Juvenile spring eruption
Juvenile spring eruption is a distinct sun-induced itchy skin condition (photodermatosis) appearing on the light-exposed skin of the ears, that predominantly affects boys or young men in early spring 1. Juvenile spring eruption is characterized by papules and vesicles that appeared on the helix of the ears 2. Juvenile spring eruption is considered a distinctive variant of polymorphic light eruption occurring in springtime after exposure to bright sunlight during cold weather 3. Boys and young men are more affected by juvenile spring eruption because they usually have less hair cover over the ears than girls and young women. Patients whose ears stick out are more susceptible. The eruption of juvenile spring eruption typically occurs in spring and consists of itchy red small lumps which evolve into blisters and crusts and heal with minimal or no scarring. Enlarged lymph nodes in the neck occur in some cases. The appearance of the rash is delayed 8–24 hours after sun exposure and heals in about 2 weeks, faster with treatment. Recurrences can occur, with similar climatic conditions.
As juvenile spring eruption tends to appear in small outbreaks, concomitant trigger such as parvovirus B19 infection have been postulated in the pathogenesis of juvenile spring eruption besides the well-established exposure to UV light 4.
Juvenile spring eruption is a harmless, temporary condition; it does not cause any other diseases and long-term monitoring is not required.
Juvenile spring eruption treatment is rarely indicated; short-term corticosteroids may accelerate the healing process and alleviate itching. Wearing a hat during the first sunny but cold days of spring may prevent recurrence.
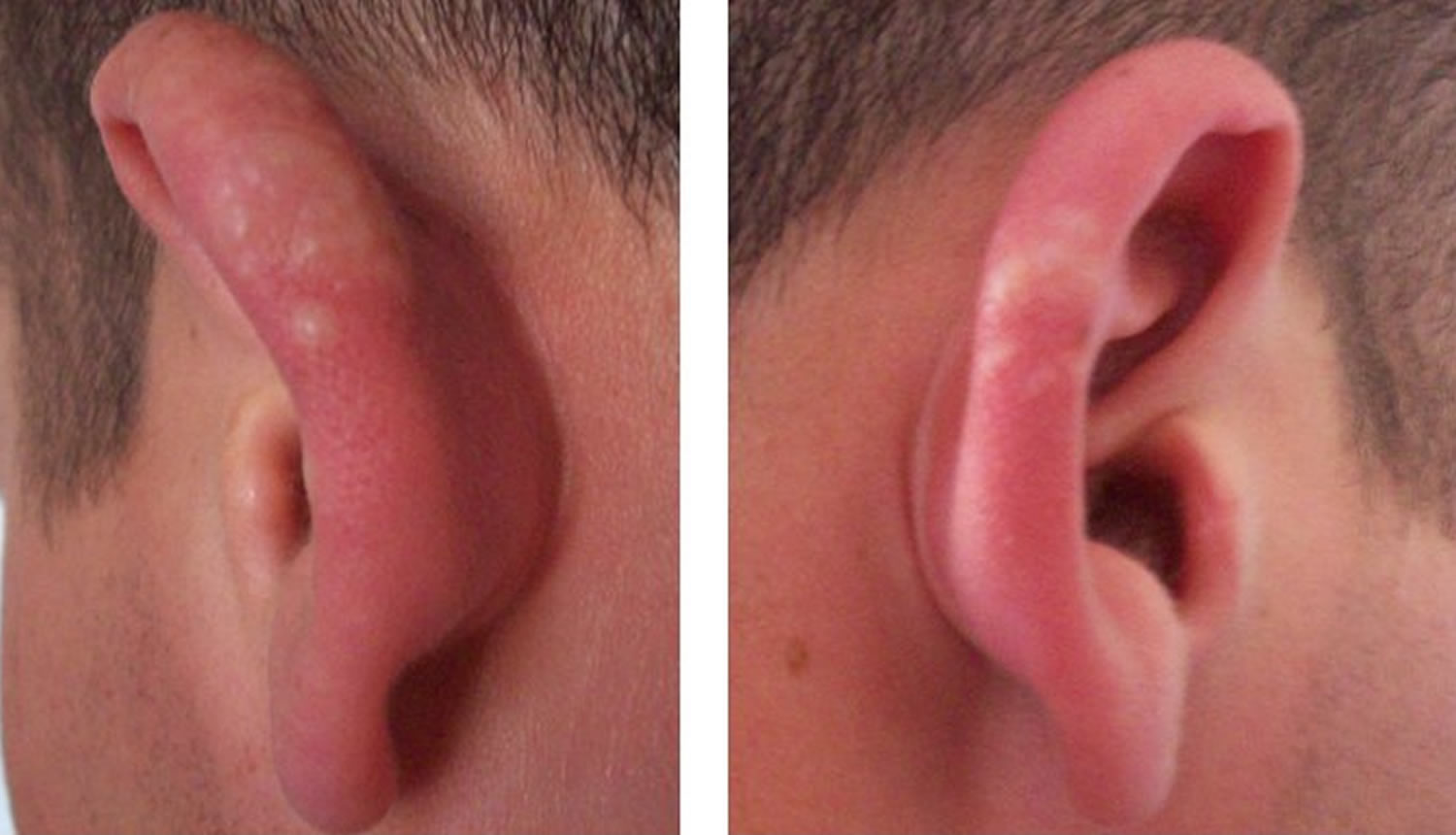
Figure 1. Juvenile spring eruption
Footnote: Helical thickening, erythema, and numerous small vesicles are present on both ears, characteristic of juvenile spring eruption.
