling or hyperkeratosis (keratoderma), with or without mild itching 1. Even though unilateral or asymmetrical involvement and concomitant infection of other sites (especially fingernails and feet) may be useful in assisting in the diagnosis of Tinea manuum, its distinction from similar inflammatory dermatoses is often challenging, with consequent diagnostic delays, errors and unnecessary therapies 2. Tinea manuum is much less common than tinea pedis (athlete’s foot or tinea affecting the foot). Tinea pedis (rare in prepubertal children; erythema, scale, fissures, maceration; itching between toes extending to sole, borders, and occasionally dorsum of foot; may be accompanied by tinea manuum 3. Mild tinea manuum is treated with topical antifungal agents, but if the treatment is unsuccessful, oral antifungal medicines may be considered, including terbinafine and itraconazole.
Tinea manuum is frequently misdiagnosed because it appears similar to 4:
- Hand dermatitis – especially the type called pompholyx.
- Psoriasis – especially palmoplantar pustulosis.
- Keratolysis exfoliativa.
The main differential diagnoses of Tinea manuum includes palmar psoriasis and chronic hand eczema 2.
Tinea manuum can be clinically distinguished from hand dermatitis 4:
- In most cases of tinea manuum, only a single hand is involved.
- If both hands are affected, involvement is asymmetrical.
- Increased skin markings can be seen in dermatitis, but in chronic tinea manuum, they are white because of surface scale.
- Involvement of both palm and back of the hand in contiguity.
- The rash may have an elevated border.
- Nearby nails may also be infected (tinea unguium). However, other skin conditions can also affect nails.
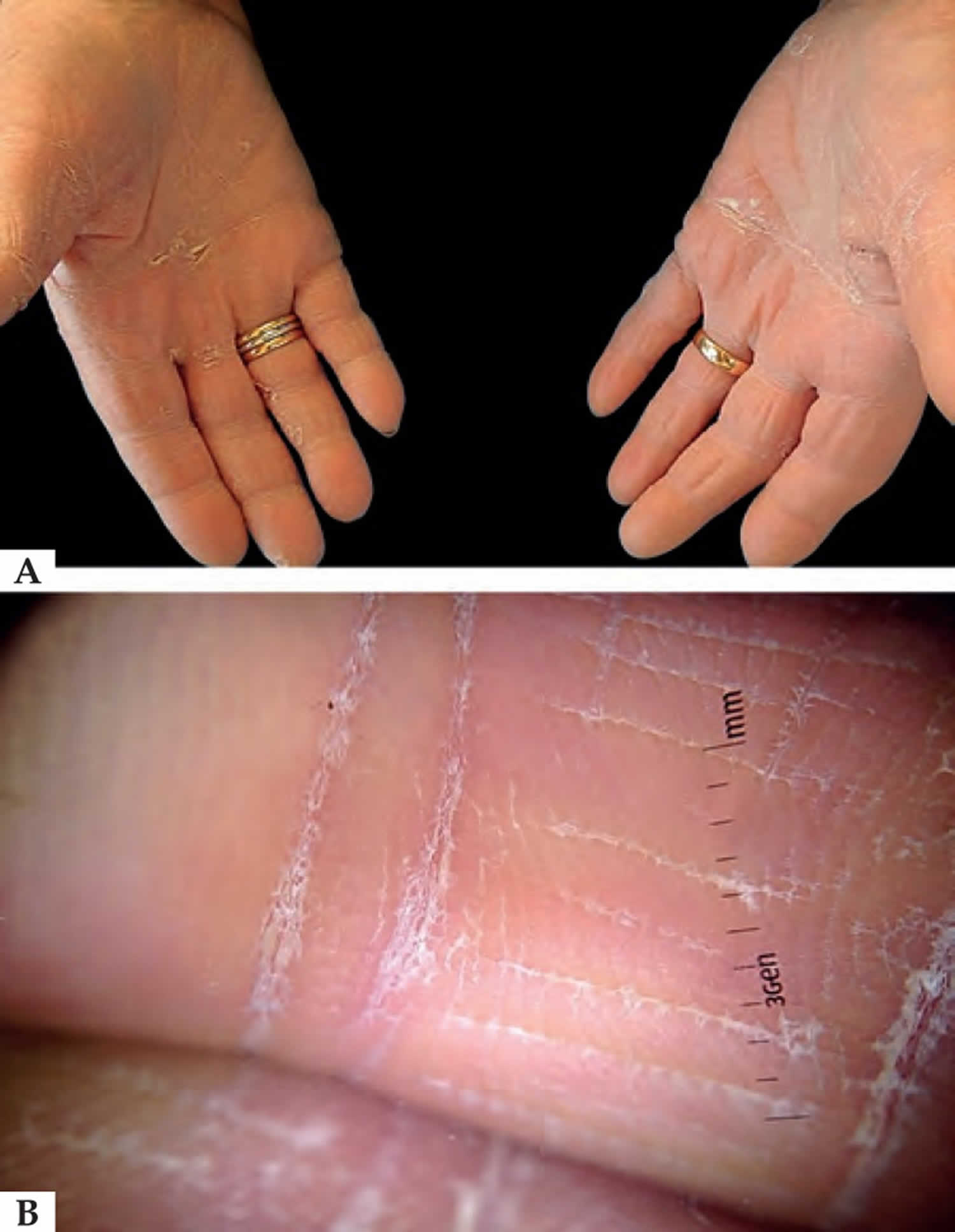
Figure 1. Tinea manuum
Footnote: Clinical examination shows diffuse white scaling involving the palmar surface and the volar aspect of the fingers of both hands (A). Polarized light dermoscopy reveals white scaling mainly located in the creases (B).
