Xia Gibbs syndrome
Xia-Gibbs syndrome is a neurological disorder characterized by weak muscle tone (hypotonia), mild to severe intellectual disability and delayed development 1. Expressive language skills (vocabulary and the production of speech) are particularly affected; children with Xia-Gibbs syndrome usually do not speak their first word, a milestone typically achieved within the first year, until age two or later, and some never learn to talk. Development of motor skills, such as crawling and walking, can also be delayed. Males usually have more severe symptoms than females.
Other signs and symptoms of Xia-Gibbs syndrome vary among affected individuals. Additional neurological features include poor coordination and balance (ataxia) and seizures. Feeding problems and sleep abnormalities can also occur in people with the condition, and many affected individuals experience short pauses in breathing while they sleep (obstructive sleep apnea). In some people with Xia-Gibbs syndrome, imaging tests of the brain show abnormalities in the brain’s structure. For example, the tissue connecting the left and right halves of the brain (the corpus callosum) can be abnormally thin.
Xia-Gibbs syndrome can also affect physical development. Growth is usually impaired, and many affected individuals are shorter than their peers. Side-to-side curvature of the spine (scoliosis) is also a common feature. Some people with Xia-Gibbs syndrome have unusual facial features, such as a broad forehead, low-set ears or ears that stick out, widely space eyes (hypertelorism), eye openings that slant up or down (upslanting palpebral fissures or downslanting palpebral fissures), a flat bridge of the nose, or a thin upper lip. Other, less-common abnormalities involving the bones and skin include premature fusion of certain skull bones (craniosynostosis), unusually loose (lax) joints, and loose skin.
Behavior problems can also occur in Xia-Gibbs syndrome. Some affected individuals have features of autism spectrum disorder, which is characterized by impaired communication and social interactions, or of attention-deficit/hyperactivity disorder (ADHD). Other problems can include aggression, anxiety, poor impulse control, and self-injury.
Brain MRI may show several structural brain defects, such as thinning of the corpus callosum and posterior fossa cysts 2.
