Pregnancy hemorrhoids
Hemorrhoids also called piles, are a normal part of your anatomy. You have both internal and external hemorrhoids, located inside the anal canal and around the anal opening, respectively. The internal hemorrhoids are a part of the blood supply to the anus and are made up of small arterial branches. External hemorrhoids are veins. You are not aware of your hemorrhoids when they are in their normal state. Hemorrhoids cause no symptoms. Pregnancy predisposes women to symptomatic hemorrhoids that usually resolve after delivery. During pregnancy, hemorrhoids are caused by increased blood flow in the pelvic area and the pressure on veins there from your growing uterus. Constipation can make your hemorrhoids worse. Constipation is when you don’t have bowel movements or they don’t happen often, or your stools (poop) are hard to pass. Adding fiber and fluids to your diet can help prevent constipation and hemorrhoids.
If you have a hemorrhoid, you may feel a tender lump on the edge of your anus. You may also see blood on the toilet paper or in the toilet after a bowel movement. Hemorrhoids may also be itchy and painful.
The symptoms of hemorrhoids can be relieved with ice packs to reduce swelling. Sitting in a bath of warm water may relieve symptoms. You also may use a hemorrhoid cream or suppositories.
Surgical intervention is contraindicated because of the risk of inducing labor 1. Conservative treatment is recommended, with excision of thrombosed external hemorrhoids if necessary.
Hemorrhoids are very common in both men and women. Nearly half of Americans have hemorrhoids by age 50 2. If you have bleeding or severe pain, see your doctor right away.
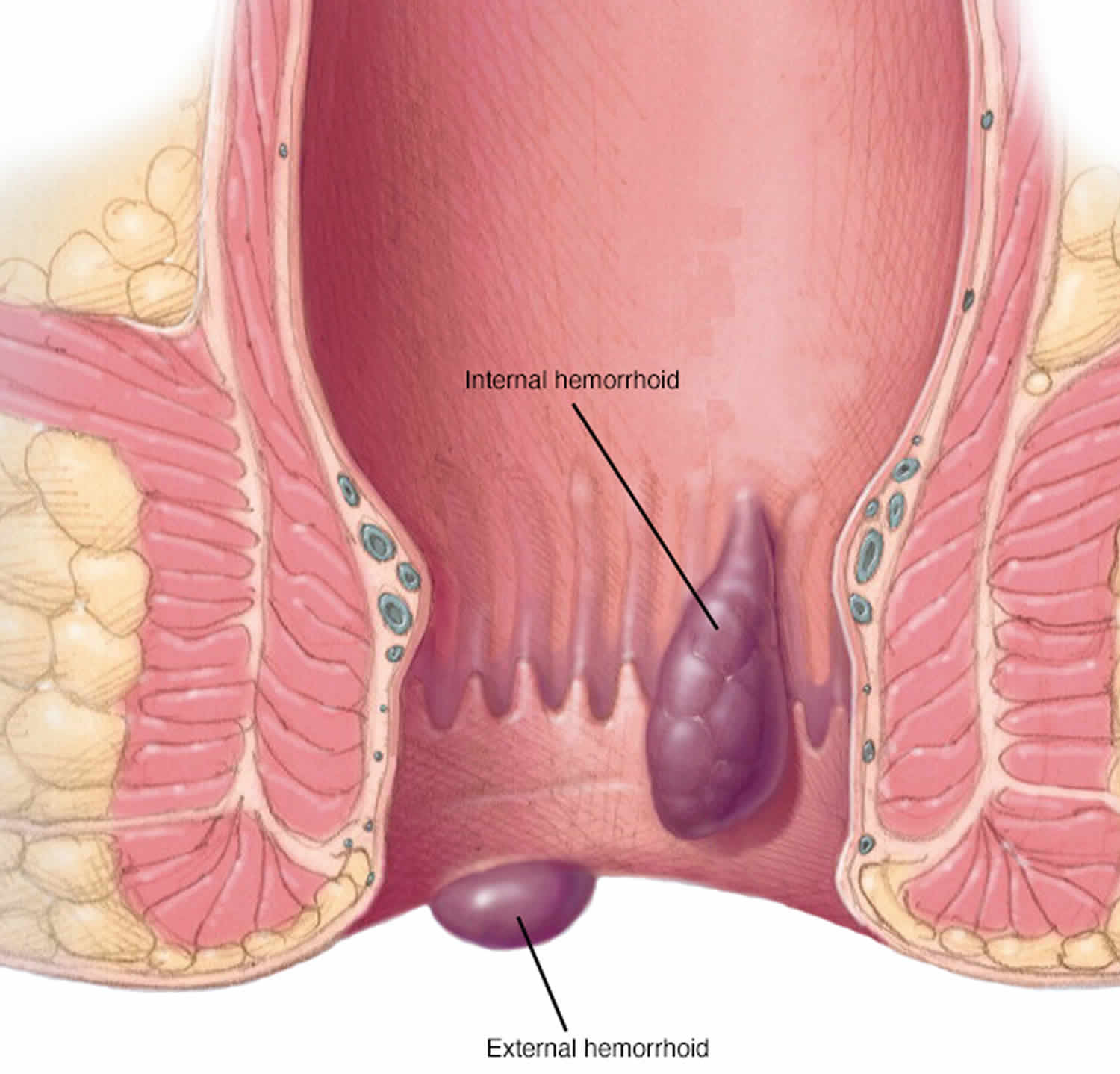
Figure 1. Pregnancy hemorrhoids
Bleeding during bowel movements is the most common sign of hemorrhoids. Your doctor can do a physical examination and perform other tests to confirm hemorrhoids and rule out more-serious conditions or diseases.
