Zollinger Ellison syndrome
Zollinger-Ellison syndrome is a rare condition that occurs when one or more tumors called gastrinomas (gastrin-producing tumors), which are located mainly in your pancreas or duodenum (part of the small intestine), cause high levels of the hormone gastrin in your blood 1. Even tiny tumors can produce large quantities of gastrin. High levels of gastrin then cause your stomach to make too much acid. Too much acid in your stomach can lead to symptoms, such as abdominal pain, vomiting blood, diarrhea, and health complications, including peptic ulcer disease and gastroesophageal reflux disease (GERD). The gastrinoma tumors are sometimes cancerous (malignant pancreatic endocrine tumor) and may spread to other areas of the body by the time of diagnosis. About 80% of cases of Zollinger-Ellison syndrome, the cause is unknown. However, about 20% to 25% of gastrinomas are caused by an inherited condition called Multiple Endocrine Neoplasia type 1 (MEN-1) 2, 3. People with a family history of MEN1 are more likely to have MEN1 and Zollinger-Ellison syndrome, therefore, MEN1 must be included in a workup if Zollinger-Ellison syndrome is highly suspicious 4.
Zollinger-Ellison syndrome is rare. Only 0.5 to 3 out of every 1 million people are diagnosed with Zollinger-Ellison syndrome each year 5. While anyone can have Zollinger-Ellison syndrome, the condition is most often diagnosed in people ages 20 to 50 years old 6. Zollinger-Ellison syndrome is slightly more common in men than in women 7.
Medications such as proton pump inhibitors (PPIs) to reduce stomach acid and heal the ulcers are the usual treatment for Zollinger-Ellison syndrome.
Doctors may recommend surgery to remove the tumors that cause Zollinger-Ellison syndrome in people who don’t have MEN1. In some cases, removing the gastrinomas will cure Zollinger-Ellison syndrome and prevent the tumors from spreading to other parts of the body. After surgery, people may still need to take PPIs to control stomach acid.
If gastrinomas are cancerous and spread to the liver, bone, or other parts of the body, doctors may recommend chemotherapy, surgery, or other cancer treatments.
See your doctor if you have a persistent, burning, aching or gnawing pain in your upper abdomen, especially if you’ve also been experiencing nausea, vomiting and diarrhea.