Xia-Gibbs syndrome is caused by mutations in the AT-Hook DNA Binding Motif Containing 1 gene (AHDC1) gene 2. Inheritance is autosomal dominant but all reported cases to date have been due to new mutations (de novo), in individuals with no family history 3.
Xia-Gibbs syndrome is thought to be a rare disorder, approximately 100 patients worldwide have been identified with Xia-Gibbs syndrome, nearly all of them in the pediatric age range and the oldest being 29 years of age 4. Doctors believe the condition is underdiagnosed, because many people with intellectual disability never have genetic testing to determine the underlying cause.
Treatment and management is supportive, and ideally, should involve several specialists. This may include careful monitoring of the airways, continuous positive airway pressure at night, frequent growth assessments, physical therapy and early interventions to maximize developmental potential 3.
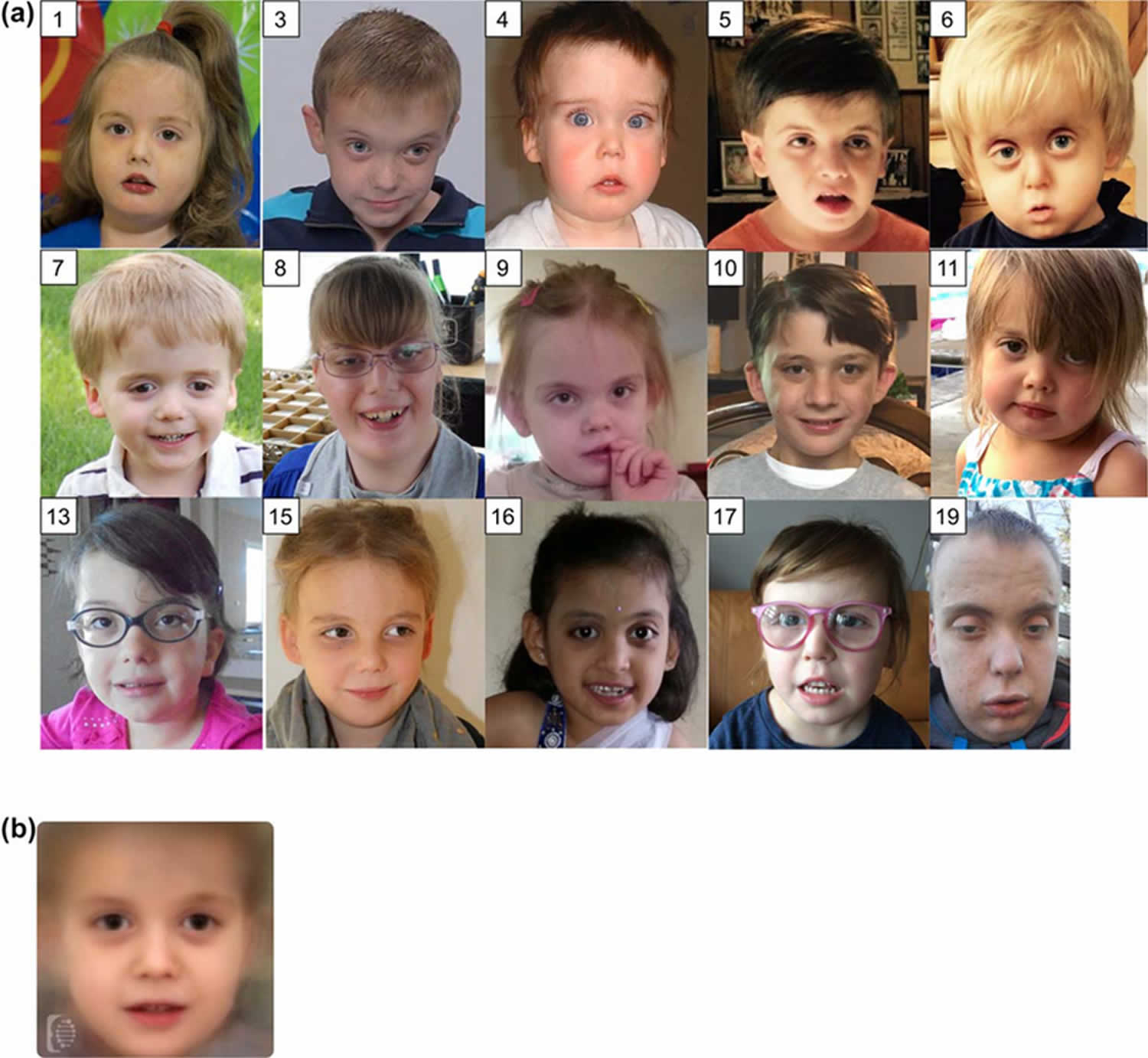
Figure 1. Xia-Gibbs syndrome
Footnote: (a) Frontal face images of some of the patients (accession number in this study are shown at top left corner) (b) A computer generated masking depicting the characteristic features of Xia-Gibbs syndrome. This image was generated using the FDNA software. Overlapping features include a broad forehead, hypertelorism, flat nasal bridge, and thin upper lip.
[Source 3 ]Xia Gibbs syndrome causes
Xia-Gibbs syndrome is caused by mutations in a gene called AHDC1 (AT-Hook DNA Binding Motif Containing 1). AHDC1 gene provides instructions for making a protein with an unknown function. Researchers suspect that the protein may be able to attach (bind) to DNA and control the activity of other genes. Most of the AHDC1 gene mutations involved in Xia-Gibbs syndrome lead to production of abnormally short AHDC1 proteins. The effects of these changes in cells are unclear. The shortened proteins may be quickly broken down or be unable to function. Or, the abnormal proteins may interfere with the function of AHDC1 proteins produced from the normal copy of the gene. Researchers suspect that a reduction in the amount of functional AHDC1 protein impairs normal brain development, leading to intellectual disability, speech problems, and other neurological features of Xia-Gibbs syndrome. Abnormal development of other body systems caused by a shortage of AHDC1 protein may account for additional signs and symptoms of the condition.
