Gallbladder polyps
Gallbladder polyps are elevated lesions on the mucosal surface of the gallbladder 1. On ultrasound a gallbladder polyp is seen as an elevation of the gallbladder wall that protrudes into the lumen 2. It should not be mobile or demonstrate posterior acoustic shadowing, which would suggest it is more likely a calculus 2. It may be sessile or pedunculated. A clearly infiltrating or large mass should be treated as a gallbladder cancer rather than a polyp 2. If there is clear reverberation or “comet tail” artefact present posterior to the lesion this should be identified as a pseudopolyp (focal adenomyomatosis or a cholesterol polyp) 3. The follow-up guidelines, therefore, do not need to be followed for these patients. Of note, not all pseudopolyps will demonstrate these findings. The vast majority of gallbladder polyps are benign (non-cancerous), but malignant forms are seen 4. On imaging, although gallbladder polyps may be detected by CT or MRI, they are usually best characterized on ultrasound as a non-shadowing and immobile polypoid ingrowth into gallbladder lumen.
Gallbladder polyp is classified according to the classification proposed by Christensen and Ishak in 1970 5. Gallbladder polyps are classified into benign tumors such as adenoma, benign pseudotumors such as adenomatous hyperplasia, adenomyoma, inflammatory polyp, cholesterol polyp, and malignant polyps such as adenocarcinoma. The reported prevalence of malignant polyps among gallbladder polyps varies from 0% to 27% 6. It is well known that gallbladder cancer at an advanced stage reveals poor prognosis even with radical resection, thus early detection and early surgical intervention is particularly important.
Gallbladder polyps are relatively frequent, seen in up to 9% of the population 7. Over 90% are benign, and the majority are cholesterol polyps. Cholesterol polyps are most frequently identified in patients between 40-50 years of age and are more common in women (female:male, 2.9:1) 8.
Gallbladder polyps may be asymptomatic, or they may be related to symptoms of cholecystitis (right upper abdominal discomfort, nausea and food intolerances) 1. Often gallbladder polyps are found inadvertently on ultrasound or CT scanning or can be incidentally found on pathologic examination of the gallbladder. Gallbladder polyps can be true neoplastic growths or pseudopolyps of cholesterol balls clinging to the wall of the gallbladder.
A wide variety of entities appear as gallbladder polyps and histology is variable:
- Benign gallbladder polyps: 95% of all polyps
- Malignant gallbladder polyps: 5% of all polyps
- adenocarcinoma: ~90% of malignant polyps
- other rare entities including:
- metastases to gallbladder
- squamous cell carcinoma
- angiosarcoma
The most common type of gallbladder polyps are pseudo or cholesterol polyps. These account for 60% to 90% of all gallbladder polyps 1. They are not true neoplastic growths, but rather they are cholesterol deposits that form as projections on the inner lumen of the gallbladder wall. They are formed from precipitation of cholesterol or bile salts. Presence of cholesterol polyps may be indicative of pathologic gallbladder disease such as chronic cholecystitis. Inflammatory polyps account for 5% to 10% of all gallbladder polyps. They are associated with inflammation of the gallbladder mucosa and wall. Usually, this type is associated with repeated bouts of cholecystitis and acute biliary colic. Both pseudopolyps and inflammatory polyps carry close to a zero risk of developing a gallbladder cancer. These polyps rarely exceed 1 cm in diameter and are often multiple. True adenomatous gallbladder polyps are considered neoplastic. They are rare and are often associated with gallstones. They can range in size from 5 mm to 20 mm. Once the polyp reaches a size of greater than 1 cm, consideration needs to be made for cholecystectomy, because of the potential malignant increases above 1 cm. Adenomyomatosis is a more common true poly. It has classically been considered a benign lesion of the fundus of the gallbladder. However, recent findings suggest these lesions do have premalignant potential. Malignant polyps tend to be singular and more than 2 cm in diameter 10.