Tell your doctor if you’ve used over-the-counter acid-reducing medications such as omeprazole (Prilosec, Zegerid), cimetidine (Tagamet HB) or famotidine (Pepcid AC) for long periods of time. These medications may mask your symptoms, which could delay your diagnosis.
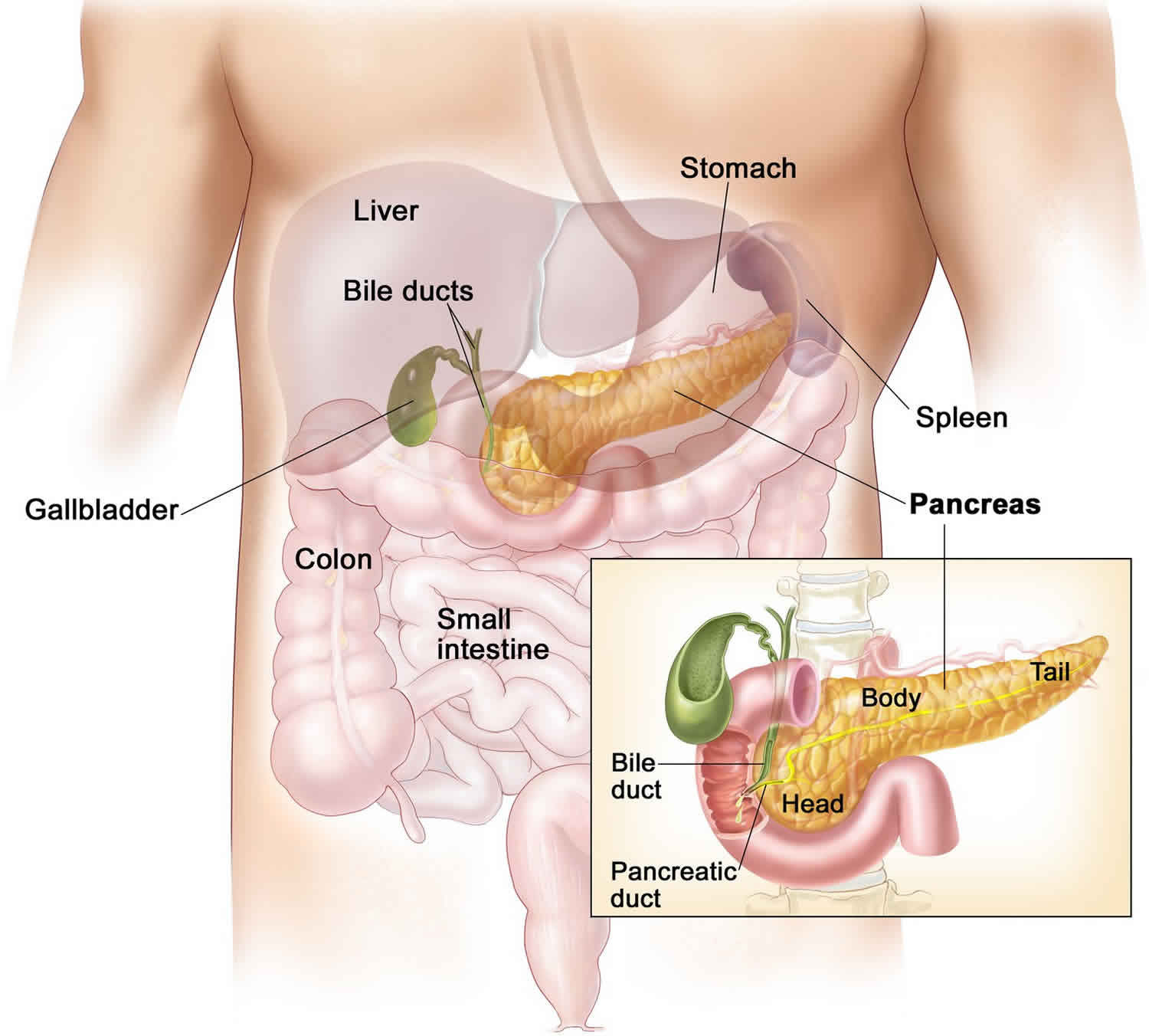
What is the pancreas
The pancreas is an organ that sits behind the stomach. It’s shaped a bit like a fish with a wide head, a tapering body, and a narrow, pointed tail. In adults it’s about 6 inches long but less than 2 inches (5 centimeters) wide.
The pancreas has 3 parts:
- the wide end is called the head. The head of the pancreas is on the right side of the abdomen (belly), behind where the stomach meets the duodenum (the first part of the small intestine).
- the bit in the middle is called the body. The body of the pancreas is behind the stomach.
- the thin end is called the tail. The tail of the pancreas is on the left side of the abdomen next to the spleen.
The pancreas is both an endocrine and exocrine gland. The endocrine part of the pancreas consists of groups of cells that are closely associated with blood vessels. These groups form “islands” of cells called pancreatic islets (islets of Langerhans). The pancreatic islets include two distinct types of cells—alpha cells, which secrete the hormone glucagon, and beta cells, which secrete the hormone insulin. Both insulin and glucagon are important hormones which help control blood sugar levels and are released directly into the blood.
About 99% of the pancreas is exocrine tissue, which secretes 1,200 to 1,500 mL of pancreatic juice per day – that are released into the small intestines to help you digest foods (especially fats). The enzymes are first released into tiny tubes called ducts. These merge to form larger ducts, which empty into the pancreatic duct. The pancreatic duct merges with the common bile duct (the duct that carries bile from the liver), and empties into the duodenum (the first part of the small intestine) at the ampulla of Vater (also known as the hepatopancreatic ampulla). The ampulla of Vater is where the pancreatic duct and bile duct join together to drain into the duodenum, which is the first part of the small intestine.