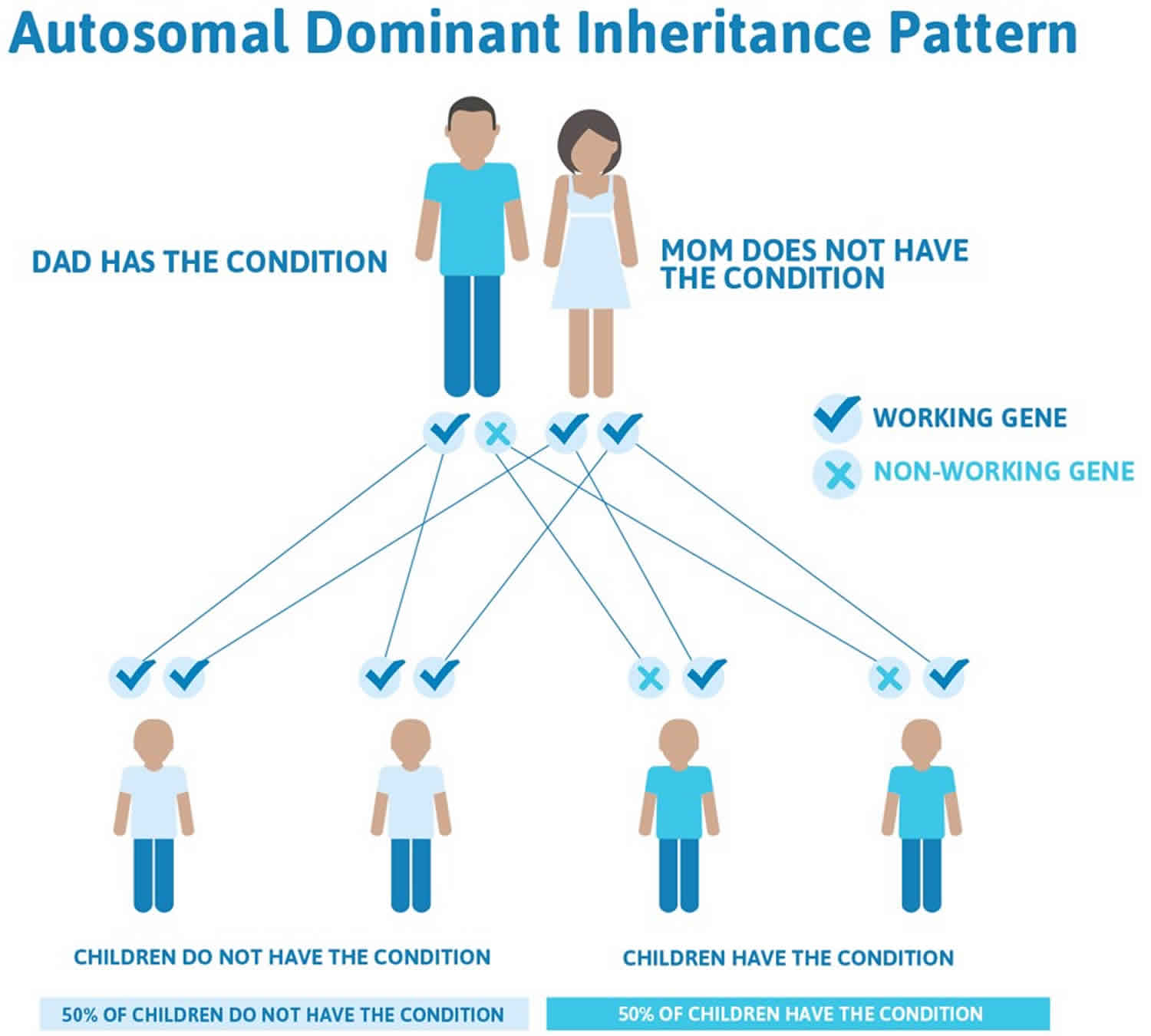
Xia-Gibbs syndrome inheritance pattern
Xia-Gibbs syndrome is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder.
Xia-Gibbs syndrome results from new (de novo) mutations in the gene that occur either during the formation of reproductive cells (eggs or sperm) in an affected individual’s parent or in early embryonic development. Affected individuals have no history of the disorder in their family.
Figure 2. Xia-Gibbs syndrome autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Xia Gibbs syndrome symptoms
People with Xia-Gibbs syndrome usually present with global developmental delay (especially delays in speech), low muscle tone (hypotonia), failure to thrive, short stature, mildly unusual facial features (broad forehead, widely-spaced eyes (hypertelorism), big and low-set ears, flat nasal bridge, and thin upper lip), and breathing difficulties when sleeping (obstructive sleep apnea). The sleep apnea may be due to a collapse of the airway when breathing (tracheomalacia). Xia-Gibbs syndrome other signs and symptoms may include autistic features, seizures, lack of coordination (ataxia), behavioral problems, crossed-eyes (strabismus), delayed myelination, micrognathia, an abnormal lateral curvature of the spine (scoliosis) and other mild dysmorphic features 3. Males usually have more severe symptoms than females.
Language and cognitive problems
A diagnosis of autism, or autism spectrum disorder, had previously been reported in 5 of the 20 patients using the modified checklist for autism in toddlers (M-CHAT) 3. Eight out of 20 patients (40%) were reported to have no speech, four (20%) were reported to use less than 50 words, two (10%) were reported to have a vocabulary of more than 50 words but do not speak in full sentences, and six (30%) patients were reported to use complete sentences with a vocabulary of more than 200 words 3. Among the 12 patients who use at least one word other than “mama” or “dada,” the median age for using one word is 2.75 (1~5) years, while the median age for using two words together is 3.5 (2~6) years 3. These data are consistent with a relationship between gender and speech as male patients are significantly more likely to be nonverbal than female patients 3. It is noteworthy that all the patients reported with no speech are male 3.