Two percent to 12% of routine gallbladder pathology specimens may contain gallbladder polyps, but true adenomatous polyps are present in less than 0.5% of all gallbladder specimens. Cholesterol polyps show an increased cholesterol content and are associated with gallbladder cholesterolosis and sludge. Inflammatory polyps exhibit inflammation of the gallbladder wall with Rotatinski- Aschoff bodies, and findings of acute or chronic cholecystitis. True adenomatous polyps have a glandular histology. Malignant polyps can demonstrate cancerous changes characteristic of adenocarcinoma, squamous cell carcinoma, and adenoacanthoma. The degree of malignant differentiation usually correlates to polyp size 11.
Despite many available imaging modalities such as ultrasonography, computed tomography (CT), magnetic resonance imaging (MRI), endoscopic retrograde cholangiography, and endoscopic ultrasonography, it is still difficult to differentiate benign polyp and malignant polyp in gallbladder polyps 4. Therefore treatment plan of gallbladder polyp should be established with consideration of many clinicopathologic characteristics altogether with information acquired from imaging studies.
The vast majority of gallbladder polyps are asymptomatic and carry a low risk of malignant degeneration. However, a small number of true gallbladder polyps will progress to malignancy. Patients with symptomatic gallbladder polyps or with enlarging polyps should be treated with cholecystectomy. The risks of performing a laparoscopic cholecystectomy are far less than missing a potential adenomatous polyp. It is recommended that if there is any indication of a gallbladder polyp being anything other than a pseudopolyp or cholesterol polyp, that cholecystectomy should be performed 12.
Figure 1. Gallbladder polyps
Footnote: Male with previous diagnosis of ulcerative colitis. Presents with elevated liver enzymes. There are multiple polypoid lesions of the gallbadder measuring over 10mm.
[Source 13 ]Gallbladder polyps causes
There a few risk factors associated with true gallbladder polyp formation. Some studies suggest conditions such as familial polyposis, Peutz-Jeghers, Gardner syndrome, and hepatitis B may be factors associated with polyp formation. Pseudo or cholesterol polyps can develop when the cholesterol or bile salt content in the bile is high. This leads to condensation of cholesterol clumps which can adhere to the wall of the gallbladder. This condition may be a precursor to gallstone formation and can also at times be seen in conjunction with gallstones. Other factors typically associated with gallbladder diseases such as obesity, sex, weight loss, and diabetes have not been shown to increase the formation of gallbladder polyps 14.
Factors associated with an increased prevalence of gallbladder polyps is unclear. Studies have shown that 4% to 7% of the population may develop gallbladder polyps. The average age of diagnosis of gallbladder polyps is around 49 years old. However, other studies have found the presence of polyps to be more prevalent in older patients 15.
Risk factors for malignant gallbladder polyp
The reported risk factors for malignant gallbladder polyp are age of the patient, total number of polyp, morphology, size, associated gallstone, and symptomatic polyp 16. Yeh et al. 17 identified age over 50 year and polyp size over 10 mm as the independent risk factors of malignant polyps. Yang et al. 18 reported that size over 10 mm, single gallbladder polyp, the presence of gallstone, age over 50 year, and clinical symptoms were associated with malignancy. Kubota et al. 19 proposed sessile polyp, isoechogenicity with the liver parenchyma, and rapid growth were also important factors predicting malignancy. Terzi et al. 20 noted age over 60 year, size over 10 mm, and associated gallstone as the risk factors for malignancy. He et al. 21 proclaimed that cholecystectomies should be indicated in polyps with size over 10 mm and age over 50 year. Jang et al. 16 identified age, polyp size, polyp morphology as the risk factors.
Gallbladder polyp symptoms
Typically gallbladder polyps are incidentally found on upper abdominal imaging, usually during imaging for upper abdominal discomfort. Most gallbladder polyps are asymptomatic, unless large 4.
The presenting symptoms of gallbladder polyps are non specific and vague, and in many cases asymptomatic 4. For such reason, gallbladder polyps are often detected incidentally.
