Pyogenic granuloma
Pyogenic granuloma also known as lobular capillary hemangioma or granuloma pyogenicum, is a common, benign (harmless) growth that often appears as a rapidly growing, bleeding bump on the skin or inside the mouth 1. Pyogenic granuloma is composed of blood vessels and may occur at the site of minor injury. Pyogenic granulomas have also been associated with medications including oral contraceptives and retinoids. Histologically, pyogenic granulomas are composed of capillaries (small blood vessels) and venules (smallest veins) with plump endothelial cells separated into lobules by fibromyxoid stroma 2. Pyogenic granuloma carries no risk of cancer, is not contagious (cannot be spread to another person) and is not due to an infection.
Pyogenic granulomas can present at any age—including at birth (congenitally), during the neonatal period, during infancy, or during pregnancy—although they are most common in older children and young adults. When a pyogenic granuloma occurs in a pregnant woman, it is sometimes called a “pregnancy tumor” (granuloma gravidarum). Pyogenic granulomas develop in up to 5% of pregnant women.
Pyogenic granulomas occur in people of all races. Women are more frequently affected by pyogenic granulomas than men, though male and female children are equally affected.
Pyogenic granulomas are most often seen in:
- Children and young adults
- Pregnant women
- Women taking oral contraceptives
- People taking certain oral retinoid medications, including isotretinoin or acitretin (Soriatane®)
- People taking protease inhibitors such as indinavir (Crixivan®)
- People on chemotherapy
See your doctor if you notice any rapidly enlarging skin growth in order to establish a correct diagnosis! Because it is prone to easy bleeding, a pyogenic granuloma lesion should be covered with a bandage until you see your doctor.
Pyogenic granulomas occur as solitary growths, but multiple (grouped) or rarely disseminated lesions have been described 3. Pyogenic granulomas appear as small or large, smooth or lobulated vascular nodules that can grow rapidly, sometimes over weeks to months and have a tendency to bleed profusely. Pyogenic granulomas are usually cutaneous, but deep-seated/subcutaneous pyogenic granulomas have been reported and mimic other vascular lesions 4. Some untreated lesions eventually atrophy, become fibromatous, and slowly regress. A retrospective review of a series of eight children with disseminated congenital or neonatal pyogenic granulomas reported the occurrence of hemorrhagic central nervous system lesions in seven patients, five of whom developed neurologic complications. Four of the eight patients had transient bleeding disorder 5.
Pyogenic granulomas that develop in pregnant women often resolve after delivery. Similarly, pyogenic granulomas associated with medications usually improve when the medicine is discontinued or the dosage is lowered. Depending on the size of the pyogenic granuloma and its location and symptoms, the doctor may decide that no treatment is necessary for pregnant women or for people who can safely stop or lower the dose of the medication that caused the lesion.
Although pyogenic granuloma is a benign condition, it is frequently removed due to its tendency to bleed, its tenderness, and its distressing appearance. However, untreated pyogenic granulomas may go away on their own.
- The main problem with pyogenic granulomas is the way that they ooze and bleed so easily after minor knocks. This can be of great nuisance, but they are usually not painful.
- People often worry that their rapid growth and bleeding mean that they are cancerous, even though they are not; however, you should always see your doctor if you have a rapidly growing skin lump.
In obvious cases of pyogenic granuloma, your physician may choose to treat it immediately after obtaining the biopsy. Such treatments include:
- Scraping and burning (curettage and cauterization). After numbing with local anesthetic, the area is scraped with a sharp instrument (a curette) and burned with an electric needle (cautery).
- Silver nitrate solution
- Topical imiquimod cream (Aldara®)
- Laser treatment
- Freezing with liquid nitrogen (cryotherapy)
- Surgical removal (excision)
Approximately 40% of pyogenic granulomas come back (recur) after treatment, especially those lesions located on the trunk of teenagers and young adults. Recurrent pyogenic granulomas are best treated by surgical excision.
A full-thickness excision is the treatment with the lowest recurrence rate (around 3%) 6, but curettage, laser photocoagulation, or cryotherapy can also be used 7. Topical timolol and propranolol have also been used.
Make an appointment with a dermatologist or another physician if any rapidly enlarging or bleeding growth develops on your skin or in the areas lining your nose or mouth (mucous membranes).
You should always go straight to your doctor if you have any marks on your skin that are growing in size, change in color or bleeds.
Are pyogenic granulomas inherited?
No. There doesn’t appear to be an increased risk in other family members.
