Trichothiodystrophy
Trichothiodystrophy also called TTD, Amish brittle hair syndrome or brittle hair-intellectual impairment-decreased fertility-short stature syndrome (BIDS syndrome), is a rare inherited condition that affects many parts of the body. The hallmark of trichothiodystrophy is brittle hair that is sparse and easily broken. Tests show that the hair is lacking sulfur (due to an abnormal synthesis of the sulphur containing keratins), an element that normally gives hair its strength.
The signs and symptoms of trichothiodystrophy vary widely. Mild cases may involve only the hair. More severe cases also cause delayed development, significant intellectual disability, and recurrent infections; severely affected individuals may survive only into infancy or early childhood.
Mothers of children with trichothiodystrophy may experience problems during pregnancy including pregnancy-induced high blood pressure (preeclampsia) and a related condition called HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome that can damage the liver. Babies with trichothiodystrophy are at increased risk of premature birth, low birth weight, and slow growth.
Most affected children have short stature compared to others their age. Intellectual disability and delayed development are common, although most affected individuals are highly social with an outgoing and engaging personality. Some have brain abnormalities that can be seen with imaging tests. Trichothiodystrophy is also associated with recurrent infections, particularly respiratory infections, which can be life-threatening. Other features of trichothiodystrophy can include dry, scaly skin (ichthyosis); abnormalities of the fingernails and toenails; clouding of the lens in both eyes from birth (congenital cataracts); poor coordination; and skeletal abnormalities.
About half of all people with trichothiodystrophy have a photosensitive form of the disorder, which causes them to be extremely sensitive to ultraviolet (UV) rays from sunlight. They develop a severe sunburn after spending just a few minutes in the sun. However, for reasons that are unclear, they do not develop other sun-related problems such as excessive freckling of the skin or an increased risk of skin cancer. Many people with trichothiodystrophy report that they do not sweat.
Trichothiodystrophy has an estimated incidence of about 1 in 1 million newborns in the United States and Europe. About 100 affected individuals have been reported worldwide 1.
The diagnostic findings of trichothiodystrophy are short, unruly, brittle hair, with alternating dark and light bands under polarizing microscopy (tiger-tail pattern), trichoschisis (or trichorrhexis), and an absent or defective cuticle visualized by scanning electron microscopy.
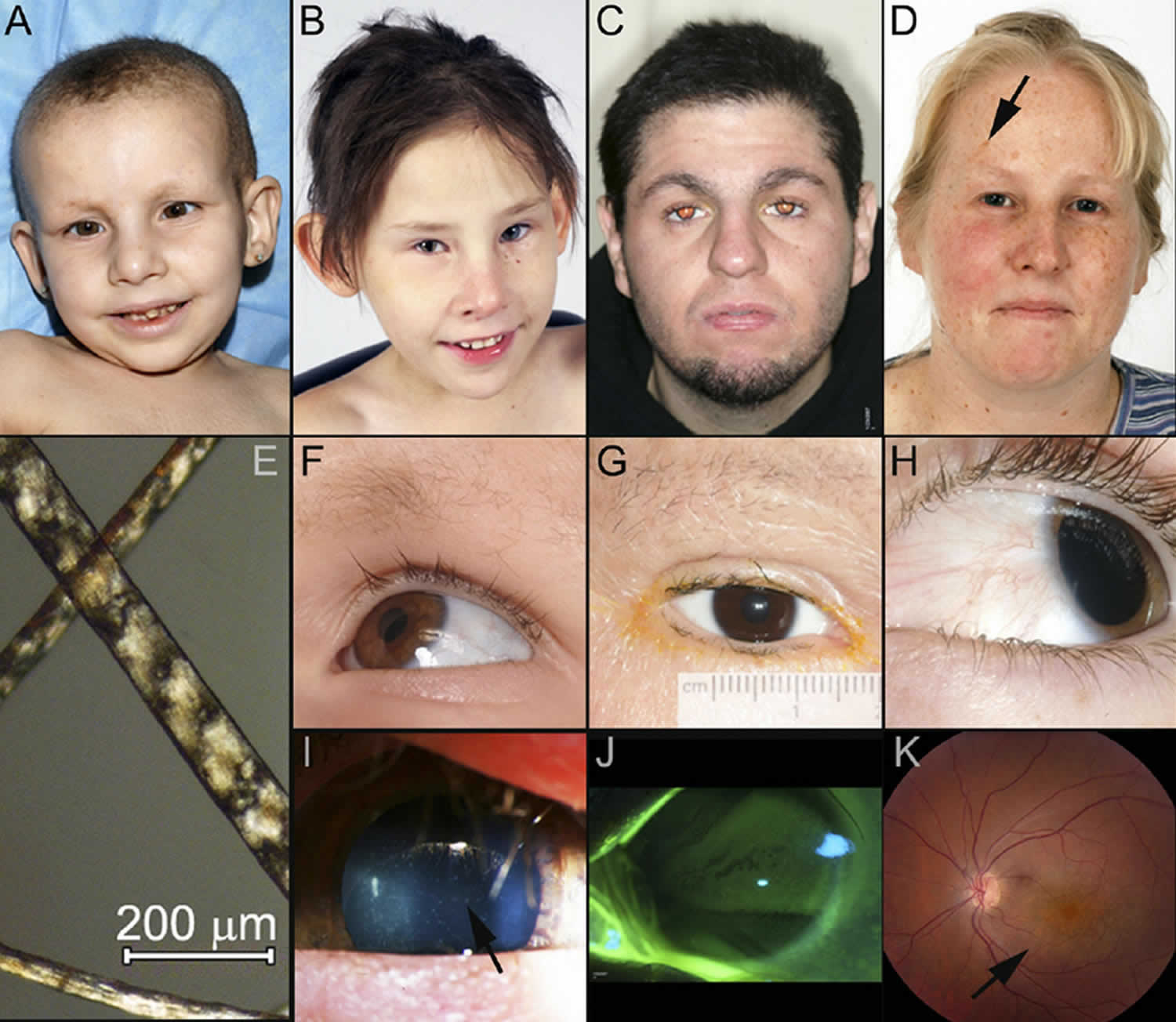
Figure 1. Trichothiodystrophy