[Source 1 ]Is tinea manuum contagious?
Yes. Tinea manuum is usually acquired by direct contact with the causative organism.
Tinea manuum results from:
- Contact with another site of infection, particularly the feet (tinea pedis) or groin (tinea cruris)
- Contact with another person with tinea
- Direct contact with an infected animal or soil
- Contact with a contaminated object such as a towel or gardening tool
It is more likely in those doing manual work, who sweat profusely (hyperhidrosis) or who already have hand dermatitis.
Preventing the spread of tinea
It is important to remember that tinea is contagious. Suggestions on how to prevent the spread of infection to others include:
- Treat tinea infections with antifungal cream.
- Wash your hands after touching infected areas.
- Do not share towels.
- Do not walk around barefoot if you have tinea pedis (tinea of the feet).
- Clean the shower, bath and bathroom floor after use.
Tinea manuum causes
Mainly, Trichophyton rubrum causes tinea manuum 5. Trichophyton interdigitale and Epidermophyton floccosum are also involved. Other occasional agents include Tricholosporum violaceum. Tricholosporum rubrum accounts for about 70% of the cases 6.
Risk factors include:
- A hot and humid environment
- Contact with another site of infection, particularly the feet (tinea pedis) or groin (tinea cruris)
- Contact with another person with tinea
- Direct contact with an infected animal or soil
- Contact with a contaminated object such as a towel or gardening tool
- Excess sweating
- Prolonged exposure to water
Risk factors for tinea manuum
Tinea manuum results from:
- Contact with another site of infection, particularly the feet (tinea pedis) or groin (tinea cruris)
- Contact with another person with tinea
- Direct contact with an infected animal or soil
- Contact with a contaminated object such as a towel or gardening tool
It is more likely in those doing manual work, who sweat profusely (hyperhidrosis) or who already have hand dermatitis.
Tinea manuum prevention
Overheating and perspiration contribute to tinea infections. Suggestions to avoid tinea infection include:
- After washing, dry the skin thoroughly, particularly between the toes and within skin folds.
- Expose the skin to the air as much as possible.
- Wear cotton socks instead of synthetics.
- Use antiperspirants to control excessive perspiration (sweating).
- Wear thongs to swimming pools, locker rooms, gyms and other communal areas.
Tinea manuum symptoms
Tinea manuum can occur as an acute inflammatory rash like tinea corporis. There is usually a raised border and clearing in the middle (ringworm). This is most likely when a zoophilic (animal) or geophilic (soil) fungus is responsible. The likely fungi are 4:
- Trichophyton erinacei — from a hedgehog 7. Trichophyton erinacei is the most common dermatophyte isolated in hedgehogs, with infection rates of 20% to 47% 8. Other than hedgehog exposure, other reported exposures include an elephant 9 and direct human-to-human contact by kissing 10.
- Trichophyton verrucosum — from cattle
- Microsporum canis — from a cat or dog
- Nannizzia gypsea — from the soil
More frequently, tinea manuum causes a slowly extending area of peeling, dryness and mild itching on the palm of one hand (hyperkeratotic tinea). Skin markings may be increased. Generally, both feet appear similar (“one hand, two-foot syndrome”). The usual cause is an anthropophilic (human) fungus 4:
- Trichophyton rubrum
- Trichophyton interdigitale
- Epidermophyton floccosum.
These fungi may also cause a blistering rash on the edges of the fingers or palm. The blisters appear in crops and contain a sticky clear fluid. They may have a peeling edge. This form of tinea manuum itches and burns.
Tinea manuum diagnosis
The diagnosis of tinea manuum is confirmed by microscopy and culture of skin scrapings (see laboratory tests for fungal infection).
