Lupus nephritis
Lupus nephritis is a type of kidney disease caused by systemic lupus erythematosus (SLE or lupus). Lupus or systemic lupus erythematosus (SLE) is an autoimmune disease, a disorder in which your body’s immune system attacks your body’s own cells and organs. Systemic lupus erythematosus (SLE) is the form of lupus that can harm your skin, joints, kidneys and brain and may be fatal. Lupus nephritis causes inflammation (swelling or scarring) of the small blood vessels that filter wastes in your kidney (glomeruli) and sometimes the kidneys, by attacking them like they would attack a disease. Kidney disease caused by systemic lupus erythematosus may get worse over time and lead to kidney failure. If your kidneys fail, you will need dialysis or a kidney transplant to maintain your health.
Kidney damage is one of the more common health problems caused by systemic lupus erythematosus. In adults who have systemic lupus erythematosus, as many as 5 out of 10 will have kidney disease. In children who have lupus, 8 of 10 will have kidney disease 1. About 10 to 20% of patients may progress to end stage renal disease 2.
African Americans, Hispanics/Latinos, and Asian Americans are more likely to develop lupus nephritis than Caucasians 3. Lupus nephritis is more common in men than in women 4.
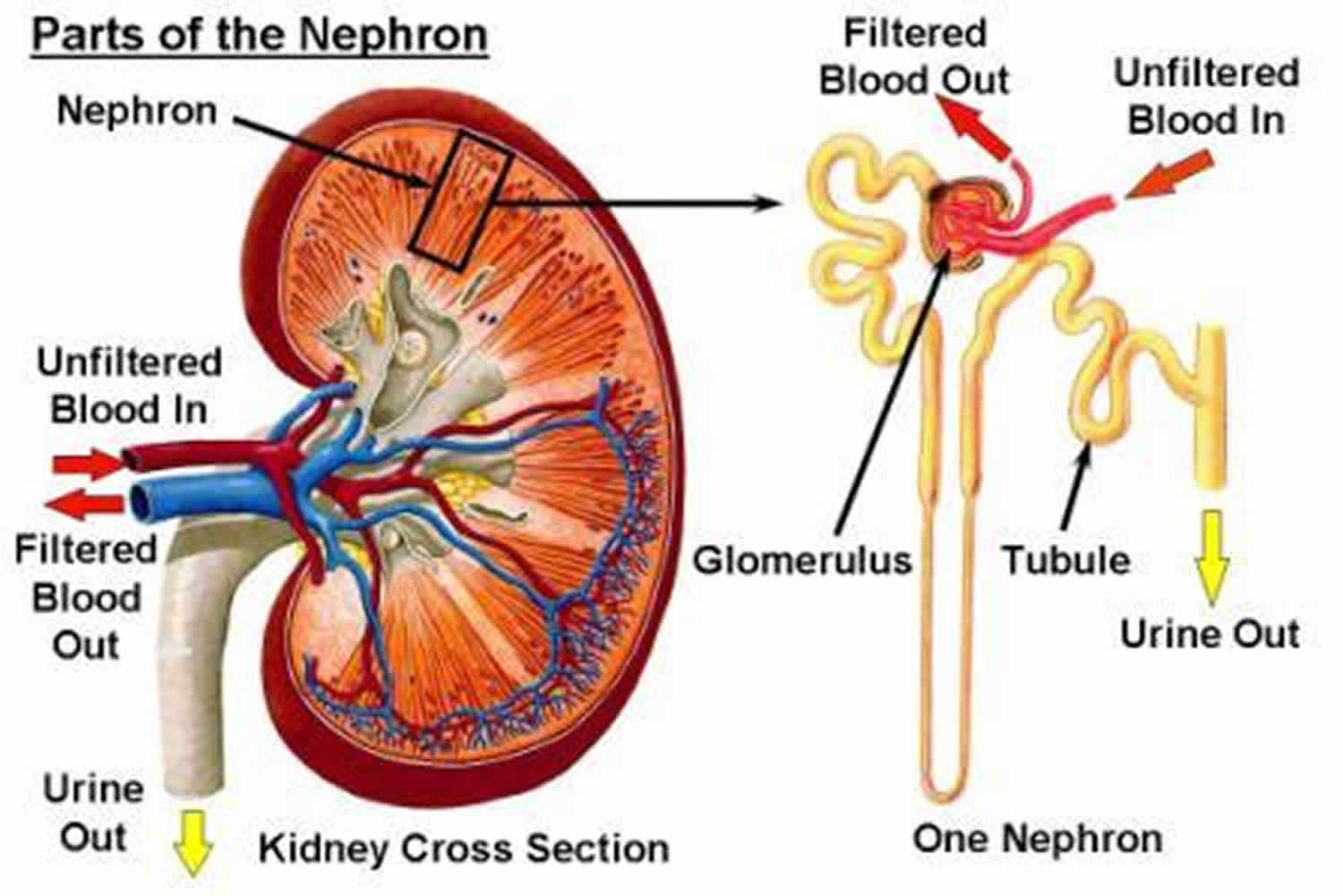
Your kidneys’ main job is to filter extra water and wastes out of your blood to make urine. To keep your body working properly, your kidneys balance the salts and minerals—such as calcium, phosphorus, sodium, and potassium that circulate in your blood. Your kidneys also make hormones that help control blood pressure, make red blood cells, and keep your bones strong.