Patients with cholesterol stones related to hypokinetic gallbladder function, cholesterolosis, or stasis may exhibit symptoms of chronic cholecystitis. Right upper abdominal pain, food intolerance, bloating, and nausea may be present. Elicitation of a positive Murphy’s sign, pain with deep palpation to the right upper abdomen, is often present. Patients with larger adenomatous lesions may have more severe and persistent right upper abdominal pain. Cases of progressive polyps that have deteriorated into a malignancy may present with jaundice, due to growth and impingement of the common or hepatic bile duct. There may also be a palpable mass in the right upper abdomen 22.
Along with easier accessibility to routine medical check-ups, recent advancements in imaging modalities such as ultrasonography and endoscopic ultrasonography, the detection of gallbladder polyps is becoming more frequent. Although there are some differences according to reports, the prevalence of gallbladder polyps in healthy subjects is 3% to 7%, and gallbladder polyps are found in 2-12% of cholecystectomy specimens 23.
Gallbladder polyp diagnosis
Gallbladder polyps are often found coincidentally with imaging such as an abdominal CT or an abdominal ultrasound. In cases of patients being worked up for gallbladder disease, the polyps are usually seen on abdominal ultrasound. They may present as a single lesion, or they may be multiple in nature. Gallbladder polyps can occur in conjunction with gallstones but are often seen in the absence of stones. Differentiation must be made between gallstones and gallbladder polyps. Gallstones are usually mobile, and polyps are fixed to the wall of the gallbladder lumen. Most polyps are hypodense and smaller than 1 cm in diameter. They can appear polypoid or sessile. Singular polyps that have a tissue density and are larger than 1 cm in diameter carry a higher malignant potential 24.
Gallbladder polyp treatment
Gallbladder polyps that have the appearance of pseudo or cholesterol polyps, in asymptomatic patients, can be followed with yearly gallbladder ultrasounds. These patients have a very low malignant risk. If serial ultrasounds reveal that the polyp is enlarging or if the patient becomes symptomatic, then cholecystectomy should be recommended. Patients with symptoms of chronic cholecystitis are usually best treated with laparoscopic or open cholecystectomy. Gallbladder