Can a pyogenic granuloma be cured?
Yes, by removing it or treating it with a cream (see treatment below).
What do pyogenic granulomas look like?
As pyogenic granulomas are made up of small blood vessels, they are bright red; later they may turn a darker shade. Their surface is shiny and moist but may become crusty after they have bled.
Pyogenic granulomas stick out from the surface of the skin as a painless red fleshy nodule. Pyogenic granulomas are seldom more than 1 cm across, typically 5-10 mm in diameter. Some have a bumpy surface and look rather like a raspberry, while others are narrower where they come out from the skin and look as if they are on a stalk.
Pyogenic granuloma is usually solitary, but multiple nodules and satellite lesions can erupt. The most common sites involved are the fingers and face. Pyogenic granuloma easily bleeds with minor trauma.
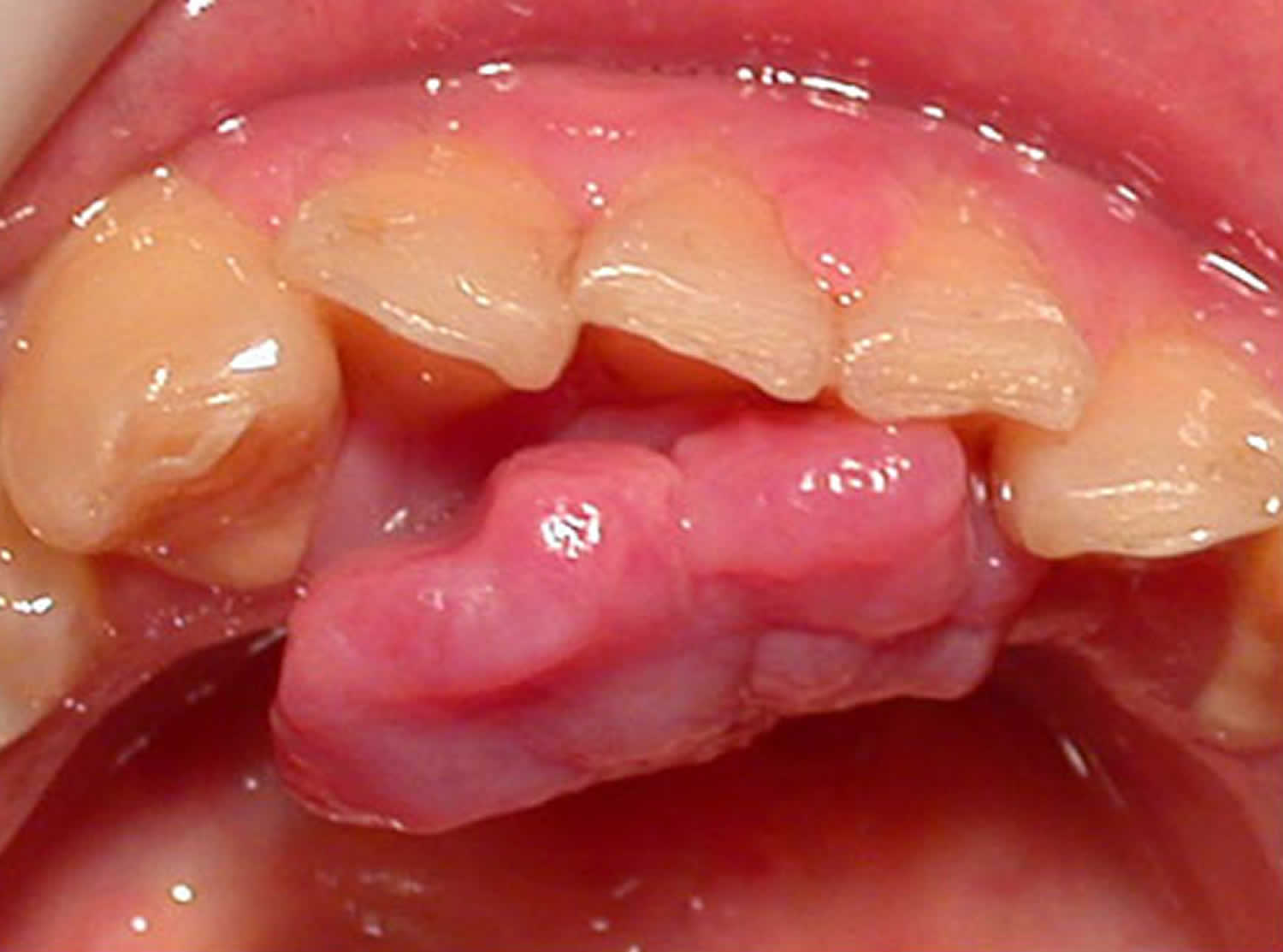
Oral mucosal pyogenic granulomas typically develop on the lip and gums (gingiva) as pedunculated or sessile slow-growing painless red papules ranging in size from a few millimetres to several centimetres. The surface can be ulcerated with a yellow-fibrinous surface, and easy bleeding. With time, the lesion becomes a paler pink color. Other mucosal sites that can be affected include the conjunctiva and nasal mucosa.