Footnote: Clinical spectrum of trichothiodystrophy. (A) Trichothiodystrophy and psychomotor retardation in a 2-year-old girl. trichothiodystrophy and photosensitivity in a 9-year-old boy showing (B) distinctive facial features and (C) hair abnormality. The patient also had ichthyosis and was found to have mutations within the XPD (ERCC2) gene.
[Source 2 ]Figure 2. Trichothiodystrophy syndrome
Footnote: Distinctive features of trichothiodystrophy (TTD) and xeroderma pigmentosum (XP)/trichothiodystrophy-affected patients. Trichothiodystrophy patients present with widely varying degrees of facial dysmorphia, hair abnormalities, and ocular characteristics. (A) Case 1, 7-year-old patient trichothiodystrophy who exhibits facial dysmorphia, ichthyosis, and extremely short, brittle hair. (B) Case 2, 6-year-old patient trichothiodystrophy with microphthalmia, microcornea, large ears, and dysmorphic facial features but long hair. (C) Case 3, 26-year-old patient trichothiodystrophy who has unremarkable facial features and relatively long hair. (D) Case 4, 30-year-old patient xeroderma pigmentosum-trichothiodystrophy, who has very long hair, facial lentigines (arrow), and freckling, normal-appearing eyebrows and lashes, and corneal neovascularization OS. Note that all trichothiodystrophy and xeroderma pigmentosum-trichothiodystrophy patients, including those with normal-appearing hair, still exhibited tiger-tail banding under polarizing light microscopy. (E) Banding seen in the magnified hair of Case 1. (F) The combination of extremely brittle or sparse eyebrows, and long, thick upper lashes common in most of the trichothiodystrophy patients, shown here in Case 1. G, Microcornea and extremely brittle or sparse eyebrows and eyelashes in 19-year-old patient trichothiodystrophy. (H) Long eyelashes and early pterygium in 5-year-old patient xeroderma pigmentosum-trichothiodystrophy. (I) Visually insignificant punctate corneal opacities (arrow) in Case 2, photographed at 3 years old. (J) Slit lamp photograph of the cornea of Case 3 using fluorescein staining. Damaged/degenerated epithelial cells are stained bright green, Oxford scale grade 6. (K) Fundus photograph also from Case 3 (age 26 at time of photo) showing focal primary retinal degeneration (arrow).
[Source 3 ]Trichothiodystrophy causes
Most cases of the photosensitive form of trichothiodystrophy result from mutations in one of three genes: ERCC2 (XPD), ERCC3, or GTF2H5. The proteins produced from these genes work together as part of a group of proteins called the general transcription factor IIH (TFIIH) complex. This complex is involved in the repair of DNA damage, which can be caused by UV radiation from the sun. The TFIIH complex also plays an important role in gene transcription, which is the first step in protein production.