polyps that are 1 cm or greater in size should undergo cholecystectomy due to the increased risk of developing gallbladder cancer. Early intervention is preferred because an early gallbladder neoplasm has a much higher rate of cure than a more advanced lesion. In fact, stage 0 gallbladder cancer has about an 80% 5-year survival rate, and stage 1 has less than a 50% survival rate. Less than 10% of all gallbladder cancers are diagnosed at stage 1 or lower. More advanced gallbladder cancers require an open cholecystectomy with resection of the gallbladder fossa of the liver along with regional lymph node removal 25.
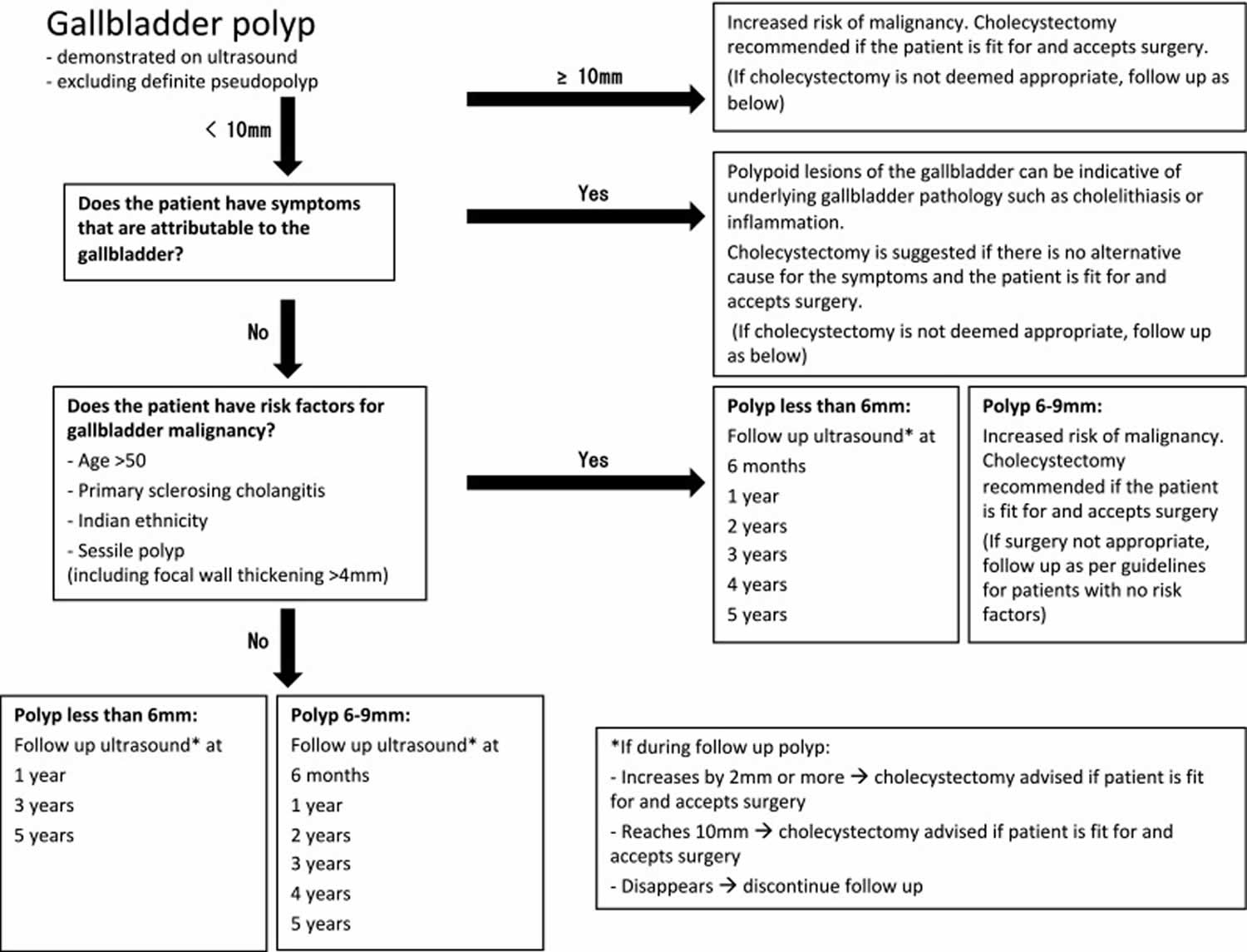
Figure 2. Gallbladder polyps management guidelines
[Source 2 ]Gallbladder polyps treatment guidelines
In 2017 joint guidelines between the European Society of Gastrointestinal and Abdominal Radiology, European Association for Endoscopic Surgery and other Interventional Techniques, International Society of Digestive Surgery – European Federation and European Society of Gastrointestinal Endoscopy were published and provide the most up to date and comprehensive guidance 2:
- Gallbladder polyp >10 mm: increased risk of malignancy, cholecystectomy recommended
- Gallbladder polyp <10 mm
- symptoms attributed to the gallbladder: cholecystectomy suggested if no other cause for the symptoms determined (polyp may be indicative of underlying occult calculus or inflammation)
- if the patient has risk factors for gallbladder malignancy (risk factors: >50 years, primary sclerosing cholangitis, Indian ethnicity, sessile polyp including focal wall thickening >4 mm):
- gallbladder polyp <6 mm
- follow-up ultrasound at 6 months, then yearly for 5 years
- an increase in size ≥2 mm: consider cholecystectomy
- gallbladder polyp >6 mm: consider cholecystectomy
- gallbladder polyp <6 mm
- no risk factors for gallbladder malignancy:
- gallbladder polyp <6 mm: follow-up ultrasound at 1, 3 and 5 years
- gallbladder polyp >6 mm:
- follow up ultrasound at 6 months, then yearly for 5 years
- an increase in size ≥2 mm: consider cholecystectomy
- no risk factors for gallbladder malignancy:
Statistically, gallbladder polyps are common and gallbladder cancer is rare, so very few polyps progress to gallbladder cancer. There is also controversy regarding the development of gallbladder cancer and some suggest that polyps may not actually progress to cancer 26.
