Patellofemoral arthritis
Patellofemoral arthritis refers to the presence of degenerative changes underneath the kneecap (the patella) and the channel-like groove in the femur (thighbone) that the patella rests in (see Figures 1 and 2). Patellofemoral arthritis occurs when the articular cartilage along the trochlear groove and on the underside of the patella wears down and becomes inflamed. When cartilage wears away, it becomes frayed and, when the wear is severe, the underlying bone may become exposed. Moving the bones along this rough surface may be painful. Patellofemoral arthritis should be considered a separate disease from medial and lateral compartment femorotibial arthritis.
The symptoms of patellofemoral arthritis can range from no symptoms to vague anterior knee pain to severe difficulties with stair climbing and descending stairs and walking. Patellofemoral arthritis is a common cause of anterior knee pain 1. The term chondromalacia is used to describe early alterations in the articular cartilage of the patella that may eventually lead to patellofemoral arthritis. The patellofemoral joint is composed of the bony patella, which is a sesamoid bone embedded in the quadriceps and patella tendons and the femur. A prepatellar bursa separates the patella from the overlying skin. The patella sits within the intracondylar or trochlear groove where the lateral condyle is of slightly greater diameter than the medial condyle. There are four articular facets: the inferior, superior, middle and medial vertical 2.
The patella is primarily stabilized medially by the medial patellofemoral ligament. This ligament originates from the adductor tubercle and inserts onto the superomedial border of the patella, resisting lateral traction of the patella. The lateral patellofemoral ligament originates from the lateral femoral condyle and attaches to the superolateral border of the patella and resists medial traction of the patella. The medial and lateral patellotibial ligaments and retinaculum also provide static stability of the joint. Dynamic stability is provided by vastus medialis, which provides medial resistance to lateral translation, and the vastus lateralis, which provides lateral resistance to medial translation. The quadriceps tendon attaching at the