Mutations in the ERCC2, ERCC3, or GTF2H5 genes reduce the amount of TFIIH complex within cells, which impairs both DNA repair and gene transcription. An inability to repair DNA damage probably underlies the sun sensitivity in affected individuals. Studies suggest that many of the other features of trichothiodystrophy may result from problems with the transcription of genes needed for normal development before and after birth.
Mutations in at least one gene, MPLKIP, have been reported to cause a non-photosensitive form of trichothiodystrophy. Mutations in this gene account for fewer than 20 percent of all cases of non-photosensitive trichothiodystrophy. Little is known about the protein produced from the MPLKIP gene, although it does not appear to be involved in DNA repair. It is unclear how mutations in the MPLKIP gene lead to the varied features of trichothiodystrophy.
In some cases, the genetic cause of trichothiodystrophy is unknown.
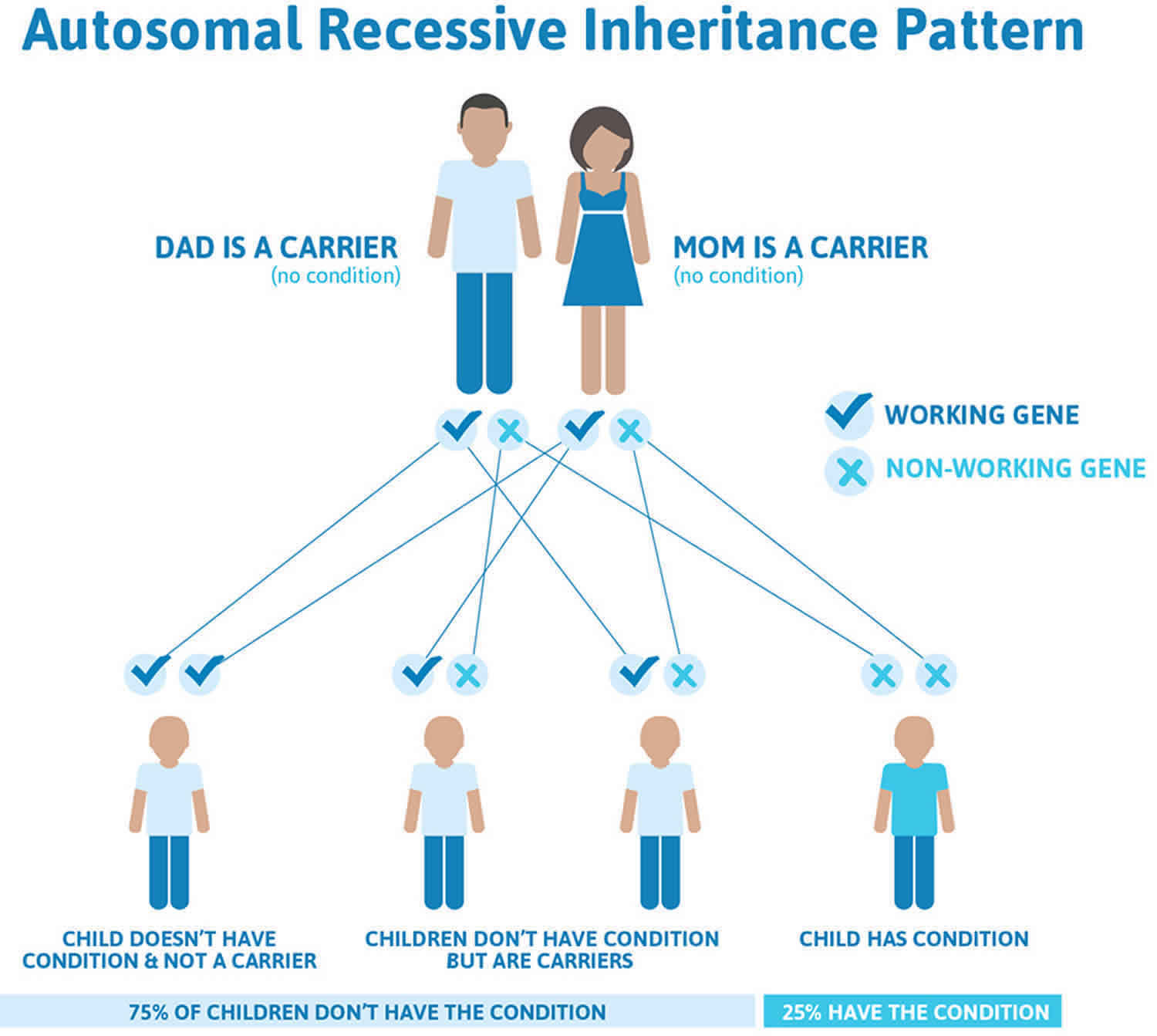
Trichothiodystrophy inheritance pattern
Trichothiodystrophy is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 3 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 3. Trichothiodystrophy autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Trichothiodystrophy symptoms
Within the spectrum of the trichothiodystrophy syndromes are numerous syndromes affecting mainly organs derived from the neuroectoderm 4. The clinical appearance is always characterized by brittle and fragile hair, often combined with growth retardation and intellectual deficit, congenital ichthyosis and nail abnormalities, among other symptoms. The abnormalities are usually obvious at birth, with variable clinical expression. The variants of trichothiodystrophy, depending on their different associations, are: BIDS syndrome (or trichothiodystrophy type D or Amish Brittle Hair syndrome), IBIDS syndrome (or Tay syndrome or trichothiodystrophy type E), PIBIDS syndrome (or trichothiodystrophy type F), Sabinas syndrome (trichothiodystrophy type B), SIBIDS syndrome, ONMRS (Itin syndrome) and Pollitt syndrome (trichothiodystrophy type C).
Pregnancy and newborn symptoms
The first sign an infant may have trichothiodystrophy may be before birth. Maternal complications during pregnancy such as pre-eclampsia, HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome, premature labor and placental abnormalities occur in approximately 81% of trichothiodystrophy pregnancies. The trichothiodystrophy infants often are low birth weight (<2500 grams) and are born with a collodion membrane on the skin. The low birth weight and collodion membrane are serious complications, and many trichothiodystrophy infants are admitted to the neonatal intensive