Tinea manuum treatment
Tinea manuum, tinea corporis, tinea cruris, and tinea pedis are generally responsive to topical creams such as terbinafine (Lamisil) and butenafine (Lotrimin Ultra), but oral antifungal agents may be indicated for extensive disease, failed topical treatment, immunocompromised patients, or severe moccasin-type tinea pedis 3. For adults, terbinafine given orally in a dosage of 250 mg/day produces rapid and long-lasting remissions. Itraconazole, an orally active azole of the triazole series acting through the inhibition of the cytochrome P450-dependent demethylation stage in the formation of ergosterol on the fungal cell membrane is effective in regimens of 200 mg/day for 30 days. Fluconazole is given in a regimen of 150 mg/week for a longer duration. Griseofulvin 500 to 1000 mg/day may also be used. For children, griseofulvin, 10 to 20 mg/kg/day or itraconazole 5 mg/kg/day may be used. Pulse therapy with itraconazole one week/ month is also effective.
Gastrointestinal side effects may occur with fluconazole but are uncommon. Itraconazole may cause gastrointestinal upsets, diarrhea, and peripheral edema, especially when used in conjunction with calcium channel blockers. Hepatotoxicity occurs at a much lower rate with fluconazole and itraconazole as compared to ketoconazole. Terbinafine also produces gastrointestinal upsets, and rarely, hepatitis.
Tinea management pitfalls
- Do not use nystatin to treat any tinea infection because dermatophytes are resistant to nystatin. However, nystatin is often effective for cutaneous Candida infections.
- Do not use oral ketoconazole to treat any tinea infection because of the U.S. Food and Drug Administration boxed warnings about hepatic toxicity and the availability of safer agents.
- Do not use griseofulvin to treat onychomycosis because terbinafine (Lamisil) is usually a better option based on its tolerability, high cure rate, and low cost.
- Do not use combination products such as betamethasone/clotrimazole because they can aggravate fungal infections.
- Do not use topical clotrimazole or miconazole to treat tinea because topical butenafine (Lotrimin Ultra) and terbinafine have better effectiveness and similar cost.
- Do not, in general, treat tinea capitis or onychomycosis without first confirming the diagnosis with a potassium hydroxide preparation, culture, or, for onychomycosis, a periodic acid–Schiff stain. However, kerion should be treated aggressively while awaiting test results, and it may be reasonable to treat a child with typical lesions of tinea capitis involving pruritus, scale, alopecia, and posterior auricular lymphadenopathy without confirmatory testing 11. If there is no lymphadenopathy, a confirmatory test is recommended 11.
- Do not treat tinea capitis solely with topical agents, but do combine oral therapy with sporicidal shampoos, such as selenium sulfide (Selsun) or ketoconazole.
- Do not perform potassium hydroxide preparations or cultures on asymptomatic household members of children with tinea capitis, but do consider empiric treatment with a sporicidal shampoo 11.
- Errichetti E, Stinco G. Dermoscopy in tinea manuum. An Bras Dermatol. 2018;93(3):447–448. doi:10.1590/abd1806-4841.20186366 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6001110
- Elewski BE, Hughey LC, Sobera JO, Hay R. Fungal Diseases. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Dermatology. 3rd ed. Vol. 2. Philadelphia: Elsevier-Saunders; 2012. pp. 1251–1284.
- Diagnosis and Management of Tinea Infections. Am Fam Physician. 2014 Nov 15;90(10):702-711. https://www.aafp.org/afp/2014/1115/p702.html
- Tinea manuum. https://dermnetnz.org/topics/tinea-manuum
- Nigam PK, Saleh D. Tinea Pedis. [Updated 2020 Feb 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470421
- Lipner SR, Scher RK. Onychomycosis: Clinical overview and diagnosis. J Am Acad Dermatol. 2019;80(4):835–851. doi:10.1016/j.jaad.2018.03.062
- Choi E, Huang J, Chew KL, Jaffar H, Tan C. Pustular tinea manuum from Trichophyton erinacei infection. JAAD Case Rep. 2018;4(6):518–520. Published 2018 Jun 2. doi:10.1016/j.jdcr.2018.01.019 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047307
- Philpot C.M., Bowen R.G. Hazards from hedgehogs: two case reports with a survey of the epidemiology of hedgehog ringworm. Clin Exp Dermatol. 1992;17(3):156–158.
- Borges-Costa J., Martins M da L. Trichophyton erinacei skin infection after recreational exposure to an elephant in Southeast Asia. Pathog Glob Health. 2014;108(1):58–59.
- Sidwell R.U., Chan I., Francis N., Bunker C.B. Trichophyton erinacei kerion barbae from a hedgehog with direct osculatory transfer to another person. Clin Exp Dermatol. 2014;39(1):38–40.
- Kelly BP. Superficial fungal infections. Pediatr Rev. 2012;33(4):e22–e37.