Also talk to your doctor if you know you have hemorrhoids and they cause pain, bleed frequently or excessively, or don’t improve with home remedies.
- Don’t assume rectal bleeding is due to hemorrhoids, especially if you are over 40 years old.
- Rectal bleeding can occur with other diseases, including colorectal cancer and anal cancer.
- If you have bleeding along with a marked change in bowel habits or if your stools change in color or consistency, consult your doctor.
- These types of stools can signal more extensive bleeding elsewhere in your digestive tract.
Seek emergency care if you experience large amounts of rectal bleeding, lightheadedness, dizziness or faintness.
Types of hemorrhoids
The type of hemorrhoid you have depends on where it occurs.
- Internal hemorrhoids involve the veins inside your rectum. Internal hemorrhoids usually don’t hurt but they may bleed painlessly.
- Prolapsed hemorrhoids may stretch down until they bulge outside your anus. A prolapsed hemorrhoid may go back inside your rectum on its own, or you can gently push it back inside.
- External hemorrhoids involve the veins outside the anus. They can be itchy or painful and can sometimes crack and bleed.
Internal hemorrhoids
Painless rectal bleeding or prolapse of anal tissue is often associated with symptomatic internal hemorrhoids. Prolapse is hemorrhoidal tissue coming from the inside that can often be felt on the outside of the anus when wiping or having a bowel movement. This tissue often goes back inside spontaneously or can be pushed back internally by the patient. The symptoms tend to progress slowly over a long time and are often intermittent.
Internal hemorrhoids are classified by their degree of prolapse 3, which helps determine management:
- Grade One: No prolapse
- Grade Two: Prolapse that goes back in on its own
- Grade Three: Prolapse that must be pushed back in by the patient
- Grade Four: Prolapse that cannot be pushed back in by the patient (often very painful)
Bleeding attributed to internal hemorrhoids is usually bright red and can be quite brisk. It may be found on the wipe, dripping into the toilet bowl, or streaked on the bowel movement itself. Not all people with symptomatic internal hemorrhoids will have significant bleeding. Instead, prolapse may be the main or only symptom. Prolapsing tissue may result in significant irritation and itching around the anus. People with internal hemorrhoids may also complain of mucus discharge, difficulty with cleaning themselves after a bowel movement or a sense that their stool is “stuck” at the anus with bowel movements. People without significant symptoms from internal hemorrhoids do not require treatment based on their appearance alone.
Most patients with grade 1 or 2 hemorrhoids, and many with grade 3 hemorrhoids, can be treated in primary care offices. Patients in whom office-based treatment is ineffective (see below under Treatment) and those with mixed hemorrhoids may require treatment in surgical suites with facilities for anesthesia. The most common surgical treatments are ligation or tissue destruction, fixation techniques (i.e., hemorrhoidopexy – hemorrhoid stapling), and excision (i.e., hemorrhoidectomy).
External hemorrhoids
Symptomatic external hemorrhoids often present as a bluish-colored painful lump just outside the anus and they tend to occur spontaneously and may have been preceded by an unusual amount of straining. The skin overlying the outside of the anus is usually firmly attached to the underlying tissues. If a blood clot or thrombosis develops in this tightly held area, the pressure goes up rapidly in these tissues often causing pain. The pain is usually constant and can be severe. Occasionally the elevated pressure in the thrombosed external hemorrhoid results in breakdown of the overlying skin and the clotted blood begins leaking out. Patients may also complain of intermittent swelling, pressure and discomfort, related to external hemorrhoids which are not thrombosed.
Thrombosed external hemorrhoids
Thrombosed external hemorrhoids cause acute, severe pain. Without intervention, the pain typically improves over two to three days, with continued improvement as the thrombus gradually absorbs over several weeks. Analgesics and stool softeners may be beneficial. Topical therapy with nifedipine and lidocaine cream is more effective for pain relief than lidocaine (Xylocaine) alone 4.