care unit (NICU). In addition to the skin abnormalities, trichothiodystrophy infants may have feeding difficulties and experience gastrointestinal reflux with aspiration and require nasogastric feeding tubes for the first several weeks of life. Many trichothiodystrophy infants will be discharged from the NICU after several weeks, then require close medical monitoring at home for several months; they often qualify for state early childhood intervention programs. Skin, Hair and Nail Symptoms
When the collodion membrane peels off in the newborn period, the skin in many areas of the body may be covered with fine scale called ichthyosis. The scale over time can thicken and darken especially at the waist and flanks; due to the scaly dry nature of their skin, trichothiodystrophy patients can have issues with chronic itching (pruritis). In addition, some children with trichothiodystrophy may not sweat very much and may have issues with hyperthermia in warmer climates. The skin on the palms and soles of the feet is often thickened and dry; painful fissures in flexural areas such as over the knuckles of the hands and instep of the foot can occur. Hyperlinear palms and soles can also be seen in many trichothiodystrophy children and adults. Eczema occurs in a small percentage of patients and increases the problems with the pruritis. Symptomatic management of the ichthyosis and dry skin is a daily process of gently removing thickened scale during bathing and followed by moisturizing the skin. Moisturizers or emollient creams and lotions are designed to make the external layers of the skin (epidermis) softer and more pliable. They also increase the skin’s hydration (water content) by reducing evaporation. The moisturizers ideally are fragrance and dye free.
For the trichothiodystrophy patients who are photosensitive, UV protection is important to prevent severe burns. Patients should avoid being outside for prolonged periods without protection. They should wear hats, sunglasses and clothing to cover their skin, such as long sleeves and long pants. When going outside during the day, they should have sunscreen applied to uncovered skin such as face, neck, ears and hands. UV can come from other artificial light sources such as halogen and florescent light bulbs and mercury vapor lamps. Photosensitive patients should avoid these types of light sources. Most trichothiodystrophy patients are not at an increased risk for skin cancer, however there are a few rare patients who exhibit symptoms of both xeroderma pigmentosum (XP) and trichothiodystrophy (the XP-trichothiodystrophy syndrome) and may develop skin cancers after UV exposure. These patients require more stringent UV protection.