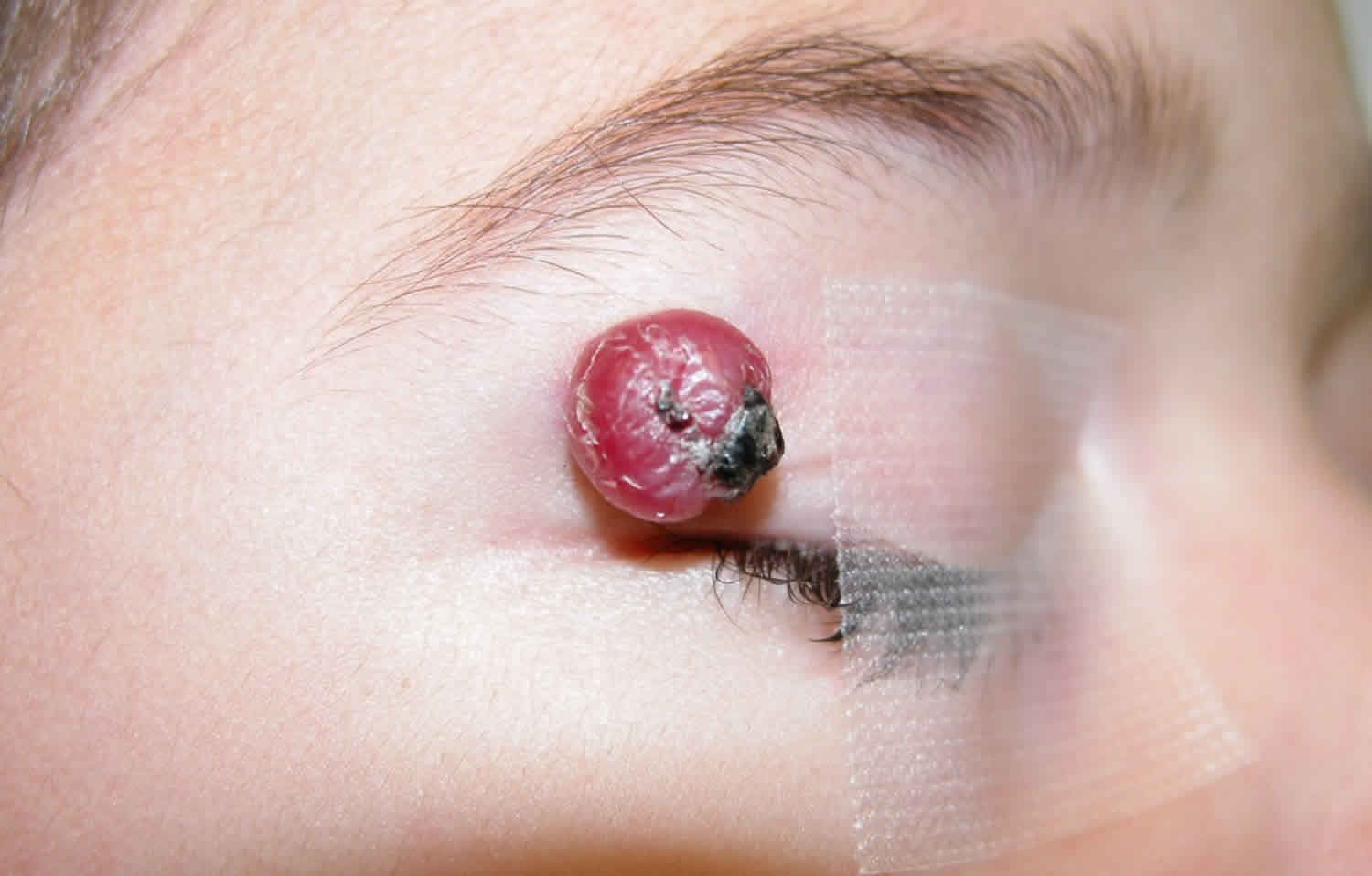
Figure 1. Pyogenic granuloma nose
Figure 2. Pyogenic granuloma mouth
Figure 3. Pyogenic granuloma gums
Figure 4. Pyogenic granuloma lip
Figure 5. Pyogenic granuloma eye
Footnote: A 30-year-old man presented with a pedunculated lesion on his right lower eyelid that had grown over a period of 3 days. Two weeks before presentation, a cyst had ruptured on the same eyelid. The new lesion started as a small lump on the bulbar conjunctiva and progressively increased in size until it protruded from the eyelid. The patient’s clinical course and a physical examination were suggestive of a pyogenic granuloma, a benign vascular lesion characterized by inflammatory cells and lobular capillary proliferation. Conjunctival pyogenic granulomas grow rapidly in the days to weeks after a conjunctival injury from surgery or trauma and can develop on the conjunctiva or external surfaces of the eyelids. The differential diagnosis includes suture granulomas, squamous papillomas, and malignant tumors, such as squamous-cell carcinoma and amelanotic melanoma. Pyogenic granulomas are often friable and prone to bleeding and can be treated with topical glucocorticoids or surgical excision. In this case, an intralesional injection of triamcinolone was administered at the time of excision to reduce the risk of recurrence. A histopathological assessment confirmed the diagnosis. On review, 3 months after excision, there was minimal scarring of the conjunctival surface and no evidence of recurrence.
[Source 8 ]Figure 6. Pyogenic granuloma finger
Pyogenic granuloma clinical findings
Distribution
- Pyogenic granuloma can arise on any part of the body but the most common sites are the fingers / hands, head and upper trunk.Morphology
- Pyogenic granuloma starts as a small red spot but quickly enlarges into a nodule
- Initially smooth, but often becomes eroded and bleeds significantly on contact
Pyogenic granuloma causes
The exact cause of sporadic pyogenic granulomas is unknown. Most pyogenic granulomas come up for no obvious reason, but some appear to follow minor damage to the skin, such as a cut that does not heal properly or a prick from a thorn. Pyogenic granulomas can also occur after starting certain medications, such as retinoids (which are sometimes used for the treatment of acne). Pyogenic granulomas often appear following an injury on the hands, arms, or face. Pyogenic granuloma may arise spontaneously within or following laser treatment or cryotherapy to a preexisting vascular malformation, such as capillary (port-wine stain)or arteriovenous malformation 9, 10, 11.
