What is white coat syndrome
White coat syndrome is a change in blood pressure levels due to the presence of a physician or other healthcare professional. In this context, the term “white coat syndrome” may refer to three important and different clinical conditions: 1) white coat hypertension, 2) white coat effect, and 3) masked hypertension 1.
White coat syndrome is a common phenomenon noted in both hypertensive and normotensive subjects 2. Some authors attribute this blood pressure (BP) elevation effect to a neuro-endocrine reflex mediated by sympathetic nervous system 3 conditioned by the anticipated concerning of having a further illness during the blood pressure measurement 4. Although it is known that anxiety elevates blood pressure and heart rate levels, it does not seem to be the trigger for the white coat syndrome episodes in the population 5.
The American College of Cardiology and American Heart Association classify hypertension for values of systolic BP ≥130 mmHg or diastolic BP ≥80 mmHg 6. However, the 2018 Guidelines of the European Society of Hypertension and European Society of Cardiology maintained the definition of arterial hypertension as in their previous 2013 guideline 7 – office values of systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg, arguing that the clinical studies analyzed provide data for the classification of blood pressure and the definition of hypertension to remain unchanged in relation to previous European Society of Hypertension and European Society of Cardiology guidelines 8.
White coat hypertension occurs when the blood pressure readings at your doctor’s office are higher than they are in other settings, such as your home. It’s called white coat hypertension because the health care professionals who measure your blood pressure sometimes wear white coats.
It was once thought that white coat hypertension was caused by the stress that doctor’s appointments can create. Once you’d left the doctor’s office, if your blood pressure normalized, the thought was that there wasn’t a problem. Patients with white coat hypertension have been shown to be more prone to higher levels of anxiety compared with both normotensive individuals and patients with persistent high blood pressure 9. Research has also shown that patients who are prone to white coat hypertension do not hyperreact to all types of emotional stimuli. Instead, they only react to emotional stimuli that have been associated with a physician’s office or the physician 10. This situational anxiety was further investigated in a study conducted by Ogedegbe et al. 9, findings from that research suggest that patients who experience white coat hypertension may have been classically conditioned to have high anxiety at physicians’ offices as a result of negative or painful experiences with the medical office or physician.
However, some doctors think that white coat hypertension might signal that you’re at risk of developing high blood pressure as a long-term condition. If you experience white coat hypertension, you may also have a higher risk of developing certain cardiovascular problems compared with people who have normal blood pressure at all times. The same may be true for people who have masked hypertension, meaning their blood pressure is normal at the doctor’s office, but spikes periodically when measured in other settings. It’s thought that even these temporary increases in your blood pressure could develop into a long-term problem.
If you have white coat hypertension, talk to your doctor about home monitoring of your condition. Your doctor may ask you to wear a blood pressure monitor (ambulatory blood pressure monitor) for up to 24 hours to track your blood pressure during the daytime as well as while you sleep. This can help determine if your high blood pressure only occurs in the doctor’s office or if it’s a persistent condition that needs treatment.
Blood pressure measurement
Currently, two well-accepted approaches are available to measure blood pressure outside the office to detect the phenomena related to white coat syndrome:
- Home blood pressure monitoring and
- Ambulatory blood pressure monitoring.
In home blood pressure monitoring method, the individuals can easily perform their blood pressure measurement. It requires a prior training, usually given by the physician and using an appropriate validated device. This method presents some advantages because it is well accepted by the patients, besides presenting measurement accuracy and being cheaper than the ambulatory blood pressure monitoring. However, with this method, it is not possible to observe the pressure fluctuations during the patients’ sleep period and also can present errors at the time of measurement due to the use of inaccurate devices and improper manipulation of the individual 11.
Ambulatory blood pressure monitoring is considered the best method to detect blood pressure fluctuation. Recently, a large research conducted by Banegas 12 concluded that ambulatory blood pressure monitoring is a better predictor of cardiovascular mortality as well as all-cause mortality than office-measured pressure. This oscillometric method is able to monitor the blood pressure of patients for a period of 24 hours, providing more accurate blood pressure measurements due to not only the mean blood pressure obtained but also the diurnal and nocturnal variabilities 13. Moreover, ambulatory blood pressure monitoring does not depend on the patients’ handling, provides more precise blood pressure information on the individuals’ routine, demonstrates nocturnal hypertension, evaluates the 24 hours efficacy of antihypertensive therapy, and as mentioned before, it is a strong predictor of cardiovascular morbidity and mortality compared with the office measurement.40 On the other hand, it presents some disadvantages such as reluctance of some patients to perform the examination due to the discomfort it causes and the possibility of inaccurate readings during the patients’ activities that cause an imperfect reproducibility 14.