In patients with severe pain from thrombosed hemorrhoids, excision or incision and evacuation of the thrombus within 72 hours of symptom onset provide more rapid pain relief than conservative treatment 5. Both procedures can be performed under local anesthesia, and the resulting wound can be left open or sutured 6.
Pregnancy hemorrhoids causes
Hemorrhoids are caused by increased pressure in the veins of your anus or rectum. One of the main causes is straining when you’re trying to have a bowel movement. This may happen if you’re constipated or if you have diarrhea. It may also happen if you sit on the toilet too long. Hemorrhoids can also be caused by obesity, heavy lifting or any other activity that caused you to strain.
The veins around your anus tend to stretch under pressure and may bulge or swell. Swollen veins (hemorrhoids) can develop from increased pressure in the lower rectum due to:
- Straining during bowel movements or heavy lifting or vigorous activity.
- Pregnancy and vaginal deliveries. Straining during physical labor
- Hard or watery bowel movements.
- Sitting on the toilet for a long time (for example, while reading or playing video games).
- A low-fiber diet.
- Aging.
- Being overweight or obesity
- Constipation
- Anal intercourse
Pregnancy hemorrhoids prevention
Here’s what you can do to help prevent hemorrhoids during pregnancy:
- Eat high-fiber foods. Eat more fruits, vegetables and whole grains. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can cause hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
- Drink plenty of water. Drink six to eight glasses of water and other liquids (not alcohol) each day to help keep stools soft.
- Consider fiber supplements. Most people don’t get enough of the recommended amount of fiber — 25 grams a day for women and 38 grams a day for men — in their diet. Studies have shown that over-the-counter fiber supplements, such as Metamucil and Citrucel, improve overall symptoms and bleeding from hemorrhoids. These products help keep stools soft and regular. If you use fiber supplements, be sure to drink at least eight glasses of water or other fluids every day. Otherwise, the supplements can cause constipation or make constipation worse.
- Do something active every day. Talk to your doctor about activities that are safe during pregnancy.
- Gain the right amount of weight during pregnancy. Talk to your doctor about how much you should gain.
- Don’t strain. Straining and holding your breath when trying to pass a stool creates greater pressure in the veins in the lower rectum.
- Go as soon as you feel the urge. If you wait to pass a bowel movement and the urge goes away, your stool could become dry and be harder to pass.
- Exercise. Stay active to help prevent constipation and to reduce pressure on veins, which can occur with long periods of standing or sitting. Exercise can also help you lose excess weight that may be contributing to your hemorrhoids.
- Avoid long periods of sitting. Sitting too long, particularly on the toilet, can increase the pressure on the veins in the anus.
Pregnancy hemorrhoids symptoms
Signs and symptoms of hemorrhoids may include:
- Painless bleeding during bowel movements — you might notice small amounts of bright red blood on your toilet tissue or in the toilet
- Itching or irritation in your anal region
- Pain or discomfort
- Swelling around your anus
- A lump near your anus, which may be sensitive or painful (may be a thrombosed hemorrhoid)
Hemorrhoid symptoms usually depend on the location.
Internal hemorrhoids. These lie inside the rectum. You usually can’t see or feel these hemorrhoids, and they rarely cause discomfort. But straining or irritation when passing stool can damage a hemorrhoid’s surface and cause it to bleed. When they cause symptoms, the most common are painless rectal bleeding, which usually is seen as bright red blood on the toilet paper or in the toilet bowl. It is important to know that just a few drops of blood in toilet water can change the color of the water dramatically.
Occasionally, straining can push an internal hemorrhoid through the anal opening. This is known as a protruding or prolapsed hemorrhoid and can cause pain and irritation.
External hemorrhoids. These are under the skin around your anus and cause no symptoms. When they cause symptoms, the most common are pain, itching, pressure and bleeding; they can often be felt as a bulge in the skin near the anal opening.
Thrombosed hemorrhoids. Sometimes blood may pool in an external hemorrhoid and form a clot (thrombus) that can result in severe pain, swelling, inflammation and a hard lump near your anus.
Pregnancy hemorrhoids complications
Complications of hemorrhoids are very rare but include:
- Anemia. Rarely, chronic blood loss from hemorrhoids may cause anemia, in which you don’t have enough healthy red blood cells to carry oxygen to your cells.
- Strangulated hemorrhoid. If the blood supply to an internal hemorrhoid is cut off, the hemorrhoid may be “strangulated,” another cause of extreme pain.
Pregnancy hemorrhoids diagnosis
Your doctor may be able to see if you have external hemorrhoids simply by looking. Tests and procedures to diagnose internal hemorrhoids may include examination of your anal canal and rectum:
- Digital examination. During a digital rectal exam, your doctor inserts a gloved, lubricated finger into your rectum. He or she feels for anything unusual, such as growths. The exam can suggest to your doctor whether further testing is needed.