A study investigated ten patients with pyogenic granulomas arising from a capillary malformation and found eight with BRAF c.1799T>A mutations, one with an NRAS c.182A>G mutation, and one with a GNAQ c.548G>A mutation 12. This GNAQ mutation was also found in the underlying capillary malformation. In 25 patients with pyogenic granulomas and no capillary malformation, 3 patients had BRAF c.1799T>A mutations and 1 patient had a KRAS c.37G>C mutation. These genetic findings will help with future treatment modalities for this benign vascular tumor 12.
Pyogenic granulomas are common in children, young adults and pregnancy, but can arise at any age. Pyogenic granuloma is sudden in onset, grows rapidly and bleeds after minimal trauma.
Factors associated with the development of a pyogenic granuloma may include:
- Trauma — recent minor trauma accounts for 7% of presentations and, in the oral cavity, chronic minor irritation is thought to be a common trigger. Nasal piercings are reported in association with intranasal pyogenic granuloma.
- Hormonal influences — can occur with oral contraceptive use and in 5% of pregnancies.
- Medications — oral retinoids, protease inhibitors (used in the treatment of HIV/AIDS), targeted cancer therapies, and immunosuppression.
- Infection — Staphylococcus aureus is frequently detected. In the oral cavity, poor dental hygiene is a common association. There is no evidence for a viral origin.
Drugs implicated in pyogenic granulomas include:
- Systemic and topical retinoids
- Antiretrovirals: Indinavir (HIV protease inhibitor) 13
- Antineoplastics
- Pyrimidine analogs: capecitabine 14 and systemic 5-fluorouracil 15
- Taxanes: docetaxel 16 and paclitaxel 17
- Epidermal growth factor receptor (EGFR) inhibitors 18, 19:
- Monoclonal antibodies against the EGFR: cetuximab and panitumumab
- EGFR tyrosine kinase inhibitors (orally active small molecule): gefitinib, erlotinib, lapatinib, afatinib, and osimertinib
- Tyrosine kinase inhibitor (imatinib) 20
- BRAF inhibitors: vemurafenib, encorafenib 21, 22
- Immunosuppressive agents
Disseminated pyogenic granulomas, a rare entity, have been documented to occur with isotretinoin use in patients with severe nodulocystic acne and the use of granulocyte colony-stimulating factor (G-CSF) in immunodeficient patients 25, 26, 27, 28.