Both home blood pressure monitoring and ambulatory blood pressure monitoring are indicated by the guidelines to identify cases of hypertension and white coat syndrome 6.
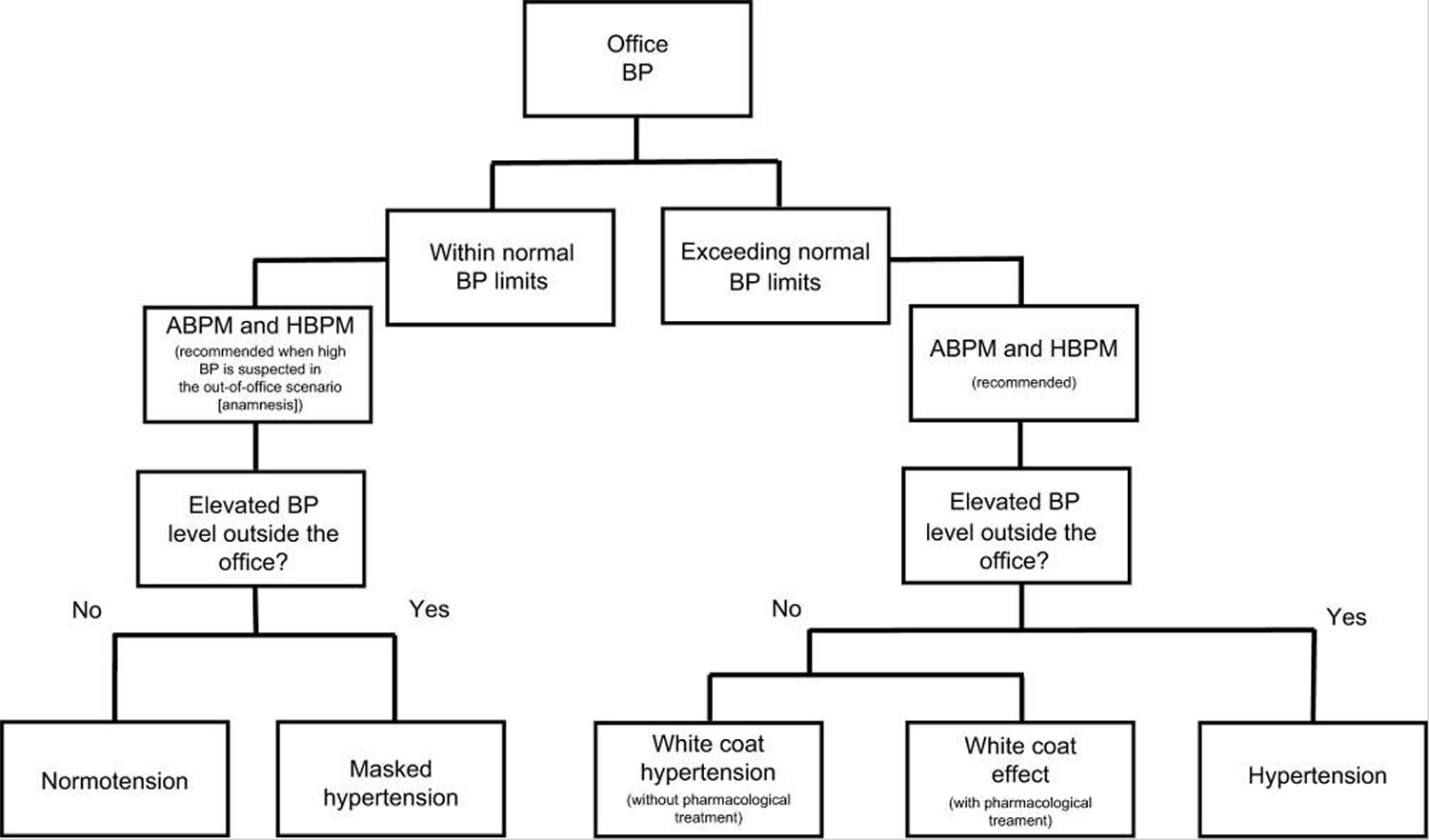
Figure 1. White coat syndrome blood pressure diagnostic pathways (flowchart of the pathway to diagnosis or classify the white coat syndrome according to the blood pressure levels.)