The scalp hair is brittle and can be sparse; it breaks easily and, in some patients, will fall out during fever (febrile) illnesses. The hair may be ‘fine’ and feel soft or it may feel more course and dry. It can be fragile and break off after a slight amount of ‘trauma’ such as combing, and for some affected people, hair breaks so easily that there are broken hairs on the pillow after sleeping. trichothiodystrophy patients may not need many haircuts; however, they can have more hair on the top of their heads and little to no hair on the sides or back. Testing of the hair in a specialty laboratory shows low sulfur content and abnormal levels of the amino acid cystine.
The scalp skin can be icthyotic, and some trichothiodystrophy patients have such thick adherent scale in the scalp that it further impedes hair growth. Applying oil to the scalp and then washing the hair with a gentle shampoo designed for scaling skin conditions can help loosen the scale.
The eyebrows are also sparse and brittle and the hair of the eyebrows may break off as well. In many patients, the eyelashes may be nearly normal. trichothiodystrophy children often have a smaller receding chin, and larger appearing ears.
Onychodystrophy, an alteration of nail development, is a common finding in trichothiodystrophy. The nails may be abnormally short, broad and ridged, and may be soft and split easily. They may also be thick, brittle and slow growing. The nails may demonstrate koilynichia, a turning upward at the tips of the nails. Another term to describe this nail abnormality is ‘spooned’. It can be helpful to include the nails when moisturizing the skin of the hands and palms.
Growth and feeding effects
Trichothiodystrophy children have short stature, many have poor weight gain, and often will not grow along the standard growth curves. However, they do grow at their own rate and should be followed with growth curves. Most children and adults with trichothiodystrophy will be shorter than their peers. It appears that growth hormone treatment is not helpful to increase overall height.
People with trichothiodystrophy can have problems with chronic gastroesophageal reflux disease and may need medications and feeding modifications to manage the symptoms. Due to feeding problems and poor weight gain, some trichothiodystrophy children will have feeding tubes (either gastrostomy or nasogastric tubes) placed to augment oral feeding. As trichothiodystrophy children age, they may lose subcutaneous fat associated with the poor weight gain, resulting in a thinner prematurely aged-looking face.
Hematologic and immune effects
Trichothiodystrophy children may also have recurrent infections. The most common infections occur in the gastrointestinal and respiratory tracts and these infections can be life threatening. The children may have low levels of neutrophils, a type of white blood cell important in fighting infections. They may also have lower levels of immunoglobins especially immunoglobin G (IgG) in the blood. This blood protein is also important in fighting infections and some trichothiodystrophy children have received IgG infusions to help treat the recurrent infections. Anemia and low iron levels are also seen in trichothiodystrophy children; they can be treated with dietary iron supplementation.
Ocular (Eye) effects
Trichothiodystrophy patients have a wide variety of ocular abnormalities and ophthalmologic care is an important part of their health monitoring. In some patients, ocular abnormalities are present at birth; however other patients may not develop ocular problems until later in childhood. The most common findings in the newborn period are congenital cataracts and nystagmus (an eye finding where the eyes make repetitive, uncontrolled movements that can affect visual acuity and depth perception). trichothiodystrophy children can also develop cataracts at later ages, and identification and surgical removal of the cataracts as soon as they become visually significant is important to preserve eyesight. Other ocular abnormalities seen in trichothiodystrophy children include small corneas (microcornea) and small eyeballs (microphthalmia) with decreased best corrected vision. As patients with trichothiodystrophy become older, they can develop dry eyes, leading to corneal surface abnormalities. Normally dry eye is a condition seen in older adults, and this trichothiodystrophy complication is often not identified until the child becomes symptomatic. A few trichothiodystrophy patients may develop a macular/retinal degeneration as they age.
Skeletal and dental effects
Skeletal and dental abnormalities may also be present. trichothiodystrophy patients have been found to have unusual skeletal findings. They have thick dense bones (osteosclerosis) in the central skeleton including the skull, spine and pelvis. They also have thinner bone (osteopenia) in the peripheral bones of the lower arms, hands and feet. The bone symptoms can vary between people with the condition.
Trichothiodystrophy patients often have poorly developed teeth. The tooth enamel is often thin and hypoplastic, leading to recurrent cavities (caries). Trichothiodystrophy children may need extensive dental care including extractions and tooth caps.