Intraoral pyogenic granulomas are seen in patients on cyclosporine and tacrolimus after a hematopoietic stem cell transplant 29, 30, 31, 32. Several case reports support this hypothesis, especially with patients treated for either acute or chronic graft versus host disease with cyclosporine or tacrolimus 29.
Pyogenic granuloma signs and symptoms
Typically, pyogenic granulomas appear as a beefy, red bump that enlarges rapidly over a few weeks. On average, pyogenic granulomas are about 5–10 mm in diameter. They may bleed easily and, in some cases, can be tender. Very rarely, more than one lesion of pyogenic granuloma may develop at the same time at the same site.
The most common locations for pyogenic granulomas include:
- Lips, gums, and inner mouth (particularly in pregnant women)
- Hands and fingers
- Head and neck
- Feet and toes
- Upper trunk
Pyogenic granuloma possible complications
These problems may occur:
- Pyogenic granuloma can bleed profusely and frequently with minor trauma, resulting in anemia.
- Secondary infections.
- Cosmetic disfigurement, which may be of psychological distress in some people, particularly when the lesion is on the face 33
- Oral pyogenic granuloma can rarely cause significant bone loss.
- Return of pyogenic granuloma after treatment.
Pyogenic granuloma differential diagnosis
The clinical differential diagnosis of cutaneous pyogenic granuloma includes:
- Amelanotic melanoma
- Kaposi sarcoma
- Bacillary angiomatosis.
Amelanotic or hypomelanotic melanoma is the most important differential diagnosis even on dermoscopy with many shared features.
The differential diagnosis of oral cavity pyogenic granuloma includes the above, as well as the site-specific peripheral giant cell granuloma and peripheral ossifying fibroma.
The differential diagnosis on histology includes cherry angioma and bacillary angiomatosis.
Pyogenic granuloma diagnosis
Your doctor will do a physical exam to diagnose pyogenic granuloma. You may also need a skin biopsy to confirm the diagnosis. Histology of pyogenic granuloma shows a prominent lobular capillary arrangement in the dermis. The overlying epidermis may be thinned or ulcerated, and the peripheral collarette is formed by elongated rete ridges and eccrine ducts. Inflammatory changes and signs of hemorrhage are secondary 34.
Although the diagnosis is often straightforward the main differential diagnosis is that of an amelanotic melanoma, which tend to bleed less than pyogenic granuloma. Other features that may increase the level of suspicion include no clear history of trauma and an atypical site or age group. To this end, lesions needing treatment are best removed surgically (deep curettage and cautery, or excision) and sent for histology.
Pyogenic granuloma treatment
If the diagnosis of pyogenic granuloma is suspected, your doctor will probably want to perform a skin biopsy. The procedure involves:
- Numbing the skin with an injectable anesthetic.
- Sampling a small piece of skin by using a flexible razor blade, a scalpel, or a tiny cookie cutter (called a “punch biopsy”). If a punch biopsy is taken, a stitch (suture) or two may be placed and will need to be removed 6–14 days later.
- Having the skin sample examined under the microscope by a specially trained physician (dermatopathologist).
Although pyogenic granuloma is a benign condition, it is frequently removed due to its tendency to bleed, its tenderness, and its distressing appearance. However, untreated pyogenic granulomas may go away on their own.
Small pyogenic granulomas may go away suddenly. Larger bumps are treated with:
- Surgical shaving or excision
- Scraping and burning (curettage and cauterization). After numbing with local anesthetic, the area is scraped with a sharp instrument (a curette) and burned with an electric needle (cautery).
- Freezing with liquid nitrogen (cryotherapy)
- Silver nitrate solution
- Topical imiquimod cream (Aldara®) (may not be as effective as surgery)
- Laser treatment
- Topical timolol and propranolol (beta blockers) have also been used.
Pyogenic granulomas that develop in pregnant women often resolve after delivery. Similarly, pyogenic granulomas associated with medications usually improve when the medicine is discontinued or the dosage is lowered. Depending on the size of the pyogenic granuloma and its location and symptoms, your doctor may decide that no treatment is necessary for pregnant women or for people who can safely stop or lower the dose of the medication that caused the lesion.