Footnote: Steps for diagnosis of normotension, hypertension, and phenomena related to white coat syndrome.
Abbreviations: BP = blood pressure; ABPM = ambulatory BP monitoring; BP = blood pressure; HBPM = home BP monitoring.
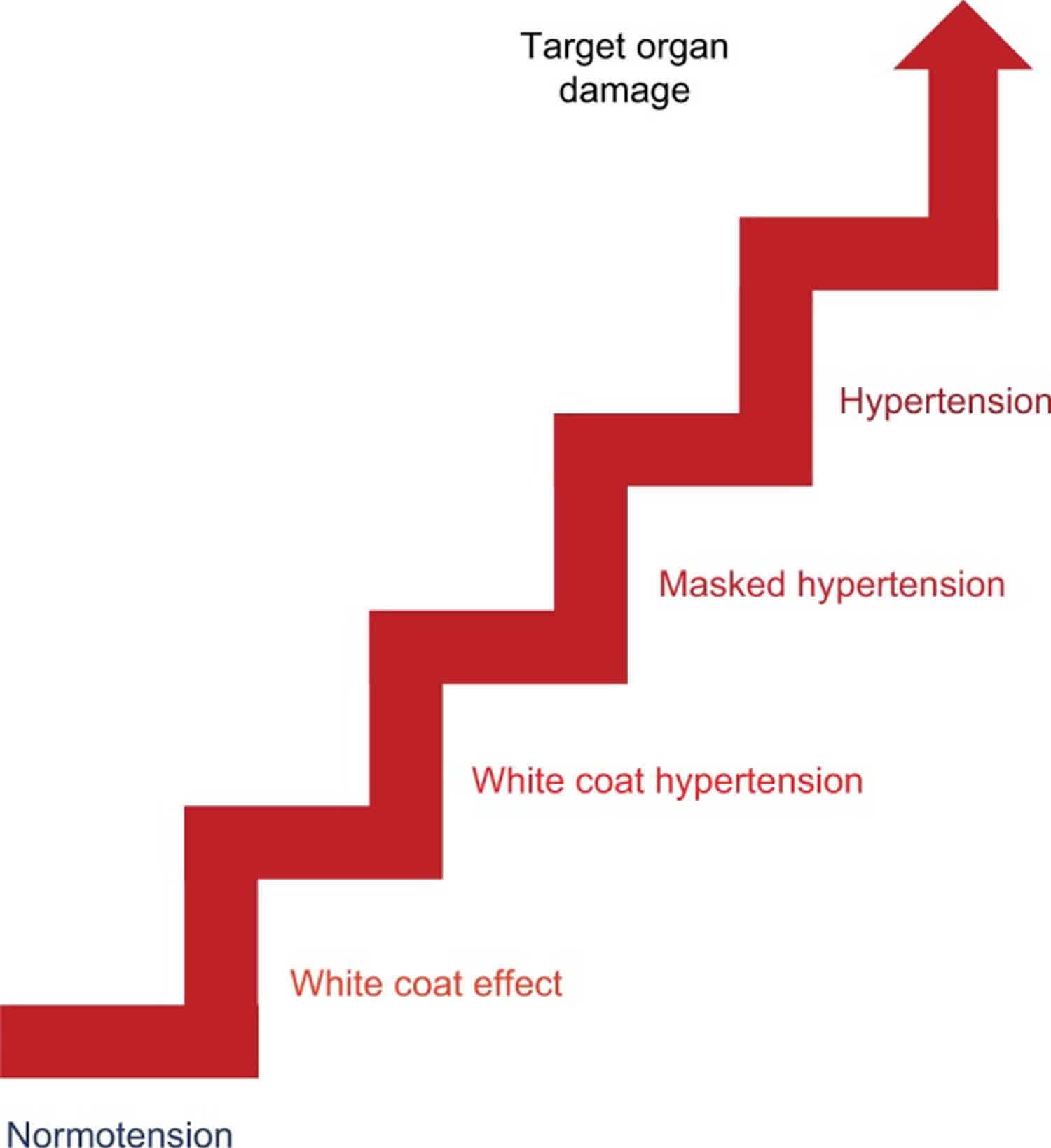
[Source 1 ]Figure 2. White coat syndrome high blood pressure levels
[Source 1 ]Table 1. Associated features of normotension, white coat syndrome, and hypertension
| Features | Normotension | White coat effect | White coat hypertension | Masked hypertension | Hypertension | |
|---|---|---|---|---|---|---|
| Within normal BP limits | Exceeding normal BP limits | |||||
| Office BP levels | ≤120/80 mmHg | >20/10 mmHg when compared to home measurements | ≥140/90 mmHg | <140/90 mmHg | <140/90 mmHg | ≥140/90 mmHg |
| 24 hours ambulatory BP monitoring levels | <130/80 mmHg | <130/80 mmHg | <130/80 mmHg | ≥130/80 mmHg | <130/80 mmHg | ≥130/80 mmHg |
| Home BP monitoring levels | <135/85 mmHg | ≤135/85 mmHg | <135/85 mmHg | ≥135/85 mmHg | <135/85 mmHg | ≥135/85 mmHg |
| Clinical characteristics | – | Higher heart rate levels and BP non-dipping condition | Higher in female sex, obese, and it seems to increase with respect to age | Increased risk of atherosclerotic cardiovascular disease, morbidity, and mortality for cardiovascular disease | Sustained elevated BP levels are related to the development of target organ damage and, consequently, increased cardiovascular risk | |
| Target organ damage | – | Low relationship with target organ damage development; correlation with arterial stiffness | Correlation with arterial stiffness and LVH | Presents a higher risk of developing target organ damage than other phenomena but less risk than hypertensive | LVH, diastolic dysfunction, carotid intima-media thickening or plaque, renal damage, and micro- as well as macro-vascular alterations | |
Abbreviations: ABPM = ambulatory BP monitoring; BP = blood pressure; CV = cardiovascular risk; CVD = cardiovascular disease; HBPM = home BP monitoring; LVH = left ventricular hypertrophy; TOD = target organ damage.
[Source 1 ]White coat syndrome blood pressure
White coat effect
Treated hypertensives may have elevated office blood pressure levels, induced by the presence of the physician or health care professional, which is called white coat effect 15. The diagnosis is confirmed when the office blood pressure presents a clinically significant elevation (>20 mmHg for Sblood pressure and >10 mmHg for Dblood pressure) when compared to out-of-office measurements of ambulatory blood pressure monitoring or home BP monitoring 16. This condition should be well evaluated as it may give the false impression of uncontrolled hypertension and the necessity of adequacy of individual’s drug therapy 17.