proximal patella creates a Q angle with a valgus axis that creates a lateral force across the patellofemoral joint. Blood supply is from the geniculate arteries: superior, medial, inferior, lateral, anterior, and descending. Sensory innervation of the anterior knee is from the lateral and anterior cutaneous branches of the femoral nerve as well as the infrapatellar branch of the saphenous nerve.
In healthy knees, the articular cartilage of the patellofemoral joint can reach a thickness of up to 7 to 8 mm; thus, it is a potent shock absorber. A complex matrix of glycosaminoglycans lowers the friction coefficient and creates a nearly frictionless surface for flexion and extension of the knee. Chondrocytes produce the proteoglycans that balance synthesis and degrade the matrix based on the chemical and biomechanical demands of the joint space.
Patellofemoral stability is provided by both the static and dynamic anatomical supporting structures. During flexion, the patella moves within the groove acting as a lever-arm, extending the functional length of the femur. In addition to a proximal-distal movement within the groove, the patella is thought to have a lateral motion with knee extension moving in a J-shaped pattern. Varus and valgus alignment of the knee, as well as any rotational component of the femur or tibia, also determine biomechanical patellofemoral function 3.
Patellofemoral anatomy
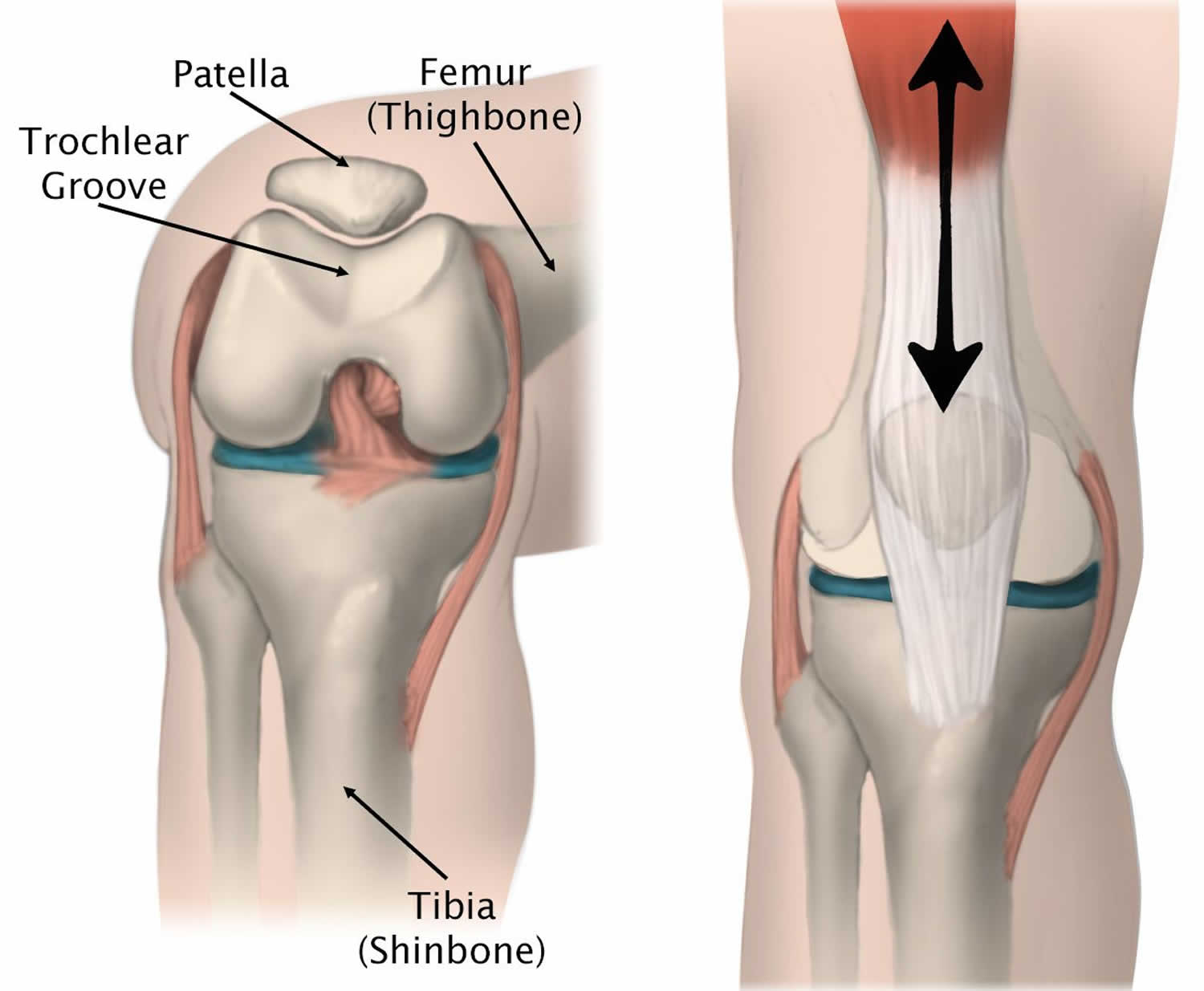
The patella is a small bone located in front of your knee joint — where the thighbone (femur) and shinbone (tibia) meet. It protects your knee and connects the muscles in the front of your thigh to your tibia.
The patella rests in a groove on top of the femur called the trochlear groove. When you bend and straighten your knee, the patella moves back and forth inside this groove.
A slippery substance called articular cartilage covers the ends of the femur, trochlear groove, and the underside of the patella. Articular cartilage helps your bones glide smoothly against each other as you move your leg.
Figure 1. Patellofemoral anatomy
Footnote: (Left) The patella rests in a small groove at the end of the femur called the trochlear groove. (Right) As you bend and straighten your knee, the patella slides up and down within the groove.