Juvenile spring eruption causes
Juvenile spring eruption cause is unknown, but both sunlight and the cold play a role. Rare familial cases have been reported. Juvenile spring eruption is probably a localized form of polymorphic light eruption — a sun allergy rash of unknown cause which can have various appearances and affects more widespread areas of sun-exposed skin. Some patients with juvenile spring eruption also have polymorphic light eruption. Cold weather, such as can occur in the spring, is also thought to play a part in juvenile spring eruption 3.
Juvenile spring eruption symptoms
The first sign of juvenile spring eruption is slight itchiness of the ears. The skin on the ears then reddens and breaks out into blisters and scabs or more rarely, blisters on the outer edge of the helix. The backs of the hands and forearms may also be involved but this is much less common. The rash only arises in spring time, never in the summer, and is triggered by exposure to the cold in the morning. Enlarged lymph nodes in the neck occur in some cases. The appearance of the rash is delayed 8–24 hours after sun exposure and heals in about 2 weeks, faster with treatment. Recurrences can occur, with similar climatic conditions. One or more flares may arise every spring, but the disorder gradually becomes less severe and eventually disappears altogether after a few years.
Juvenile spring eruption diagnosis
Juvenile spring eruption is usually diagnosed clinically and tests are not necessary.
Juvenile spring eruption treatment
The lesions of juvenile spring eruption are treated with potent topical steroids and emollients. Antihistamines may be prescribed for the itch. The ears should be protected from sun exposure.
To prevent recurrences of juvenile spring eruption, especially when climatic conditions are conducive, hats and sunscreens should be used. Hair can be grown over the ears.
There is some evidence to support prophylactic short courses of oral steroids to prevent the eruption during a holiday break 5, hydroxychloroquine, and antioxidants such as Polypodium leucotomes extract, lycopene, beta-carotene, nicotinamide and astaxanthin 6. For moderate cases consider prednisolone enteric-coated (EC) tablets, 25 mg oral daily for five days starting the day before their holiday (if away for two weeks give an extra five days’ supply to use if needed) 7.
For more severe cases refer for consideration of phototesting and further management, for example phototherapy in springtime to promote tolerance (12-16 exposures gives four months of protection), intramuscular depot steroids and in severe cases immunosuppressive drugs such as azathioprine 7.
References- Kreuter A, Koushk Jalali B, Tigges C, Silling S, Lehmann P, Wieland U. Juvenile Spring Eruption Associated With Parvovirus B19 Infection. JAMA Dermatol. 2018;154(11):1356–1357. doi:10.1001/jamadermatol.2018.2932
- Kılıç Sayar, S. (2020), Juvenile spring eruption among soldiers: A report of a large outbreak. Australas J Dermatol. https://doi.org/10.1111/ajd.13495
- Stratigos AJ, Antoniou C, Papadakis P, et al. Juvenile spring eruption: clinicopathologic features and phototesting results in 4 cases.J Am Acad Dermatol.2004;50(2)(suppl):S57-S60. doi:10.1016/S0190-9622(03)02469-1
- Kreuter A, Koushk Jalali B, Tigges C, Silling S, Lehmann P, Wieland U. Juvenile Spring Eruption Associated With Parvovirus B19 Infection. JAMA Dermatol. 2018 Nov 1;154(11):1356-1357. doi: 10.1001/jamadermatol.2018.2932
- Lembo S, Raimondo A. Polymorphic Light Eruption: What’s New in Pathogenesis and Management. Front Med (Lausanne). 2018 Sep 10;5:252. doi: 10.3389/fmed.2018.00252
- Oakley AM, Ramsey ML. Polymorphic Light Eruption. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430886
- Polymorphic light eruption & juvenile spring eruption. http://www.pcds.org.uk/clinical-guidance/polymorphic-light-eruption-and-juvenile-spring-eruption