White coat effect was associated with higher heart rate levels and non-dipping of nocturnal blood pressure – fail in decrease of 10% of blood pressure on nocturnal levels 18. These outcomes reinforce the hypothesis that white coat effect is mediated by the overactivity of the sympathetic nervous system; and the subjects may evolve toward a worse prognosis, since the association of non-dipping with target organ damage and cardiovascular disease risk is well known 19. The white coat effect presents a high prevalence in patients with resistant hypertension (individuals with blood pressure above the recommended level, despite the concomitant use of three antihypertensive agents, being one diuretic and prescribed in ideal doses) 20 and is also closely related to ischemia silent myocardium in this group 21.
Some studies have found a correlation between white coat effect and arterial stiffness 22. Despite one study did not use the pulse wave velocity, the gold standard method, they believe that the white coat effect may be the clinical manifestation of impaired arterial compliance and might therefore be a sign of severity in the context of stable arterial hypertension 22. Additionally, they reported that white coat effect may be caused by the arterial aging since they found a correlation between white coat effect and the amplitude of the backward pressure wave, which suggest increased arterial stiffness 23.
White coat effect appears to be a less damaging phenomenon inside the group of white coat syndrome. All studies have shown a weak or low relationship between white coat effect and target organ damage development in patients with mild-to-moderate hypertension 24 and also in resistant hypertensives 25.
White coat hypertension
It is worth noting that white coat effect and white coat hypertension are often wrongly used as the same term, so one must be careful not to misinterpret these phenomena.
White coat hypertension is characterized when the individual without anti-hypertensive treatment presents high blood pressure levels (above the reference to be characterized as hypertensive) in the office, but with normal readings when measured by ambulatory blood pressure monitoring or home BP monitoring 6. Thus, if only the office reading was observed, the patients would falsely be characterized as hypertensive; therefore, the correct nomenclature is white coat hypertension. White coat hypertension is nevertheless a subgroup of the white coat effect. White coat hypertension is diagnosed after at least three occasions when office blood pressure is ≥140/90 mmHg when the mean 24-hour ambulatory blood pressure monitoring is <135/85 mmHg 8.