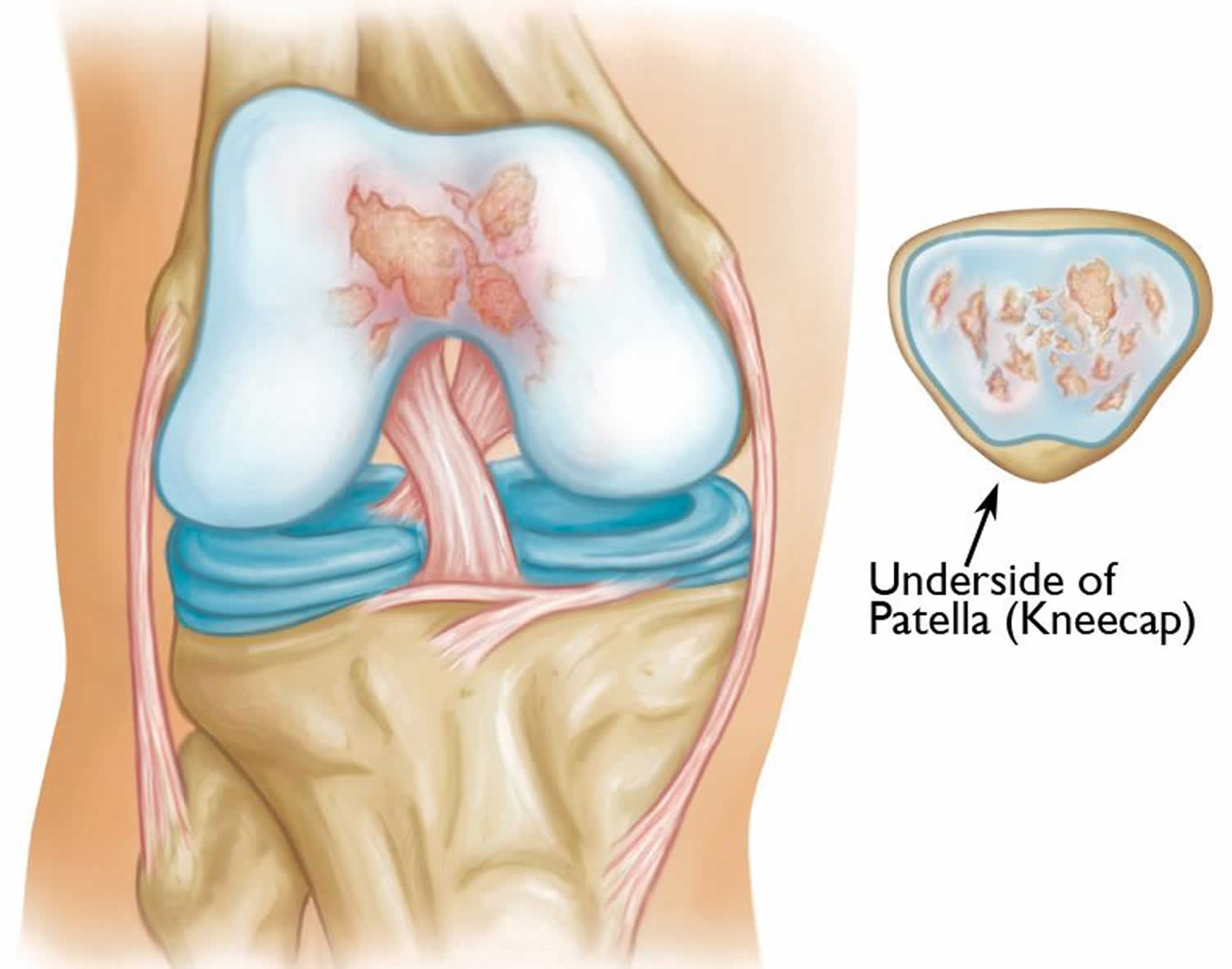
Figure 2. Patellofemoral arthritis
Footnote: Illustration shows patellofemoral arthritis. The patella (kneecap) has been removed to show damage to the cartilage on the underside.
Patellofemoral arthritis causes
Patellofemoral arthritis is a broad term refers to the presence of degenerative changes to the patellofemoral joint or osteochondral degeneration of the patellofemoral joint space. The arthritis is typically a combination of degenerative changes in the articular cartilage of the patella, termed chondromalacia, as well as abnormal biomechanical tracking of the patella within the trochlear groove which is most often in the lateral patellar facet. Patellofemoral arthritis may be unicompartmental or associated with femorotibial arthritis in either the medial or lateral compartments, or both.
Patients with patellofemoral arthritis frequently have a history of instability, including dislocation or subluxation, laxity, malalignment which usually manifests as lateralization, muscle imbalance, or high riding patella which is known as “patella alta.” Anterior cruciate ligament (ACL) reconstruction with either hamstring or patella tendon graft is another risk factor for developing patellofemoral arthritis.
Other causes of patellofemoral arthritis:
- Dysplasia occurs when the patella does not fit properly in the trochlear groove of the femur. Because of this, when the knee moves, there are increased stresses on the cartilage. This begins to wear the cartilage down.
- Patellar (kneecap) fractures often damage the articular cartilage that covers and protects the underside of the bone. Even though the broken bone heals, the joint surface may no longer be smooth. There is friction when the patella moves against the joint surface of the femur. Over time, this can lead to arthritis.