Lupus is treated with drugs that block your body’s immune system. These include drugs like steroids (corticosteroid) and antimalarial drugs. Everyone is different and your doctor will make a treatment plan that is right for you. Usually treatment for lupus nephritis include:
- Corticosteroids (often called “steroids”)
- Immunosuppressive drugs
- Angiotensin-converting-enzyme inhibitor (ACE inhibitors) and angiotensin 2 receptor blockers (ARBs)
- Diuretics
- Diet change (reduced sodium/salt and protein)
Lupus nephritis stages
The current standardized classification system for lupus nephritis is derived from the World Health Organization (WHO) and International Society of Nephrology/Renal Pathology Society’s recommendations. The classification system is based on glomerular morphologic changes seen on microscopy, immune deposits seen on immunofluorescence, and also electronic microscopy.
- Class 1 is minimal mesangial lupus nephritis, in which glomeruli appear normal on light microscopy. Immunofluorescence shows immune complex deposits in the mesangial space.
- Class 2 is proliferative mesangial lupus nephritis since mesangial proliferation is seen on light microscopy unlike Class 1. Similar to class 1, immunofluorescence also shows immune complex deposits in the mesangial space.
- Class 3 is focal lupus nephritis. Immune complex deposits may be visualized in the mesangial, subendothelial and/or subepithelial space on immunofluorescence imaging.
- Class 4 is diffuse lupus nephritis in which immune complex deposits may occur in the mesangial, subendothelial and/or the subepithelial space. Lesions may be segmental, involving less than 50% of the glomeruli, or global, which instead involves more than 50%.
- Class 5 is membranous lupus nephritis, in which immune complex deposits are in the mesangial and subepithelial space. Capillary loops are thickened due to subepithelial immune complex deposits. At this class, nephrotic range proteinuria occurs. Class 5 may also include Class 3 and 4 pathology.
- Class 6 is advanced sclerosing lupus nephritis in which most of the glomeruli are sclerosed. However, immune complex deposits are not visualized on immunofluorescence since more than 90% of the glomeruli are scarred.
Lupus nephritis causes
Lupus nephritis is a common manifestation of systemic lupus erythematosus (SLE). Lupus nephritis is primarily caused by a type-3 hypersensitivity reaction, which results in the formation of immune complexes 2. Anti-double-stranded DNA (anti-dsDNA) binds to DNA, which forms an anti-dsDNA immune complex. These immune complexes deposit on the mesangium, subendothelial, and/or subepithelial space near the glomerular basement membrane of the kidney. This leads to an inflammatory response with the onset of lupus nephritis, in which the complement pathway is activated with a resultant influx of neutrophils and other inflammatory cells. While an autoimmune phenomenon causes lupus nephritis, there are also genetic components which may predispose an SLE patient to develop lupus nephritis. For instance, polymorphisms in the allele coding for the immunoglobulin receptors on macrophages and APOL1 gene variations found exclusively in African American populations with SLE were found to be associated with predisposition to lupus nephritis 5.
No one knows what causes lupus or systemic lupus erythematosus. Your family history and things in your environment such as infections, viruses, toxic chemicals or pollutants (car fumes, factory smoke) may play a role in causing systemic lupus erythematosus. Men and women of all ages and races get lupus. However, about 90 percent of people diagnosed with lupus are women and most often strikes during the child-bearing years.
Lupus is also more common in people of African or Asian background. African Americans and Asian Americans are about 2 to 3 times more likely to develop lupus than Caucasians 6. In the United States, 1 out of every 250 African American women will develop lupus 7.
Lupus nephritis symptoms
Lupus nephritis can cause many signs and symptoms and may be different for everyone. The symptoms of lupus nephritis may include foamy urine and edema, swelling that occurs when your body has too much fluid, usually in the legs, feet, or ankles, and less often in the hands or face. You may also develop high blood pressure.
Signs of lupus nephritis include:
- Blood in the urine (hematuria): Glomerular disease can cause your glomeruli to leak blood into your urine. Your urine may look pink or light brown from blood.
- Protein in the urine (proteinuria): Glomerular disease can cause your glomeruli to leak protein into your urine. Your urine may be foamy because of the protein.
- Edema: Having extra fluid that your kidneys cannot remove that causes swelling in body parts like your legs, ankles, or around your eyes.