A previously commonly accepted strategy is:
- ≤6 mm: no further follow up necessary 26
- 6-9 mm: follow up to ensure no interval growth; follow-up interval varies from 3 to 6 months 27
- ≥10 mm: surgical consultation
- usually warrants cholecystectomy
- if no cholecystectomy, annual follow up is justified 28
Lower thresholds for follow up or intervention may be warranted if the patient population is known to have a higher risk of gallbladder carcinoma (e.g. higher incidences in Pakistan, Ecuador, and females in India).
References- Jones MW, Deppen JG. Gallbladder Polyp. [Updated 2019 Mar 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470211
- Wiles R, Thoeni RF, Barbu ST, et al. Management and follow-up of gallbladder polyps : Joint guidelines between the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), European Association for Endoscopic Surgery and other Interventional Techniques (EAES), International Society of Digestive Surgery - European Federation (EFISDS) and European Society of Gastrointestinal Endoscopy (ESGE). Eur Radiol. 2017;27(9):3856–3866. doi:10.1007/s00330-017-4742-y https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5544788
- Sugiyama M, Atomi Y, Yamato T. Endoscopic ultrasonography for differential diagnosis of polypoid gall bladder lesions: analysis in surgical and follow up series. Gut. 2000;46:250–254. doi: 10.1136/gut.46.2.250.
- Kwon W, Jang JY, Lee SE, Hwang DW, Kim SW. Clinicopathologic features of polypoid lesions of the gallbladder and risk factors of gallbladder cancer. J Korean Med Sci. 2009;24(3):481–487. doi:10.3346/jkms.2009.24.3.481 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2698196
- Christensen AH, Ishak KG. Benign tumors and pseudotumors of the gallbladder. Report of 180 cases. Arch Pathol. 1970;90:423–432.
- Lee KF, Wong J, Li JC, Lai PB. Polypoid lesions of the gallbladder. Am J Surg. 2004;188:186–190.
- Uncommon Intraluminal Tumors of the Gallbladder and Biliary Tract: Spectrum of Imaging Appearances. Radiographics. 2019 Mar-Apr;39(2):388-412. doi: 10.1148/rg.2019180164. Epub 2019 Feb 1. https://doi.org/10.1148/rg.2019180164
- Levy AD, Murakata LA, Abbott RM et-al. From the archives of the AFIP. Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics. 2002 Mar-Apr;22(2):387-413. https://doi.org/10.1148/radiographics.22.2.g02mr08387
- Gallbladder cancer: the polyp-cancer sequence. Br J Surg. 1990 Apr;77(4):363-4. https://doi.org/10.1002/bjs.1800770403
- Wu T, Sun Z, Jiang Y, Yu J, Chang C, Dong X, Yan S. Strategy for discriminating cholesterol and premalignancy in polypoid lesions of the gallbladder: a single-centre, retrospective cohort study. ANZ J Surg. 2019 Apr;89(4):388-392.
- Esendağlı G, Akarca FG, Balcı S, Argon A, Erhan SŞ, Turhan N, Zengin Nİ, Keser SH, Çelik B, Bulut T, Abdullazade S, Erden E, Savaş B, Bostan T, Sağol Ö, Ağalar AA, Kepil N, Karslıoğlu Y, Günal A, Markoç F, Saka B, Özgün G, Özdamar ŞO, Bahadır B, Kaymaz E, Işık E, Ayhan S, Tunçel D, Yılmaz BÖ, Çelik S, Karabacak T, Seven İE, Çelikel ÇA, Gücin Z, Ekinci Ö, Akyol G. A Retrospective Evaluation of the Epithelial Changes/Lesions and Neoplasms of the Gallbladder in Turkey and a Review of the Existing Sampling Methods: A Multicentre Study. Turk Patoloji Derg. 2018;34(1):41-48.