Risk factors for the development of patellofemoral arthritis include age, obesity, history of interarticular or patellar fracture, prior dislocation or subluxation, overuse from sport including high-intensity running or weight training, and history of arthritis in other joints. Systemic inflammatory disorders such as rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, juvenile idiopathic arthritis, and systemic lupus erythematosus are among other risk factors 4.
Patellofemoral arthritis symptoms
The main symptom of patellofemoral arthritis is anterior knee pain. Because the patellofemoral joint is in front of the knee, you may have pain in this area. The pain can be present at rest or with no activity at all. Most of the time, however, it is brought on by activities that put pressure on the kneecap, such as kneeling, squatting, climbing and descending stairs, and getting up from a low chair. Essentially, any activity that increases flexion of the knee increases the force load on the patellofemoral joint and causes pain. Patients may report popping, cracking, and grinding symptoms. They may report a history of stiffness or pseudo-locking due to the friction of the patella in the trochlear groove and a sensation of instability or “giving way.” It is also important to clarify if the patient has had any subluxation or dislocation events 5.
In addition, you may experience a crackling sensation called crepitus when you move your knee. Crepitus is sometimes painful and can be loud enough for other people to hear. When the disease is advanced, your kneecap may get stuck or “catch” when you straighten your knee.
Patellofemoral arthritis complications
In patients managed conservatively, complications are limited to persistent pain and instability and progression of the disease. Complications of surgical management include infection, quadriceps weakness, loss of normal function, and persistent pain despite the procedure. Patients may develop femorotibial osteoarthritis requiring total knee arthroplasty.
Patellofemoral arthritis diagnosis
Radiography is the principal study used in the diagnosis of patellofemoral arthritis. Computed tomography can also be used to determine patellar tilt and articular damage. Arthroscopy can be used for both diagnosis and therapy.
No laboratory tests are usually required for the initial workup for knee pain. However, if clinical suspicion arises, a workup for systemic causes of polyarticular arthritis may be appropriate. This workup includes but is not limited to an evaluation for Lyme disease, rheumatoid arthritis, psoriatic arthritis, and gout.
Clinical examination
A gait exam should be performed assessing for foot pronation, valgus or varus knees, and rotational malalignment of the tibia or femur. Gait exam findings associated with patellofemoral osteoarthritis include increased anterior pelvic tilt through the stance phase, increased lateral pelvic tilt on the contralateral side, increased hip adduction and lower hip extension during stance. Your doctor may measure the Q angle. Your doctor may observe an effusion, quadriceps, or hamstrings atrophy. The patella may be “squinting” or tilted inward, or alternatively, “frog eyed” and tilting outward. Patella tracking and mobility during passive flexion and extension should be observed.
Palpation during passive flexion-extension of the joint may reveal crepitus and is the exam finding most suggestive of patellofemoral arthritis. In patellofemoral arthritis, there can be tenderness around the medial or lateral patellar facet, or on the medial or lateral femoral condyles. The patellar grind test, also known as the Clarke test, is performed with the patient supine with the knee in full extension. The provider places their hand on the proximal patella and asks the patient to slowly contract their quadriceps muscle while resisting proximal movement of the patella. A positive test is a pain at the patellofemoral joint. The examiner may also passively move the patella in a superior-inferior or medial-lateral direction while applying posteriorly directed pressure. The patellar apprehension test involves placing a laterally directed force over the patella with the knee in full extension and at 90 degrees of extension. A positive test is a pain or quadriceps recruitment to avoid pain. This test primarily looks for patellar laxity or mobility but can also be suggestive of patellofemoral arthritis.
Imaging studies
Standard radiographs are typically sufficient to evaluate the patellofemoral joint. AP, lateral, and axial views are routinely obtained. These can be used to evaluate for joint space narrowing, subchondral sclerosis, osteophytes, articular degeneration, and patellar alignment. The lateral view can evaluate the alignment of the patella (alta, normal, or baja), femoral condylar dysplasia, and arthritis. The axial view, also termed “merchant” or “sunrise” view, can evaluate for patellar malalignment, trochlear groove depth, and arthritis. Both lateral and axial views can evaluate the patellofemoral joint space to assess the degree of arthritis. The Rosenberg or AP view is best used to evaluate the femorotibial compartments. Radiographic evidence of patellofemoral arthritis is as high as 34% in women and 19% in men over the age of 55.