Pancreatic islets are relatively concentrated in the tail of the pancreas, whereas the head is more exocrine. Over 90% of pancreatic cancers arise from the ducts of the exocrine portion (ductal carcinomas), so cancer is most common in the head of the gland.
Figure 1. Pancreas location
Figure 2. Pancreas
Figure 3. Pancreas cell types
Zollinger Ellison syndrome signs and symptoms
Extra stomach acid can cause symptoms similar to those of peptic ulcer disease and gastroesophageal reflux disease (GERD), as well as other symptoms.
Common signs and symptoms of Zollinger-Ellison syndrome may include:
- Burning or dull pain in the abdomen or belly, between your belly button and middle of the chest
- Diarrhea, which may sometimes be the only symptom
- Burning, aching, gnawing or discomfort in your upper abdomen
- Acid reflux and heartburn
- Burping
- Nausea and vomiting
- Bleeding in your digestive tract
- Unintended weight loss
- Decreased appetite
You should see a doctor right away if you have symptoms such as:
- chest pain
- persistent vomiting
- problems breathing
- problems or pain while swallowing
- signs of bleeding in the digestive tract
- sudden, sharp stomach pain that doesn’t go away
- weakness or feeling faint
These could be signs of a complication or another serious health problem.
Zollinger Ellison complications
The extra stomach acid caused by Zollinger-Ellison syndrome can lead to peptic ulcer disease or GERD. Without treatment, these diseases can lead to complications such as:
- bleeding or perforation in the upper digestive tract
- a blockage that can stop food from moving from your stomach into your duodenum
- esophagitis or esophageal stricture
The tumors that cause Zollinger-Ellison syndrome are sometimes cancerous and may spread to other parts of your body. If the cancer spreads, it most often spreads to lymph nodes near the tumor and later to the liver and bones.
Zollinger Ellison syndrome causes
In most Zollinger-Ellison syndrome cases, experts don’t know what causes the gastrinomas to form mainly in the pancreas and duodenum. In about 20% to 25% of cases, a rare genetic disorder called MEN1 causes gastrinomas to form 2. Zollinger-Ellison syndrome begins when one or more gastrinoma tumors form in your pancreas or duodenum or at other sites such as the lymph nodes adjacent to your pancreas 8, 2.
Your pancreas sits behind and below your stomach. It produces enzymes that are essential to digesting food. The pancreas also produces several hormones including insulin, a hormone that helps to control your blood glucose. Digestive juices from the pancreas, liver and gallbladder mix in the duodenum, the part of the small intestine next to your stomach. This is where digestion reaches its peak.
The tumors that occur with Zollinger-Ellison syndrome are made up of cells that secrete large amounts of the hormone called gastrin. Increased gastrin makes the stomach produce far too much stomach acid. The excess stomach acid then leads to peptic ulcers and sometimes to diarrhea. Normally, your body releases a small amount of gastrin after you eat, and gastrin triggers your stomach to make acid.
Besides causing excess acid production, the tumors are often cancerous (malignant). Although the tumors tend to grow slowly, the cancer can spread elsewhere — most commonly to nearby lymph nodes or your liver.
Zollinger-Ellison syndrome and MEN-1
Zollinger-Ellison syndrome may be caused by an inherited condition called Multiple Endocrine Neoplasia type 1 (MEN-1). People with MEN 1 also have tumors in the parathyroid glands and may have tumors in their pituitary glands.
About 25% of people who have gastrinomas have them as part of MEN-1. They may also have tumors in the pancreas and other organs.
If you have a blood relative, such as a sibling or parent, with MEN-1, it’s more likely that you’ll have Zollinger-Ellison syndrome.
Zollinger Ellison syndrome diagnosis
Your doctor may suspect you have Zollinger-Ellison syndrome if you have certain symptoms and signs, such as:
- chronic diarrhea that occurs along with GERD or peptic ulcer disease
- peptic ulcer disease that usually is chronic, comes back repeatedly, and is severe or leads to complications
- peptic ulcer disease without Helicobacter pylori (H. pylori) infection or without a history of nonsteroidal anti-inflammatory drug (NSAID) use
- personal or family history of MEN1 or MEN1 symptoms
Your doctor will base a Zollinger-Ellison syndrome diagnosis on the following:
- Medical history. Your doctor will ask about your signs and symptoms and review your medical history.