A few pyogenic granulomas lose their color and shrivel with time, but most are such a nuisance that they need to be treated before then. Freezing a pyogenic granuloma with liquid nitrogen can get rid of it but does not provide a specimen that can be checked in the laboratory. The usual treatment is to scrape pyogenic granulomas off with a sharp spoon-like instrument (a curette) after the area has been made numb by an injection of a local anaesthetic. The bleeding area left behind is then sealed with a hot point (cauterized).
A gel containing timolol or topical steroids have also been used successfully to treat pyogenic granulomas. Although the evidence for this is still limited. This maybe especially useful in children as it avoids more invasive procedures.
- In a single-arm series of patients with acquired ocular pyogenic granulomas, a small number of pediatric patients were treated for 21 days to 6 weeks with twice-daily topical timolol, 0.5% 35, 36. Complete or near-complete responses without subsequent recurrence or progression were noted in 75% to 100% of the patients (all ages).
- A study of 22 patients with skin pyogenic granulomas who were treated with topical 1% propranolol ointment with occlusion had the following results 37:
- Fifty-nine percent of patients achieved complete responses (mean, 66 days), 18% of patients had stable disease, and 22% of patients did not respond to the treatment.
In this study, only skin toxicity was assessed. - The authors did not comment on the penetrance of the propranolol formulation or include a safety evaluation of the side effects such as hypoglycemia and the effects on heart rate or blood pressure.
- Fifty-nine percent of patients achieved complete responses (mean, 66 days), 18% of patients had stable disease, and 22% of patients did not respond to the treatment.
Other non-surgical treatments that have been used with variable success on these lesions, mostly when they are multiple or recurrent, are steroid injections, imiquimod (medication cream used to treat warts and sun damage, works by stimulating the immune system), silver nitrate, and lasers.
Approximately 40% of pyogenic granulomas come back (recur) after treatment, especially those lesions located on the trunk of teenagers and young adults. Recurrent pyogenic granulomas are best treated by surgical excision.
Pyogenic granuloma prognosis
Since most pyogenic granulomas do not regress spontaneously and may bleed, ulcerate, or be cosmetically disfiguring, they may necessitate treatment on these grounds 33. There is a high chance that the problem will come back if the whole granuloma is not destroyed during treatment. Partial resection by shave excision or curettage may lead to recurrence in the future. There is a risk of up to 15% of the pyogenic granuloma coming back. In these cases, the area is sometimes cut out and the wound closed with stitches. A scar may remain after treatment.
Oral pyogenic granulomas occurring in pregnant women usually regress once they deliver their baby 38.
References- Sarwal P, Lapumnuaypol K. Pyogenic Granuloma. [Updated 2022 Oct 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556077
- Wollina U, Langner D, França K, Gianfaldoni S, Lotti T, Tchernev G. Pyogenic Granuloma – A Common Benign Vascular Tumor with Variable Clinical Presentation: New Findings and Treatment Options. Open Access Maced J Med Sci. 2017 Jul 13;5(4):423-426. doi: 10.3889/oamjms.2017.111
- Browning, J.C., Eldin, K.W., Kozakewich, H.P.W., Mulliken, J.B. and Bree, A.F. (2009), Congenital Disseminated Pyogenic Granuloma. Pediatric Dermatology, 26: 323-327. https://doi.org/10.1111/j.1525-1470.2008.00858.x
- Putra, J, Rymeski, B, Merrow, AC, Dasgupta, R, Gupta, A. Four cases of pediatric deep-seated/subcutaneous pyogenic granuloma: Review of literature and differential diagnosis, J Cutan Pathol, 2017. https://doi.org/10.1111/cup.12923
- Alomari MH, Kozakewich HPW, Kerr CL, Uller W, Davis SL, Chaudry G, Liang MG, Orbach DB, Mulliken JB, Greene AK, Afshar S, Fishman SJ, Taghinia AH, Al-Ibraheemi A, Alomari AI. Congenital Disseminated Pyogenic Granuloma: Characterization of an Aggressive Multisystemic Disorder. J Pediatr. 2020 Nov;226:157-166. doi: 10.1016/j.jpeds.2020.06.079
- Lee J, Sinno H, Tahiri Y, Gilardino MS. Treatment options for cutaneous pyogenic granulomas: a review. J Plast Reconstr Aesthet Surg. 2011 Sep;64(9):1216-20. doi: 10.1016/j.bjps.2010.12.021
- Patrizi, A., Gurioli, C. and Dika, E. (2015), Pyogenic granulomas in childhood: New treatment modalities. Dermatologic Therapy, 28: 332-332. https://doi.org/10.1111/dth.12237
- Pyogenic Granuloma of the Conjunctiva. N Engl J Med 2017; 376:1667 DOI: 10.1056/NEJMicm1613657 https://www.nejm.org/doi/full/10.1056/NEJMicm1613657
- Bacher J, Assaad D, Adam DN. Pyogenic granuloma of the foot with satellitosis: a role for conservative management. J Cutan Med Surg. 2011 Jan-Feb;15(1):58-60. doi: 10.2310/7750.2010.09068
- Beers BB, Rustad OJ, Vance JC. Pyogenic granuloma following laser treatment of a port-wine stain. Cutis. 1988 Apr;41(4):266-8.