Radiographs can be used to quantify changes in the patella in cases of suspected patellofemoral arthritis. The sulcus angle is typically about 138 degrees. The congruence angle is used to measure lateral patellar displacement and is normally negative 6 degrees. The Insall-Salvati ratio, which is used to assess for patella alta, is the ratio of the length of the patella ligament to patella bone measured on the lateral view. The patellofemoral index ratio compares the distance between the medial and lateral articular spaces.
If the diagnosis is in doubt, CT can better assess the patellofemoral joint although this is unnecessary in most patients with known or suspected arthritis. CT may be utilized to help identify lateral patellar subluxation or femoral trochlear dysplasia. In the setting of trauma where patella osteochondritis dissecans or other ligamentous injury is suspected, MRI is the imaging study of choice. Ultrasound may have a role in diagnosing patellofemoral arthritis when radiographs are unavailable; although the inability to see the articular side of the patella limits diagnostic utility. Arthroscopy can also be used for diagnosis and therapy.
Inflammatory causes of patellofemoral arthritis should be considered in the right clinical context. Serology for Lyme disease, rheumatoid arthritis, gonococcal arthritis, etc. should be considered when appropriate.
Patellofemoral arthritis staging
Radiographically, patellofemoral arthritis is classified into four stages based on the merchant view:
- Mild – more than 3 mm of joint space
- Moderate – less than 3 mm of joint space but no bony contact
- Severe – bony surfaces in contact over less than one-quarter of the joint surface
- Very severe – bony contact throughout the entire joint surface
Patellofemoral arthritis treatment
Treatment of patellofemoral arthritis has been challenging to clinicians. This is partly due to its variety of causes as well as growing but an inadequate understanding of cartilage regeneration. In most cases, management is non-operative, and conservative treatment is indicated.
Nonsurgical treatment
Treatment of patellofemoral arthritis is similar to the treatment of knee arthritis in general. Most cases can be treated without surgery. Nonsurgical options include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Drugs like aspirin, naproxen, and ibuprofen reduce both pain and swelling.
- Glucosamine and chondroitin sulfate may reduce or decrease the degree of knee pain. Intra-articular injections can also reduce pain symptoms.
- Kinesio-taping of the patella is well supported in the literature and can provide relief. This is aimed at preventing lateralization of the patella and is termed McConnell taping. A simple knee sleeve with compression may provide relief. Patella stabilizing braces and hinged braces can also play a role in treating patellofemoral osteoarthritis although not all patients will gain relief.
- Exercise. Regular exercise can decrease stiffness and strengthen the muscles that support your knee. Patients who have patellofemoral arthritis should try to avoid activities that put stress on the front of the knee, such as squatting. If you regularly do high-impact exercise, switching to low-impact activities will put less stress on your knee. Walking and swimming are good low-impact options.
- Activity modification. Activity modification may be helpful, including decreasing the frequency of squats, lunges, jumps, and other activities with prolonged flexion and increasing other activities that place less stress on the anterior knee.
- Weight loss. If you are overweight, losing just a few pounds can make a big difference in the amount of stress you place on your knee. Losing weight can also make it easier to move and maintain independence.
- Physical therapy. Physical therapy is a mainstay for treatment and can alleviate patellofemoral pain by strengthening the quadriceps femoris complex, most often the vastus medialis, as well as stretching the lateral patellar retinaculum. This can help with maltracking and range of motion of the joint. In patients with patellofemoral pain syndrome, which includes patellofemoral arthritis, 67% reported resolution of symptoms within 6 months of initiating physical therapy, and 80% graded their knee as excellent after 7 years. Specific exercises can improve range-of-motion in your knee. Exercises to strengthen the quadriceps muscles will help relieve pressure on the kneecap when you straighten your leg. If an exercise causes pain, stop the exercise and talk to your doctor or physical therapist.
- Cortisone (steroid) injections. Cortisone is a powerful anti-inflammatory medicine that can be injected directly into your knee. Corticosteroid injections are generally first-line therapy with the most robust evidence supporting their use.
- Viscosupplementation. In this procedure, a substance is injected into the joint to improve the quality of the joint fluid. The effectiveness of viscosupplementation in treating arthritis is unclear and continues to be studied by researchers.
- Platelet-rich plasma and other regenerative medicine modalities may have a role in treating patellofemoral osteoarthritis although the evidence is mixed with these options as well and more research is generally required.
Surgical treatment
Surgery is an option when nonsurgical treatment has failed. Several types of surgical procedures are available.