- Blood tests. A sample of your blood is analyzed to see whether you have elevated gastrin levels. While elevated gastrin may indicate tumors in your pancreas or duodenum, it can also be caused by other conditions. For example, gastrin may also be elevated if your stomach isn’t making acid, or you’re taking acid-reducing medications, such as proton pump inhibitors. You need to fast before this test and may need to stop taking any acid-reducing medications to get the most accurate measure of your gastrin levels. Because gastrin levels can fluctuate, this test may be repeated a few times. The test is diagnostic if the gastrin level is greater than 1000 pg/ml 9. However, the fasting gastrin level can normalize after parathyroidectomy in patients with MEN1 and gastrinoma resection even though the Zollinger-Ellison syndrome is not fully cured 10.
- Secretin stimulation test. Your doctor may also perform a secretin stimulation test. For this test, your doctor first measures your gastrin levels, then gives you an injection of the hormone secretin and measures gastrin levels again. If you have Zollinger-Ellison, your gastrin levels will increase even more.
- Stomach acid tests. Doctors may order a test to check the pH or acidity of your stomach fluids. A health care professional will insert a tube through your nose, down your throat, and into your stomach to take a sample of fluid. Doctors may also measure your stomach acid pH during an upper gastrointestinal (GI) endoscopy. In some cases, doctors may order additional tests to measure the amount of acid your stomach makes.
- Upper gastrointestinal endoscopy. After you’re sedated, your doctor inserts a thin, flexible instrument with a light and video camera (endoscope) down your throat and into your stomach and duodenum to look for ulcers. Through the endoscope, your doctor may remove a tissue sample (biopsy) from your duodenum to help detect the presence of gastrin-producing tumors. Your doctor will ask you not to eat anything after midnight the night before the test.
- Endoscopic retrograde cholangiopancreatography (ERCP). Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure that combines upper gastrointestinal (GI) endoscopy and x-rays to examine the bile ducts and pancreatic ducts.
- Endoscopic ultrasound. In this procedure, your doctor examines your stomach, duodenum and pancreas with an endoscope fitted with an ultrasound probe. The probe allows for closer inspection, making it easier to spot tumors. It’s also possible to remove a tissue sample through the endoscope. You’ll need to fast after midnight the night before this test, and you’ll be sedated during the test.
- Imaging tests. Your doctor may use imaging techniques such as a nuclear scan called somatostatin receptor scintigraphy. This test uses radioactive tracers to help locate tumors. Other helpful imaging tests include ultrasound, computerized tomography (CT), magnetic resonance imaging (MRI) and 68Ga-DOTATATE PET-CT scanning.
Zollinger Ellison syndrome differential diagnosis
Differential diagnosis of hypergastrinemia includes vagotomy, peptic ulcer disease secondary to Helicobacter pylori infection, nonsteroidal anti-inflammatory drugs (NSAIDs) use, gastric outlet obstruction, renal insufficiency, short bowel syndrome, and autoimmune gastritis (Type A) 11.
The cause of peptic ulcers includes the overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and aspirin. A clinician may not be able to distinguish abdominal pain from excess acids and ulcers from peptic ulcer disease and Zollinger-Ellison syndrome, but Zollinger-Ellison syndrome causes more diarrhea and esophageal disease 10. Helicobacter pylori produce urease which acts near G cells and causes urea hydrolysis and alkalization, affecting D cells and diminishing somatostatin cell release secondary to inflammation. Gastric outlet obstruction causes antral distention which activates parietal cells via acetylcholine 11. Patients with chronic kidney disease or end-stage renal disease and undergoing dialysis have elevated serum gastrin. Gastrin clears through the kidney, and renal insufficiency will prevent the kidney from working properly. One study revealed an increase in gastric cell growth in a rat model with uremia resulted from proton back-diffusion in the stomach causing less mucosal barrier protection 11. Gastric outlet obstruction causes distension of the antrum which activates parietal cells via acetylcholine and results in hypergastrinemia 11.