Neurologic effects
Most children and adults with trichothiodystrophy have some form of developmental delay. Small head size (microcephaly) is also a common finding in trichothiodystrophy children and adults. Often, these children do not walk or talk at the usual ages. Many children with trichothiodystrophy will have MRI scans of the brain for evaluation of the developmental delay. Most trichothiodystrophy children are found to have an abnormal amount of myelin (white matter) in the brain and central nervous system. The myelin acts as an ‘insulator’ around nerve sheaths, helping to speed up nerve transmission. In addition, trichothiodystrophy children can have tremors and difficulty coordinating fine and gross muscle coordination. A few patients have developed seizures. Hearing loss can also be seen but it is generally due to recurrent ear infections and not nerve deafness. Despite the developmental delays, individuals with trichothiodystrophy are outgoing and highly social.
Miscellaneous effects
Boys with trichothiodystrophy may have cryptorchidism, a condition where the testes fail to descend into the scrotum. They generally require surgery to correct the condition. In women, breast tissue may be sparsely developed in spite of normal development of the nipples. A few trichothiodystrophy females have developed menstruation.
Trichothiodystrophy diagnosis
An initial evaluation for trichothiodystrophy involves a diagnostic work-up, including obtaining a detailed history of the patient’s prenatal and neonatal history. A detailed physical exam is performed to assess clinical features such as hair abnormalities, short stature, small chin, ichthyosis, intellectual impairment or developmental delay, and bone and teeth anomalies. Evaluation by a developmental pediatrician or neurologist may determine whether there is any developmental delay or intellectual impairment. MRI imaging of the brain to identify abnormal patterns of myelination is often performed. Laboratory testing for immune function, blood count and iron levels can also be performed. trichothiodystrophy is typically diagnosed by polarized light microscopy of hair shafts, revealing a tiger-tail pattern, and at times by measurement of reduced sulfur content in patient’s hair. The classical tiger-tail pattern alone usually is enough to diagnose trichothiodystrophy. However, there are other conditions with similar hair shaft abnormalities and often genetic testing is ordered to confirm the diagnosis. However, there are a few patients with features of trichothiodystrophy who will not have mutations in the known genes. They may have mutations in yet to be identified trichothiodystrophy associated genes.
Trichothiodystrophy treatment
Trichothiodystrophy patients generally have complex health care needs and benefit from a multidisciplinary approach to their medical management. Patients who are sensitive to ultraviolent rays must be protected from exposure to the sun and other sources of ultraviolet radiation. Monitoring for developmental delay with special education services may be required in school and the children should be evaluated for rehabilitation needs. Ongoing physical therapy may be advised for joint stiffness, muscle tightening (contractures), and poor coordination. Specialized health care providers may be involved in medical management depending on symptoms (i.e. neurologists for seizures, dermatologists for skin symptoms, endocrinologists for growth issues). Skin symptoms of dry skin (ichthyosis) are treated by applying skin softening emollients and products containing alpha-hydroxy acids which help break down skin buildup (keratolytics).This can be particularly effective after bathing while the skin is still moist. Individuals with frequent infections may benefit from prophylactic antibiotics and in some patients, administration of IgG. No formal guidelines for the medical management of trichothiodystrophy exist and management is largely based on symptoms and clinical manifestations.
Genetic counseling is recommended for families of children with trichothiodystrophy.
Trichothiodystrophy life expectancy
At present the clinical course of trichothiodystrophy syndrome patients is not known 5.
References- Trichothiodystrophy. https://ghr.nlm.nih.gov/condition/trichothiodystrophy
- Itin, P., Sarasin, A., & Pittelkow, M. (2001). Trichothiodystrophy: update on the sulfur-deficient brittle hair syndromes. Journal of the American Academy of Dermatology, 44 6, 891-920; quiz 921-4.
- Brooks, Brian & Thompson, Amy & Clayton, Janine & Chan, Chi-Chao & Tamura, Deborah & Zein, Wadih & Blain, Delphine & Hadsall, Casey & Rowan, John & Bowles, Kristen & Khan, Sikandar & Ueda, Takahiro & Boyle, Jennifer & Oh, Kyu-Seon & DiGiovanna, John & Kraemer, Kenneth. (2011). Ocular Manifestations of Trichothiodystrophy. Ophthalmology. 118. 2335-42. 10.1016/j.ophtha.2011.05.036
- Trichothiodystrophy. https://rarediseases.info.nih.gov/diseases/12109/trichothiodystrophy
- Kraemer KH, Patronas NJ, Schiffmann R, Brooks BP, Tamura D, DiGiovanna JJ. Xeroderma pigmentosum, trichothiodystrophy and Cockayne syndrome: a complex genotype-phenotype relationship. Neuroscience. 2007;145(4):1388-1396. doi:10.1016/j.neuroscience.2006.12.020