- Weight gain: due to the fluid your body is not able to get rid of.
- High blood pressure
Kidney problems often start at the same time or shortly after lupus symptoms appear and can include:
- joint pain or swelling
- muscle pain
- fever with no known cause
- a red rash, often on the face, across the nose and cheeks, sometimes called a butterfly rash because of its shape
Lupus nephritis complications
Treatment works well to control lupus nephritis, so you may not have complications. However, between 10 to 30 percent of people who have lupus nephritis develop kidney failure 8.
The most severe form of lupus nephritis, called diffuse proliferative nephritis, can cause scars to form in the kidneys. Scars are permanent, and kidney function often declines as more scars form. Early diagnosis and treatment may help prevent long-lasting damage.
People who have lupus nephritis are at a high risk for cancer, primarily B-cell lymphoma —a type of cancer that begins in the cells of the immune system. They are also at a high risk for heart and blood vessel problems.
Lupus nephritis diagnosis
Lupus nephritis is diagnosed through urine and blood tests and a kidney biopsy.
Urine test
Your health care professional uses a urine sample to look for blood and protein in your urine. You collect the urine sample in a container in a health care professional’s office or lab. For the test, a nurse or technician places a strip of chemically treated paper, called a dipstick, into the urine. Patches on the dipstick change color when blood or protein is present. A high level of protein or a high number of red blood cells in the urine means kidney damage. The urine will also be examined under a microscope to look for kidney cells.
Blood test
Your health care professional uses a blood test to check your kidney function. The blood test measures creatinine, a waste product from the normal breakdown of muscles in your body. Your kidneys remove creatinine from your blood. Health care professionals use the amount of creatinine in your blood to estimate your glomerular filtration rate (GFR). As kidney disease gets worse, the level of creatinine goes up.
Kidney biopsy
A kidney biopsy is a procedure that involves taking a small piece of kidney tissue for examination under a microscope. A doctor performs the biopsy in a hospital using imaging techniques such as ultrasound or a computed tomography (CT) scan to guide the biopsy needle into the kidney. Health care professionals numb the area to limit pain and use light sedation to help you relax during the procedure.
The kidney tissue is examined in a lab by a pathologist—a doctor who specializes in diagnosing diseases.
A kidney biopsy can:
- confirm a diagnosis of lupus nephritis
- find out how far the disease has progressed
- guide treatment
The American College of Rheumatology recommends biopsies for people with signs of active lupus nephritis who have not yet been treated 1. Early diagnosis and prompt treatment may help protect your kidneys.
Lupus nephritis treatment
Doctors treat lupus nephritis with medicines that suppress your immune system so it stops attacking and damaging your kidneys. Goals of treatment are to:
- reduce inflammation in your kidneys
- decrease immune system activity
- block your body’s immune cells from attacking the kidneys directly or making antibodies that attack the kidneys
Lupus nephritis medicines
Your health care professional may prescribe a corticosteroid, usually prednisone, and a medicine to suppress your immune system, such as cyclophosphamide or mycophenolate mofetil, and hydroxychloroquine, a medicine for people who have systemic lupus erythematosus. Corticosteroids and immunosuppressive drugs are used to calm your immune system (your body’s defense system) and stop it from attacking your glomeruli.
Lupus nephritis can cause high blood pressure in some people. You may need more than one kind of medicine to control your blood pressure. Blood pressure medicines include:
- Angiotensin-converting-enzyme inhibitor (ACE inhibitors) and angiotensin 2 receptor blockers, with drug names that end in –pril or –sartan.
- Diuretics
- Beta blockers
- Calcium channel blockers
ACE inhibitors and angiotensin 2 receptor blockers (ARBs) are blood pressure medications used to reduce protein loss and control your blood pressure. Diuretics help your kidneys remove fluid from your body and control swelling. Diuretics can be used to lower your blood pressure too.
Lupus nephritis diet
If you have kidney disease, you may need to change what you eat. Dietitians are nutrition experts who can advise you about healthy eating and meal planning. Eating the right foods can help you manage your kidney disease. If you have high blood pressure, eating foods with less sodium (salt) may help you lower your blood pressure. Reducing protein in your food choices will lighten the load of wastes on your kidneys.
Lupus nephritis prognosis
Over the past 4 decades, changes in the treatment of lupus nephritis and general medical care have greatly improved both renal involvement and overall survival. During the 1950s, the 5-year survival rate among patients with lupus nephritis was close to 0% 9. The subsequent addition of immunosuppressive agents such as intravenous (IV) pulse cyclophosphamide has led to documented 5- and 10-year survival rates as high as 85% and 73%, respectively 10.
Mortality (death) in patients with end-stage renal disease due to lupus nephritis has declined significantly in recent decades. The mortality rate per 100 patient-years declined from 11.1 in 1995-1999 to 6.7 in 2010-2014. Deaths due to cardiovascular disease declined by 44% and deaths due to infection declined 63% 11.