Zollinger Ellison syndrome treatment
Treatment of Zollinger-Ellison syndrome addresses the hormone-secreting tumors as well as the ulcers they cause. Doctors treat Zollinger-Ellison syndrome with medicines and surgery.
Treatment of tumors
An operation to remove the tumors that occur in Zollinger-Ellison requires a skilled surgeon because the gastrinoma tumors are often small and difficult to locate. If you have just one tumor, your doctor may be able to remove it surgically, but surgery may not be an option if you have multiple tumors or tumors that have spread to your liver. On the other hand, even if you have multiple tumors, your doctor still may recommend removing a single large tumor. Doctors may recommend surgery to remove the tumors that cause Zollinger-Ellison syndrome in people who don’t have MEN1. In some cases, removing the gastrinomas will cure Zollinger-Ellison syndrome and prevent the tumors from spreading to other parts of the body. After surgery, people may still need to take proton pump inhibitors (PPIs) to control stomach acid.
In people who have MEN1, doctors don’t typically recommend surgery to remove the tumors that cause Zollinger-Ellison syndrome, especially if the gastrinomas are relatively small. People with MEN1 often have many small tumors, making it difficult for surgeons to find and remove them all. Doctors may recommend surgery to remove any larger tumors, which have a higher chance of spreading to other parts of the body.
In some cases, doctors advise other treatments to control tumor growth, including:
- Removing as much of a liver tumor as possible (debulking)
- Attempting to destroy the tumor by cutting off the blood supply (embolization) or by using heat to destroy cancer cells (radiofrequency ablation)
- Injecting drugs into the tumor to relieve cancer symptoms
- Using chemotherapy to try to slow tumor growth
- Having a liver transplant
Treatment of excess acid
Excess acid production can almost always be controlled. Medications known as proton pump inhibitors (PPIs) are the first line of treatment. Proton pump inhibitors (PPIs) lower the amount of acid your stomach makes, which can relieve symptoms and promote healing. Doctors may prescribe a higher dose of PPIs when starting treatment and may lower the dose over time. Many people with Zollinger-Ellison syndrome need lifelong treatment with PPIs.
Proton pump inhibitors (PPIs) are powerful drugs that reduce acid by blocking the action of the tiny “pumps” within acid-secreting cells. Commonly prescribed medications include lansoprazole (Prevacid), omeprazole (Prilosec, Zegerid), pantoprazole (Protonix), rabeprazole (Aciphex) and esomeprazole (Nexium).
The dose of PPIs such as oral omeprazole and intravenous pantoprazole must be adjusted to normalize basal acid output levels to less than 15 mEq per hour and less than 5 mEq per hour for those who had surgery to decrease acid secretion 4. Eighty milligrams of pantoprazole by mouth twice daily is the typical dose 4. Patients should take this on an empty stomach 3. For those rare patients who cannot tolerate PPIs, an H2-receptor antagonist is an option 12.
Long-term use of prescription proton pump inhibitors, especially in people age 50 and older, has been associated with an increased risk of fractures of the hip, wrist and spine, according to the Food and Drug Administration. This risk is small and should be weighed against the acid-blocking benefits of these medications.
Long-term use of prescription proton pump inhibitors to treat Zollinger-Ellison syndrome may also lead to low levels of vitamin B12.
Octreotide (Sandostatin), a medication similar to the hormone somatostatin, may counteract the effects of gastrin and be helpful for some people.
Talk with your doctor about the risks and benefits of these medicines.
Zollinger Ellison syndrome prognosis
Because Zollinger-Ellison syndrome involves gastrinoma, its the prognosis is based on whether the gastrinomas are benign or malignant 4. About 60% to 90% of gastrinomas are malignant with metastasis to the lymph nodes, liver, or distant organs. Fifty percent of pancreatic gastrinomas have a 50% incidence, and 10% of duodenal gastrinomas have a 10% incidence to the liver. Metastasis to the liver has a direct effect on overall survival as pancreatic gastrinomas have lower long-term survival rates than duodenal gastrinomas 4. The patients with liver metastases have a 15% 10-year survival after the surgery, but those without liver metastases have a 95% 20-year survival which is a significant finding 3.