White coat hypertension phenomenon accounts for up to 25%–30% of subjects attending outpatient hypertension centers. The prevalence is higher in female sex, obese, and it seems to increase according to the age 26. Some authors believe that white coat hypertension is an intermediate stage between normotensive and hypertensive conditions 27. A study demonstrated that patients with white coat hypertension condition had 2.5-fold higher chances to develop a sustained hypertension compared to normotensive subjects 27. Hence, it should no longer be considered a harmless clinical state since there is a correlation between sustained high blood pressure levels with the development of target organ damage and consequent increase in cardiovascular risk.
White coat hypertension was independently associated with arterial stiffness in treated hypertensive individuals 28. Also, a study has shown that subjects with white coat hypertension had a worse vascular function and a greater cardiovascular mortality compared to prehypertensives 29. Andrikou et al 30 observed that masked hypertension and white coat hypertension presented lower pulse wave velocity when compared with individuals with sustained arterial hypertension, and these two phenomena were associated with a higher inflammatory grade and arterial stiffening when compared with normotensive subjects. In addition, some white coat hypertension and normotensive studies have found a slight worsening in the elastic properties of the aorta in individuals with white coat hypertension, but when this group is compared to individuals with sustained hypertension, the results are controversial 31. These findings may reinforce the hypothesis that subjects with white coat hypertension develop more cardiovascular disease than normotensive individuals 32.
Recently, Androulakis et al 33 observed that individuals with white coat hypertension have higher levels of left ventricular mass index when compared to normotensives. This result corroborates with previous findings, which suggest that white coat hypertension subjects present an intermediate risk between normotensive and hypertension in children 34 and adults 35 for developing left ventricular hypertrophy (LVH). The prevalence of left ventricular hypertrophy found in individuals with white coat hypertension is 8%, and it increases to 36% when associated with metabolic syndrome 36, contrasting with no case of left ventricular hypertrophy found in the control subjects for that analyses.
Hypertensive subjects also present a greater chance to develop renal damage. However, some studies have shown that children and elderly with white coat hypertension present no significant difference in albuminuria when compared to normotensives 37. Although few studies have explored this matter, these results may infer that patients with white coat hypertension have less renal involvement than individuals with established hypertension 38 – though it can only be speculated.
Masked hypertension
Masked hypertension is characterized as an inverse condition of white coat hypertension – adequate blood pressure levels in the office (<140/90 mmHg) but high levels outside the office by ambulatory blood pressure monitoring (≥130/80 mmHg) or home BP monitoring (≥135/85 mmHg) 39. According to the European Society of Hypertension, this definition should be used only for those who do not treat hypertension 40.
Masked hypertension may be suspected in young individuals with normal blood pressure in the office but who present with left ventricular hypertrophy, diabetes, and/or obesity, a family history of hypertension, many cardiovascular disease factors, or even a high office blood pressure at any moment 14. Currently, it is considered that the prevalence of masked hypertension varies between 15% and 30% 41. This phenomenon is strongly associated with the increased risk of atherosclerotic cardiovascular disease in different populations 42 and with an increased risk of morbidity and mortality for cardiovascular disease 43.
Most studies have compared masked hypertension with white coat hypertension because they were classified as “opposite” phenomena and, although both may present similar characteristics, it has been observed that masked hypertension is more related to target organ damage than white coat hypertension 44.
In relation to target organ damage, individuals with masked hypertension have thickening and lower complacency of the carotid artery in comparison with normotensive, despite no significant hemodynamic and blood pressure differences when compared to hypertensive patients 45. It was also observed that individuals with untreated masked hypertension condition present a higher risk of left ventricular structural alterations compared to the normotensive counterparts 46.
Hypertension presents harmful consequences for the patients, and interestingly, masked hypertension subjects are also accompanied by an increased risk of target organ damage 11 followed by the subjects with white coat hypertension. Additionally, masked hypertension and white coat hypertension conditions are independently associated with major cardiovascular events when compared to normotensives 47.
Taken together, the findings of most studies undoubtedly indicated that individuals with white coat syndrome have an increased target organ damage when compared with individuals with normal blood pressure levels. It is suggested that the target organ damage development in subjects with white coat syndrome, primarily in masked hypertension, could be close to the risk associated with hypertensive subjects.