- Li Y, Tejirian T, Collins JC. Gallbladder Polyps: Real or Imagined? Am Surg. 2018 Oct 01;84(10):1670-1674.
- Gallbladder polyps and primary sclerosing cholangitis. https://radiopaedia.org/cases/gallbladder-polyps-and-primary-sclerosing-cholangitis
- Liu HW, Chen CY. Ovo-lactovegetarian diet as a possible protective factor against gallbladder polyps in Taiwan: A cross-sectional study. Ci Ji Yi Xue Za Zhi. 2019 Jan-Mar;31(1):29-34.
- Torabi Sagvand B, Edwards K, Shen B. Frequency, Risk Factors, and Outcome of Gallbladder Polyps in Patients With Primary Sclerosing Cholangitis: A Case-Control Study. Hepatol Commun. 2018 Dec;2(12):1440-1445.
- Jang YS, Lee JH, Kim JY, Kim SH, Kim SG, Hwang YJ, Yun YK. Surgical outcomes and risk factors for gallbladder carcinoma of polypoid lesions of gallbladder. Korean J Hepatobiliary Pancreat Surg. 2005;9:164–170.
- Yeh CN, Jan YY, Chao TC, Chen MF. Laparoscopic cholecystectomy for polypoid lesions of the gallbladder: a clinicopathologic study. Surg Laparosc Endosc Percutan Tech. 2001;11:176–181.
- Yang HL, Sun YG, Wang Z. Polypoid lesions of the gallbladder: diagnosis and indications for surgery. Br J Surg. 1992;79:227–229.
- Kubota K, Bandai Y, Noie T, Ishizaki Y, Teruya M, Makuuchi M. How should polypoid lesions of the gallbladder be treated in the era of laparoscopic cholecystectomy? Surgery. 1995;117:481–487.
- Terzi C, Sokmen S, Seckin S, Albayrak L, Ugurlu M. Polypoid lesions of the gallbladder: report of 100 cases with special reference to operative indications. Surgery. 2000;127:622–627.
- He ZM, Hu XQ, Zhou ZX. Considerations on indications for surgery in patients with polypoid lesion of the gallbladder. Di Yi Jun Yi Da Xue Xue Bao. 2002;22:951–952.
- Chang KL, Estores DS. Upper Gastrointestinal Conditions: Gallbladder Conditions. FP Essent. 2017 Jul;458:33-38.
- Ahrendt SA, Pitt HA. Biliary tract. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Sabiston textbook of surgery: the biological basis of modern surgical practice. 17th ed. Philadelphia: Elsevier Saunders; 2004. pp. 1597–1641.
- Kopf H, Schima W, Meng S. [Differential diagnosis of gallbladder abnormalities : Ultrasound, computed tomography, and magnetic resonance imaging]. Radiologe. 2019 Apr;59(4):328-337.
- Şahiner İT, Dolapçı M. When should gallbladder polyps be treated surgically? Adv Clin Exp Med. 2018 Dec;27(12):1697-1700.
- Incidentally detected gallbladder polyps: is follow-up necessary?–Long-term clinical and US analysis of 346 patients. Radiology. 2011 Jan;258(1):277-82. doi: 10.1148/radiol.10100273. Epub 2010 Aug 9. https://doi.org/10.1148/radiol.10100273
- Andrén-Sandberg A. Diagnosis and management of gallbladder polyps. N Am J Med Sci. 2012;4(5):203–211. doi:10.4103/1947-2714.95897 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3359430
- Managing incidental findings on abdominal and pelvic CT and MRI, Part 4: white paper of the ACR Incidental Findings Committee II on gallbladder and biliary findings. J Am Coll Radiol. 2013 Dec;10(12):953-6. doi: 10.1016/j.jacr.2013.05.022. https://doi.org/10.1016/j.jacr.2013.05.022