- Aghaei S. Pyogenic granuloma arising in port-wine stain after cryotherapy. Dermatol Online J. 2003 Dec;9(5):16. https://escholarship.org/uc/item/5wj259vv
- Groesser L, Peterhof E, Evert M, Landthaler M, Berneburg M, Hafner C. BRAF and RAS Mutations in Sporadic and Secondary Pyogenic Granuloma. J Invest Dermatol. 2016 Feb;136(2):481-6. doi: 10.1038/JID.2015.376
- Bouscarat F, Bouchard C, Bouhour D. Paronychia and pyogenic granuloma of the great toes in patients treated with indinavir. N Engl J Med. 1998 Jun 11;338(24):1776-7. doi: 10.1056/NEJM199806113382417
- V. Piguet, L. Borradori, Pyogenic granuloma‐like lesions during capecitabine therapy, British Journal of Dermatology, Volume 147, Issue 6, 1 December 2002, Pages 1270–1272, https://doi.org/10.1046/j.1365-2133.2002.05000_6.x
- Curr, N., Saunders, H., Murugasu, A., Cooray, P., Schwarz, M. and Gin, D. (2006), Multiple periungual pyogenic granulomas following systemic 5-fluorouracil. Australasian Journal of Dermatology, 47: 130-133. https://doi.org/10.1111/j.1440-0960.2006.00248.x
- C. Devillers, O. Vanhooteghem, A. Henrijean, M. Ramaut, M. De La Brassinne, Subungueal pyogenic granuloma secondary to docetaxel therapy, Clinical and Experimental Dermatology, Volume 34, Issue 2, 1 March 2009, Pages 251–252, https://doi.org/10.1111/j.1365-2230.2008.02799.x
- Paul LJ, Cohen PR. Paclitaxel-associated subungual pyogenic granuloma: report in a patient with breast cancer receiving paclitaxel and review of drug-induced pyogenic granulomas adjacent to and beneath the nail. J Drugs Dermatol. 2012 Feb;11(2):262-8.
- High WA. Gefitinib: a cause of pyogenic granulomalike lesions of the nail. Arch Dermatol. 2006 Jul;142(7):939. doi: 10.1001/archderm.142.7.939-a
- Segaert S, Van Cutsem E. Clinical signs, pathophysiology and management of skin toxicity during therapy with epidermal growth factor receptor inhibitors. Ann Oncol. 2005 Sep;16(9):1425-33. doi: 10.1093/annonc/mdi279
- Dika E, Barisani A, Vaccari S, Fanti PA, Ismaili A, Patrizi A. Periungual pyogenic granuloma following imatinib therapy in a patient with chronic myelogenous leukemia. J Drugs Dermatol. 2013 May;12(5):512-3. https://jddonline.com/articles/periungual-pyogenic-granuloma-following-imatinib-therapy-in-a-patient-with-chronic-myelogenous-leuke-S1545961613P0512X
- Henning B, Stieger P, Kamarachev J, Dummer R, Goldinger SM. Pyogenic granuloma in patients treated with selective BRAF inhibitors: another manifestation of paradoxical pathway activation. Melanoma Res. 2016 Jun;26(3):304-7. doi: 10.1097/CMR.0000000000000248
- Sammut SJ, Tomson N, Corrie P. Pyogenic granuloma as a cutaneous adverse effect of vemurafenib. N Engl J Med. 2014 Sep 25;371(13):1265-7. doi: 10.1056/NEJMc1407683
- Patruno, C., Balato, N., Cirillo, T., Napolitano, M. and Ayala, F. (2013), Etanercept and pyogenic granuloma. Dermatol Ther, 26: 493-495. https://doi.org/10.1111/dth.12022
- Sibaud V, Dalenc F, Mourey L, Chevreau C. Paronychia and pyogenic granuloma induced by new anticancer mTOR inhibitors. Acta Derm Venereol. 2011 Sep;91(5):584-5. doi: 10.2340/00015555-1097