How to get over white coat syndrome
There is no treatment or ways to overcome white coat syndrome. If you have white coat syndrome, talk to your doctor about home blood pressure monitoring of your condition. Your doctor may ask you to wear a blood pressure monitor (ambulatory blood pressure monitor) for up to 24 hours to track your blood pressure during the daytime as well as while you sleep. This can help determine if your high blood pressure only occurs in the doctor’s office or if it’s a persistent condition that needs treatment.
Currently, two well-accepted approaches are available to measure blood pressure outside the office to detect the phenomena related to white coat syndrome:
- Home blood pressure monitoring and
- Ambulatory blood pressure monitoring.
Ambulatory blood pressure monitoring may be the most effective method for diagnosing and confirming whether patients are persistently hypertensive or experiencing white coat syndrome 48. Ambulatory blood pressure monitoring should be used to confirm the diagnosis of white coat hypertension within 3 months, and then every 6 months thereafter, as well as to provide continued monitoring of these patients, as there is a risk of developing true hypertension 49. In the clinical/office setting, measuring patient blood pressure in a quiet room with an automatic device may reduce the magnitude of the difference between office and out-of-office blood pressure measurements 50.
There may be other techniques that can, in the future, enhance the doctor–patient relationship, and thereby reduce patient anxiety and white coat syndrome. Ideally, the utilized techniques should focus on providing information and reducing stress before office visits. Some past interventions to improve patient communication, for example, have involved waiting room interventions to improve communication about pain by using health educators 51 and increasing patient-initiated communication through having health educators coach participants to ask questions and to express concerns 52. Interventions using health educators might be useful in working with patients to reduce stress and anxiety before medical visits.
Telemedicine presents another alternative for changing the physician–patient relationship to reduce white coat hypertension and anxiety. There are many methods of telemedicine, such as email communication and interactive video medical visits, that could be used to change the typical communication process and potentially reduce anxiety. There is evidence that patient-centered communication and patient involvement in care can still occur in telemedicine at the same level as they do in face-to-face interactions 53. Studies show that patient satisfaction can be achieved through this form of medical care, but much more research in this area is needed 54.
When using telemedicine for hypertension care, studies have shown the potential to improve the accurate diagnosis of essential hypertension as well. The telemedicine service consists of using an automatic home blood pressure monitor connected to a landline telephone to transmit the data. The blood pressure readings are then transmitted to the patient’s physician. Results from this study indicated that 64% of patients using this service were diagnosed with essential hypertension, whereas only 26% of patients not using this service were correctly diagnosed with hypertension. Furthermore, those in the telemedicine service group were able to have a diagnosis earlier than those not using this service 55. Not only are patients able to be diagnosed earlier in the illness’s progression, but past research has also demonstrated that the use of telemedicine can improve medication adherence and blood pressure control, along with improving health outcomes, thereby possibly also reducing the use of health care services and associated costs 56. Although this use of technology has not been studied in patients with white coat hypertension, the results and implications of these previous studies could have beneficial effects on these patients, leading to a greater likelihood of optimal health.
References- Pioli MR, Ritter AM, de Faria AP, Modolo R. White coat syndrome and its variations: differences and clinical impact. Integr Blood Press Control. 2018;11:73-79. Published 2018 Nov 8. doi:10.2147/IBPC.S152761 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233698/
- Pickering TG. Blood pressure measurement and detection of hypertension. Lancet. 1994;344(8914):31–35.
- Mancia G, Bertinieri G, Grassi G, et al. Effects of blood-pressure measurement by the doctor on patient’s blood pressure and heart rate. Lancet. 1983;2(8352):695–698
- Bloomfield DA, Park A. Decoding white coat hypertension. World J Clin Cases. 2017;5(3):82–92
- Terracciano A, Scuteri A, Strait J, et al. Are personality traits associated with white-coat and masked hypertension? J Hypertens. 2014;32(10):1987–1992. discussion 1992
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324.
- Mancia G, Fagard R, Narkiewicz K, et al. Task Force Members 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31(7):1281–1357
- Williams B, Mancia G, Spiering W, et al. Authors/Task Force Members 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) 2018;36(10):1953–2041.
- The misdiagnosis of hypertension: the role of patient anxiety. Ogedegbe G, Pickering TG, Clemow L, Chaplin W, Spruill TM, Albanese GM, Eguchi K, Burg M, Gerin W. Arch Intern Med. 2008 Dec 8; 168(22):2459-65.
- Comparison of the cardiovascular effects of different laboratory stressors and their relationship with blood pressure variability. Parati G, Pomidossi G, Casadei R, Ravogli A, Groppelli A, Cesana B, Mancia G. J Hypertens. 1988 Jun; 6(6):481-8.