- Chondroplasty. Arthroscopy with debridement of the patellar cartilage is controversial. Chondroplasty procedure is done with arthroscopy — inserting thin surgical instruments into small incisions around your knee. During a chondroplasty, your surgeon trims and smooths roughened arthritic joint surfaces. Chondroplasty is an option in cases of mild to moderate cartilage wear.
- Soft tissue realignment. Soft tissue realignment of the extensor mechanism is generally directed at decreasing lateralization of the patella in the trochlear groove. This procedure varies at the discretion of the surgeon and patient and includes the release of the lateral patellar retinaculum, reattachment or reconstruction of the medial patellofemoral ligament, or advancement of the vastus medialis obliquus. The soft tissues on either side of the kneecap are tightened or released to change the position of the kneecap in the trochlear groove.
- Cartilage grafting. Normal healthy cartilage tissue may be taken from another part of the knee or from a tissue bank to fill a hole in the articular cartilage. This procedure is typically considered only for younger patients who have small areas of cartilage damage.
- Tibial tuberosity transfer. This procedure can help relieve pain in patients with arthritis in specific portions of the patella. In the appropriate patient, this procedure can reduce the pain of patellofemoral arthritis, particularly in young patients. The patellar tendon below the kneecap attaches to a bump on the front of the knee called the tibial tuberosity. Shifting the bump in any direction will change the position of the kneecap. After the procedure, the patella should move more smoothly in the trochlear groove, reducing pressure on the arthritic areas and relieving pain.
- Patellofemoral replacement (patelloplasty). During this “partial” knee replacement, damaged bone and cartilage surfaces are removed and replaced with metal and polyethylene (plastic) components. A thin metal shield is used to resurface the trochlear groove at the end of the femur. A plastic “button” or cover is used to resurface the backside of the patella. These components are typically held to the bone with cement.
- Patellofemoral replacement surgery cannot be carried out if there is arthritis involving other parts of the knee. If this is the case, your doctor may recommend a total knee replacement.
- Total knee replacement. In a total knee replacement, all the cartilage surfaces of the knee are resurfaced. The end of the femur and the top of the tibia are capped with a metal prosthesis. A plastic spacer is placed in between these components to create a smooth gliding surface. Additionally, the patella itself is usually resurfaced with a plastic “button.”
Postoperative and rehabilitation care
In general, rehabilitation of patellofemoral arthritis, whether operative or nonoperative, is directed at strengthening the quadriceps muscle, specifically the vastus medialis oblique, hip muscles, and core. The goals are to decrease the Q angle, lateralize the patella, and improve racking in the trochlear groove. If surgery is performed, the surgeon will have protocols specific to their procedure.
Patellofemoral arthritis prognosis
The prognosis of patients who develop patellofemoral arthritis is variable. For most patients, treatment for patellofemoral arthritis is successful in relieving pain and improving function. However, outcomes vary depending on patient-specific factors and the type of treatment. Your doctor will talk with you about the expected outcome of treatment in your specific situation.
Generally speaking, it is a progressive disease that requires more aggressive intervention as the degenerative changes worsen. In younger or otherwise healthy patients, conservative management may reduce their symptoms to a point where it does not affect their activities of daily living. In other patients who have more progressed disease state, involvement of the femorotibial joint, obesity, or other chronic medical conditions, they will generally require more aggressive management.
References- Kiel J, Kaiser K. Patellofemoral Arthritis. [Updated 2019 Jan 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513242
- Woon CYL, Christ AB, Goto R, Shanaghan K, Shubin Stein BE, Gonzalez Della Valle A. Return to the operating room after patellofemoral arthroplasty versus total knee arthroplasty for isolated patellofemoral arthritis-a systematic review. Int Orthop. 2019 Jan 07
- Lim JW, Chen JY, Chong HC, Pang HN, Tay DKJ, Chia SL, Lo NN, Yeo SJ. Pre-existing patellofemoral disease does not affect 10-year survivorship in fixed bearing unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018 Oct 04
- Agarwala S, Shetty V, Karumuri LK, Vijayvargiya M. Patellar Resurfacing versus Nonresurfacing with Patellaplasty in Total Knee Arthroplasty. Indian J Orthop. 2018 Jul-Aug;52(4):393-398.
- Coburn SL, Barton CJ, Filbay SR, Hart HF, Rathleff MS, Crossley KM. Quality of life in individuals with patellofemoral pain: A systematic review including meta-analysis. Phys Ther Sport. 2018 Sep;33:96-108.