- Exner JH, Dahod S, Pochi PE. Pyogenic Granuloma-like Acne Lesions During Isotretinoin Therapy. Arch Dermatol. 1983;119(10):808–811. doi:10.1001/archderm.1983.01650340018012
- Benedetto C, Crasto D, Ettefagh L, Nami N. Development of Periungual Pyogenic Granuloma with Associated Paronychia Following Isotretinoin Therapy: A Case Report and a Review of the Literature. J Clin Aesthet Dermatol. 2019 Apr;12(4):32-36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6508482
- Lenczowski JM, Cassarino DS, Jain A, Turner ML. Disseminated vascular papules in an immunodeficient patient being treated with granulocyte colony-stimulating factor. J Am Acad Dermatol. 2003 Jul;49(1):105-8. doi: 10.1067/mjd.2003.306
- Palmero ML, Pope E. Eruptive pyogenic granulomas developing after drug hypersensitivity reaction. J Am Acad Dermatol. 2009 May;60(5):855-7. doi: 10.1016/j.jaad.2008.11.021
- Cheney-Peters D, Lund TC. Oral Pyogenic Granuloma After Bone Marrow Transplant in the Pediatric/Adolescent Population: Report of 5 Cases. J Pediatr Hematol Oncol. 2016 Oct;38(7):570-3. doi: 10.1097/MPH.0000000000000593
- Kanda Y, Arai C, Chizuka A, Suguro M, Hamaki T, Yamamoto R, Yamauchi Y, Matsuyama T, Takezako N, Shirai Y, Miwa A, Iwasaki K, Nasu M, Togawa A. Pyogenic granuloma of the tongue early after allogeneic bone marrow transplantation for multiple myeloma. Leuk Lymphoma. 2000 Apr;37(3-4):445-9. doi: 10.3109/10428190009089447
- Bachmeyer C, Devergie A, Mansouri S, Dubertret L, Aractingi S. Botriomycome de la langue au cours de la maladie chronique du greffon contre l’hôte [Pyogenic granuloma of the tongue in chronic graft versus host disease]. Ann Dermatol Venereol. 1996;123(9):552-4. French.
- Lee L, Miller PA, Maxymiw WG, Messner HA, Rotstein LE. Intraoral pyogenic granuloma after allogeneic bone marrow transplant. Report of three cases. Oral Surg Oral Med Oral Pathol. 1994 Nov;78(5):607-10. doi: 10.1016/0030-4220(94)90173-2
- Kapadia SB, Heffner DK. Pitfalls in the histopathologic diagnosis of pyogenic granuloma. Eur Arch Otorhinolaryngol. 1992;249(4):195-200. doi: 10.1007/BF00178468
- Pyogenic granuloma. https://dermnetnz.org/topics/pyogenic-granuloma
- Oke I, Alkharashi M, Petersen RA, Ashenberg A, Shah AS. Treatment of Ocular Pyogenic Granuloma With Topical Timolol. JAMA Ophthalmol. 2017 Apr 1;135(4):383-385. doi: 10.1001/jamaophthalmol.2017.0110
- Jaiswal H, Patidar N, Shah C, Singh R, Jain E, Piyush P. Topical timolol 0.5% as the primary treatment of ophthalmic pyogenic granuloma: A prospective, single-arm study. Indian J Ophthalmol. 2021 May;69(5):1155-1160. doi: 10.4103/ijo.IJO_2404_20
- Neri, I, Baraldi, C, Balestri, R, Piraccini, BM, Patrizi, A. Topical 1% propranolol ointment with occlusion in treatment of pyogenic granulomas: An open-label study in 22 children. Pediatr Dermatol. 2018; 35: 117– 120. https://doi.org/10.1111/pde.13372
- Løes S, Tornes K. Misinterpretation of histopathological results as an important risk factor for unneeded surgery – case report of a “near miss” event in a pregnant woman. Patient Saf Surg. 2008 Jun 5;2:14. doi: 10.1186/1754-9493-2-14