- Parati G, Stergiou GS, Asmar R, et al. ESH Working Group on Blood Pressure Monitoring European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010;24(12):779–785.
- Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship between Clinic and Ambulatory Blood-Pressure Measurements and Mortality. N Engl J Med. 2018;378(16):1509–1520
- Sociedade Brasileira de Cardiologia (SBC); Sociedade Brasileira de Hipertensão (SBH); Sociedade Brasileira de Nefrologia (SBN) V Diretrizes Brasileiras de Monitoração Ambulatorial Da Pressão Arterial (MAPA V) e III Diretrizes de Monitoração Residencial da Pressão Arterial (MRPA III) [V Guidelines for ambulatory blood pressure monitoring (ABPM) and III Guidelines for home blood pressure monitoring (HBPM)] Arq Bras Cardiol. 2011;97(3 Suppl 3):1–24. Portuguese
- O’Brien E, Parati G, Stergiou G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31(9):1731–1768.
- Celis H, Fagard RH. White-coat hypertension: a clinical review. Eur J Intern Med. 2004;15(6):348–357
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324
- Malachias MVB, Gomes MAM, Nobre F, et al. 7th Brazilian Guideline of Arterial Hypertension: Chapter 2 – Diagnosis and Classification. Arq Bras Cardiol. 2016;107(3 Suppl 3):7–13. English, Portuguese
- Bochud M, Bovet P, Vollenweider P, et al. Association between white-coat effect and blunted dipping of nocturnal blood pressure. Am J Hypertens. 2009;22(10):1054–1061
- Cuspidi C, Meani S, Salerno M, et al. Cardiovascular target organ damage in essential hypertensives with or without reproducible nocturnal fall in blood pressure. J Hypertens. 2004;22(2):273–280.
- Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403–1419
- Modolo R, Ruggeri Barbaro N, de Faria AP, et al. The white-coat effect is an independent predictor of myocardial ischemia in resistant hypertension. Blood Press. 2014;23(5):276–280.
- de Simone G, Schillaci G, Chinali M, et al. Estimate of white-coat effect and arterial stiffness. J Hypertens. 2007;25(4):827–831.
- Fujita H, Matsuoka S, Awazu M. White-Coat and Reverse White-Coat Effects Correlate with 24-h Pulse Pressure and Systolic Blood Pressure Variability in Children and Young Adults. Pediatr Cardiol. 2016;37(2):345–352
- Kristensen KS, Høegholm A, Bang LE, et al. No impact of blood pressure variability on microalbuminuria and left ventricular geometry: analysis of daytime variation, diurnal variation and ‘white coat’ effect. Blood Press Monit. 2001;6(3):125–131.
- Figueiredo VN, Martins LC, Boer-Martins L, et al. The white coat effect is not associated with additional increase of target organ damage in true resistant hypertension. Med Clin (Barc) 2013;140(1):1–5
- Cuspidi C, Sala C, Grassi G, Mancia G. White coat hypertension: to treat or not to treat? Curr Hypertens Rep. 2016;18(11):80.
- Mancia G, Bombelli M, Facchetti R, et al. Long-term risk of sustained hypertension in white-coat or masked hypertension. Hypertension. 2009;54(2):226–232
- Barochiner J, Aparicio LS, Alfie J, et al. Arterial Stiffness in Treated Hypertensive Patients With White-Coat Hypertension. J Clin Hypertens (Greenwich) 2017;19(1):6–10.
- Sung SH, Cheng HM, Wang KL, et al. White coat hypertension is more risky than prehypertension: important role of arterial wave reflections. Hypertension. 2013;61(6):1346–1353.
- Andrikou I, Tsioufis C, Dimitriadis K, et al. Similar levels of low-grade inflammation and arterial stiffness in masked and white-coat hypertension: comparisons with sustained hypertension and normotension. Blood Press Monit. 2011;16(5):218–223.
- Erdogan D, Caliskan M, Gullu H, et al. Aortic elastic properties and left ventricular diastolic function in white-coat hypertensive individuals. Blood Press Monit. 2006;11(4):191–198
- Longo D, Zaetta V, Perkovic D, et al. Impaired arterial elasticity in young patients with white-coat hypertension. Blood Press Monit. 2006;11(5):243–24
- Androulakis E, Papageorgiou N, Lioudaki E, et al. Subclinical Organ Damage in White-Coat Hypertension: The Possible Role of Cystatin C. J Clin Hypertens (Greenwich) 2017;19(2):190–197.