On the other hand, duodenal gastrinomas have a higher incidence of lymph node metastases than pancreatic gastrinomas, 70% versus 40% respectively. However, lymph node involvement did not show a decrease in survival without liver metastases 13, 14.
References- Roy PK, Venzon DJ, Feigenbaum KM, Koviack PD, Bashir S, Ojeaburu JV, Gibril F, Jensen RT. Gastric secretion in Zollinger-Ellison syndrome. Correlation with clinical expression, tumor extent and role in diagnosis–a prospective NIH study of 235 patients and a review of 984 cases in the literature. Medicine (Baltimore). 2001 May;80(3):189-222. doi: 10.1097/00005792-200105000-00005
- Jensen RT, Ito T. Gastrinoma. [Updated 2020 Nov 21]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279075
- Krampitz GW, Norton JA. Current management of the Zollinger-Ellison syndrome. Adv Surg. 2013;47:59-79. doi: 10.1016/j.yasu.2013.02.004
- Cho MS, Kasi A. Zollinger Ellison Syndrome. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537344
- Jensen RT. Chapter 57: Zollinger-Ellison syndrome. In: Podolsky DK, Camilleri M, Fitz G, et al, eds. Yamada’s Textbook of Gastroenterology. 6th ed. John Wiley & Sons Ltd; 2016:1078–1102.
- Zollinger-Ellison syndrome (gastrinoma): Clinical manifestations and diagnosis. https://www.uptodate.com/contents/zollinger-ellison-syndrome-gastrinoma-clinical-manifestations-and-diagnosis
- Berna MJ, Hoffmann KM, Serrano J, Gibril F, Jensen RT. Serum gastrin in Zollinger-Ellison syndrome: I. Prospective study of fasting serum gastrin in 309 patients from the National Institutes of Health and comparison with 2229 cases from the literature. Medicine (Baltimore). 2006 Nov;85(6):295-330. doi: 10.1097/01.md.0000236956.74128.76
- Cingam SR, Botejue M, Hoilat GJ, et al. Gastrinoma. [Updated 2021 Dec 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441842
- Epelboym I, Mazeh H. Zollinger-Ellison syndrome: classical considerations and current controversies. Oncologist. 2014 Jan;19(1):44-50. doi: 10.1634/theoncologist.2013-0369
- Gibril F, Jensen RT. Zollinger-Ellison syndrome revisited: diagnosis, biologic markers, associated inherited disorders, and acid hypersecretion. Curr Gastroenterol Rep. 2004 Dec;6(6):454-63. doi: 10.1007/s11894-004-0067-5
- Phan J, Benhammou JN, Pisegna JR. Gastric Hypersecretory States: Investigation and Management. Curr Treat Options Gastroenterol. 2015 Dec;13(4):386-97. doi: 10.1007/s11938-015-0065-8
- Norton JA, Foster DS, Ito T, Jensen RT. Gastrinomas: Medical or Surgical Treatment. Endocrinol Metab Clin North Am. 2018 Sep;47(3):577-601. doi: 10.1016/j.ecl.2018.04.009
- Sutliff VE, Doppman JL, Gibril F, Venzon DJ, Yu F, Serrano J, Jensen RT. Growth of newly diagnosed, untreated metastatic gastrinomas and predictors of growth patterns. J Clin Oncol. 1997 Jun;15(6):2420-31. doi: 10.1200/JCO.1997.15.6.2420
- Roland CL, Bian A, Mansour JC, Yopp AC, Balch GC, Sharma R, Xie XJ, Schwarz RE. Survival impact of malignant pancreatic neuroendocrine and islet cell neoplasm phenotypes. J Surg Oncol. 2012 May;105(6):595-600. doi: 10.1002/jso.22118