- Visual inspection. Because internal hemorrhoids are often too soft to be felt during a rectal exam, your doctor may also examine the lower portion of your colon and rectum with an anoscope, proctoscope or sigmoidoscope.
Your doctor may want to examine your entire colon using colonoscopy if:
- Your signs and symptoms suggest you might have another digestive system disease
- You have risk factors for colorectal cancer
- You’re middle-aged and haven’t had a recent colonoscopy.
The American Society of Colon and Rectal Surgeons recommends taking the patient history and performing a physical examination with anoscopy and further endoscopic evaluation if there is concern for inflammatory bowel disease or cancer 7. A complete evaluation of the colon is warranted in the following groups 7:
- Patients who are 50 years or older and have not had a complete examination of the colon within the past 10 years
- Patients who are 40 years or older and have not had a complete examination of the colon within the past 10 years, and who have one first-degree relative in whom colorectal cancer or adenoma was diagnosed at age 60 years or younger
- Patients who are 40 years or older and have not had a complete examination of the colon within the past five years, and who have more than one first-degree relative in whom colorectal cancer or adenoma was diagnosed at age 60 years or younger
- Patients with iron deficiency anemia
- Patients who have a positive fecal occult blood test.
Pregnancy hemorrhoids treatment
You can often relieve the mild pain, swelling and inflammation of hemorrhoids with home treatments. Often these are the only treatments needed.
Eat high-fiber foods. Eat more fruits, vegetables and whole grains – it is usually recommended you eat 20-35 grams of fiber per day. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can worsen symptoms from existing hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
Don’t sit for a long time. Get up and move around to help move the weight of your uterus off of the pelvic veins.
Use topical treatments. Apply an over-the-counter hemorrhoid cream or suppository containing hydrocortisone, or use pads containing witch hazel or a numbing agent.
Soak regularly in a warm bath or sitz bath. Soak your anal area in plain warm water 10 to 15 minutes two to three times a day. Make sure the water’s not hot. A sitz bath fits over the toilet.
Keep the anal area clean. Bathe (preferably) or shower daily to cleanse the skin around your anus gently with warm water. Avoid alcohol-based or perfumed wipes. Gently pat the area dry or use a hair dryer.
Don’t use dry toilet paper. To help keep the anal area clean after a bowel movement, use moist towelettes or wet toilet paper that doesn’t contain perfume or alcohol.
Apply cold patch or witch hazel pads. Apply ice packs or cold compresses on your anus to relieve swelling.
Take oral pain relievers. You can use acetaminophen (Tylenol, others), aspirin or ibuprofen (Advil, Motrin IB, others) temporarily to help relieve your discomfort.
Ask your doctor about over-the-counter medicine (creams or wipes) that are safe to use during pregnancy. Also ask about fiber supplements and stool (poop) softeners. Don’t take any medicine, supplement or herbal product without talking to your doctor first. Over-the-counter medicine is medicine you can buy without a prescription from your doctor. A supplement is a product you take to make up for certain nutrients that you don’t get enough of in the foods you eat. An herbal product, like a pill or tea, is made from herbs (plants) that are used in cooking.
With these treatments, hemorrhoid symptoms often go away within a week. See your doctor if you don’t get relief in a week, or sooner if you have severe pain or bleeding.
References- Hemorrhoids. Am Fam Physician. 2011 Jul 15;84(2):204-210. http://www.aafp.org/afp/2011/0715/p204.html
- Hemorrhoids and Other Anal Disorders. American College of Gastroenterology. http://patients.gi.org/topics/hemorrhoids-and-other-anal-disorders/
- Hemorrhoids. American Society of Colon and Rectal Surgeons. https://www.fascrs.org/patients/disease-condition/hemorrhoids-expanded-version
- Perrotti P, Antropoli C, Molino D, De Stefano G, Antropoli M. Conservative treatment of acute thrombosed external hemorrhoids with topical nifedipine. Dis Colon Rectum. 2001;44(3):405–409.
- Greenspon J, Williams SB, Young HA, Orkin BA. Thrombosed external hemorrhoids: outcome after conservative or surgical management. Dis Colon Rectum. 2004;47(9):1493–1498.
- Zuber TJ. Hemorrhoidectomy for thrombosed external hemorrhoids. Am Fam Physician. 2002;65(8):1629–1632.
- Cataldo P, Ellis CN, Gregorcyk S, et al.; Standards Practice Task Force, The American Society of Colon and Rectal Surgeons, USA. Practice parameters for the management of hemorrhoids (revised). Dis Colon Rectum. 2005;48(2):189–194.