- Lande MB, Meagher CC, Fisher SG, et al. Left ventricular mass index in children with white coat hypertension. J Pediatr. 2008;153(1):50–54
- Ihm SH, Youn HJ, Park CS, et al. Target organ status in white-coat hypertensives: usefulness of serum procollagen type I propeptide in the respect of left ventricular diastolic dysfunction. Circ J. 2009;73(1):100–105
- Mulè G, Nardi E, Cottone S, et al. Metabolic syndrome in subjects with white-coat hypertension: impact on left ventricular structure and function. J Hum Hypertens. 2007;21(11):854–860.
- Seeman T, Pohl M, Palyzova D, John U. Microalbuminuria in children with primary and white-coat hypertension. Pediatr Nephrol. 2012;27(3):461–467
- Høegholm A, Bang LE, Kristensen KS, Nielsen JW, Holm J. Microalbuminuria in 411 untreated individuals with established hypertension, white coat hypertension, and normotension. Hypertension. 1994;24(1):101–105
- Kang YY, Li Y, Huang QF, et al. Accuracy of home versus ambulatory blood pressure monitoring in the diagnosis of white-coat and masked hypertension. J Hypertens. 2015;33(8):1580–1587.
- Williams B, Mancia G, Spiering W, et al. Authors/Task Force Members 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) 2018;36(10):1953–2041
- Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens. 2014;28(9):521–528.
- Anstey DE, Booth JN, 3rd, Abdalla M, et al. Predicted Atherosclerotic Cardiovascular Disease Risk and Masked Hypertension Among Blacks in the Jackson Heart Study. Circ Cardiovasc Qual Outcomes. 2017;10(7):e003421
- Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship between Clinic and Ambulatory Blood-Pressure Measurements and Mortality. N Engl J Med. 2018;378(16):1509–1520.
- Yoon HJ, Ahn Y, Park JB, et al. Are metabolic risk factors and target organ damage more frequent in masked hypertension than in white coat hypertension? Clin Exp Hypertens. 2010;32(7):480–485.
- Scuteri A, Morrell CH, Orru’ M, et al. Gender specific profiles of white coat and masked hypertension impacts on arterial structure and function in the SardiNIA study. Int J Cardiol. 2016;217:92–98.
- Cuspidi C, Sala C, Tadic M, et al. Untreated masked hypertension and subclinical cardiac damage: a systematic review and meta-analysis. Am J Hypertens. 2015;28(6):806–813
- Tientcheu D, Ayers C, Das SR, et al. Target Organ Complications and Cardiovascular Events Associated With Masked Hypertension and White-Coat Hypertension: Analysis From the Dallas Heart Study. J Am Coll Cardiol. 66(20):2159–2169.
- White-coat hypertension: new insights from recent studies. Franklin SS, Thijs L, Hansen TW, O’Brien E, Staessen JA. Hypertension. 2013 Dec; 62(6):982-7.
- Ambulatory blood pressure monitoring in the diagnosis and management of hypertension. Grossman E. Diabetes Care. 2013 Aug; 36 Suppl 2():S307-11.
- Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Circulation. 2005 Feb 8; 111(5):697-716.
- Street RL, Jr, Slee C, Kalauokalani DK, Dean DE, Tancredi DJ, Kravitz RL. Improving physician-patient communication about cancer pain with a tailored education-coaching intervention. Patient Educ Couns. 2010;80(1):42–47
- Kim YM, Putjuk F, Basuki E, Kols A. Increasing patient participation in reproductive health consultations: an evaluation of “Smart Patient” coaching in Indonesia. Patient Educ Couns. 2003;50(2):113–122
- Agha Z, Schapira RM, Laud PW, McNutt G, Roter DL. Patient satisfaction with physician-patient communication during telemedicine. Telemed J E Health. 2009;15(9):830–839.
- Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320(7248):1517–1520
- Rogers MA, Buchan DA, Small D, Stewart CM, Krenzer BE. Telemedicine improves diagnosis of essential hypertension compared with usual care. J Telemed Telecare. 2002;8(6):344–349.
- Friedman RH, Kazis LE, Jette A, et al. A telecommunications system for monitoring and counseling patients with hypertension. Impact on medication adherence and blood pressure control. Am J Hypertens. 1996;9(4 Pt 1):285–292.