Morbidity associated with lupus nephritis is related to the renal disease itself, as well as to treatment-related complications and comorbidities, including cardiovascular disease and thrombotic events. Progressive renal failure leads to anemia, uremia, and electrolyte and acid-based abnormalities. Hypertension may lead to an increased risk of coronary artery disease and cerebrovascular accident.
Nephrotic syndrome may lead to edema, ascites, and hyperlipidemia, adding to the risk of coronary artery disease and the potential for thrombosis. The findings from one study indicate that patients with lupus nephritis, particularly early-onset lupus nephritis, are at increased risk for morbidity from ischemic heart disease 12.
In a study of 56 children (< 18 years) with either global or segmental diffuse proliferative lupus nephritis, long-term renal outcomes were similar. Most patients reached adulthood but sustained significant renal damage. Complete remission rates were 50% and 60% in the global and segmental groups, respectively. Renal survival rates, defined as an estimated glomerular filtration rate of ≥60 mL/min/1.73 m2, were 93%, 78%, and 64 % at 1, 5, and 10 years, respectively, and corresponding patient survival rates were 98%, 96%, and 91%, respectively, with similar rates in the global and segmental groups 13.
Therapy with corticosteroids, cyclophosphamide, and other immunosuppressive agents increases the risk of infection. Long-term corticosteroid therapy may lead to osteoporosis, avascular necrosis, diabetes mellitus, and hypertension, among other complications. Cyclophosphamide therapy may cause cytopenias, hemorrhagic cystitis, infertility, and an increased risk of malignancy.
Biomarkers of renal outcome in lupus nephritis include proteinuria and serum albumin. Studies have shown that a proteinuria cut-off of less than 0.7 or 0.8 g/day at 12 months predicts good long-term renal outcome. Domingues et al reported that serum albumin > 3.7 g/dL at 12 months predicts favorable renal outcome at 48 months 14.
References- Liu CC, Kao AH, Manzi S, Ahearn JM. Biomarkers in systemic lupus erythematosus: challenges and prospects for the future. Therapeutic Advances in Musculoskeletal Disease. 2013;5(4):210–233.
- Musa R, Qurie A. Lupus Nephritis. [Updated 2019 Jan 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499817
- Diagnosis and classification of renal disease in systemic lupus erythematosus. UpToDate website. Updated March 24, 2016. Accessed October 19, 2016.
- Hahn BH, McMahon M, Wilkinson A, et al. American College of Rheumatology guidelines for screening, treatment and management of lupus nephritis. Arthritis Care & Research. 2012;64(6):797–808.
- Jorge A, Wallace ZS, Lu N, Zhang Y, Choi HK. Renal Transplantation and Survival Among Patients With Lupus Nephritis: A Cohort Study. Ann. Intern. Med. 2019 Jan 22
- Pons-Estel GJ, Alarcón GS, Scofield L, Reinlib L, Cooper GS. Understanding the epidemiology and progression of systemic lupus erythematosus. Seminars in Arthritis and Rheumatism. 2010;39(4):257–268.
- Madhok R. Systemic lupus erythematosus: lupus nephritis. BMJ Clinical Evidence. 2015 Dec 18:pii:1123.
- Ortega LM, Schultz DR, Lenz O, Pardo V, Contreras GN. Review: lupus nephritis: pathologic features, epidemiology and a guide to therapeutic decisions. Lupus. 2010;19(5):557–574.
- Lupus Nephritis. https://emedicine.medscape.com/article/330369-overview
- Dooley MA. Clinical and epidemiologic features of lupus nephritis. Wallace DJ, Hahn BH, eds. Dubois’ Lupus Erythematosus and Related Syndromes. 8th ed. Philadelphia, PA: Elsevier Saunders; 2013. 438-54.
- Jorge A, Wallace ZS, Zhang Y, Lu N, Costenbader KH, Choi HK. All-Cause and Cause-Specific Mortality Trends of End-Stage Renal Disease due to Lupus Nephritis from 1995 to 2014. Arthritis Rheumatol. 2018 Sep 18.
- Faurschou M, Mellemkjaer L, Starklint H, et al. High risk of ischemic heart disease in patients with lupus nephritis. J Rheumatol. 2011 Nov. 38(11):2400-5.
- Rianthavorn P, Buddhasri A. Long-term renal outcomes of childhood-onset global and segmental diffuse proliferative lupus nephritis. Pediatr Nephrol. 2015 Nov. 30 (11):1969-76.
- Domingues V, Levinson BA, Bornkamp N, Goldberg JD, Buyon J, Belmont HM. Serum albumin at 1 year predicts long-term renal outcome in lupus nephritis. Lupus Sci Med. 2018. 5 (1):e000271.