Seizures
Seizures were reported in 6 out of 20 (30%) patients. The median onset age of seizure is 4 years old (9 months~12 years old). An abnormal EEG was reported in three out of these six (50%) patients.
Timing of walking
Independent walking is reported in 16 out of 20 patients (80%), with median beginning walking age of 2.5 (1.5~6) years. All the patients who are not able to walk independently are male. However, there is no significant difference between the ability to walk independently between male and female patients. Hypotonia is reported in 18 out of 20 patients (90%).
Scoliosis
Scoliosis was reported in 4 of 20 (20%) patients (ages 10~21 years), and three had received surgery for the condition. Compared to a general population prevalence of idiopathic scoliosis of 0.47–5.2% with an age of onset of 10–15 years, the risk of scoliosis in Xia Gibbs syndrome individuals is significantly increased (compared to 5.2% prevalence) 5. No sex bias was apparent.
Airway and sleep disorder
Sleep apnea was reported in 9 out of 20 patients (45%), three of these nine patients (33.3%) use respiratory support during sleep.
Strabismus
Strabismus was reported in 8 out of 20 patients (40%).
Dysmorphic features
Facial features (Figure 1a) consistently revealed dysmorphic features such as broad forehead, hypertelorism, flat nasal bridge, and thin upper lip. These features are also shown in the composite mask depicting the characteristic appearance of Xia Gibbs syndrome patients (Figure 1b). To date, no patient has been clinically diagnosed based on a recognizable pattern of facial dysmorphisms, or a facial gestalt.
Aggressive behaviors
Aggressive behavior in at least one patient was suggested by Yang et al. 6. Jiang et al 3 were unable to ascertain any history of overtly aggressive behavior in the reported cases, although several parents described a history of self-injury.
Xia Gibbs syndrome diagnosis
Xia-Gibbs syndrome is a rare disorder with approximately 100 patients worldwide have been identified, nearly all of them in the pediatric age range and the oldest being 29 years of age 4. Doctors believe the condition is underdiagnosed, because many people with intellectual disability never have genetic testing to determine the underlying cause.
Xia Gibbs syndrome is diagnosed using whole-exome sequencing (WES) showing truncating variant in the AHDC1 gene. To date, genomic scale sequencing has been widely adopted in the pediatric setting, where it has demonstrated a diagnostic rate of ∼25% 7. Despite examples of its benefit in older patients, it remains underutilized as a diagnostic tool in adults 8.
Abnormal MRI
An abnormal MRI was reported in 12 out of 20 (60%) patients who have had MRI performed. MRI images for re-review were available for six patients. Jiang et al 3 found that 6/6 had thinning of the corpus callosum (Figure 3, compare b–f to “control” individuals a and d). In addition, several subjects were found to have a cyst in the posterior fossa (Subject 4, Figure 3b, Subject 3 Figure 3e, Subject 7, Figure 3h).
Figure 3. Xia Gibbs syndrome MRI scans
Footnote: Brain MRI features of the subjects, unless otherwise indicated a Sagittal T1 image is shown. (a) A control subject (a clinical MRI for history of minor head trauma) in a subject at age 13 months showing a typical corpus callosum (red arrow). (b) Subject 4 at age 6 months, shows thinning of the corpus callosum posteriorly (red arrow) in addition there is a large extra-axial fluid space posterior to the cerebellum. (c) Subject 2 at age 6 months, although the young age limits the assessment, the corpus callosum appears thin (red arrow). (d) A control subject (a clinical MRI for history of seizure) in a subject at age 3 years showing a typical corpus callosum (red arrow). (e) Subject 3 at age 10 years, shows thinning of the corpus callosum (red arrow), particularly in the posterior portion, there is also a large extra-axial fluid space posterior to the cerebellum. (f) Subject 2 (also shown in c) now at age 1 year, a later study confirms the suspicion of the 6-month study suggesting thinning of the corpus callosum. (g) Subject 7 at age 5 years, a T2 axial image shows the extra-axial fluid space around the cerebellum is larger than normal and dysmorphic in appearance. (h) Subject 7 at age 5 years, a T1 sagittal image shows thinning of the corpus callosum and a large extra-axial fluid space posterior to the cerebellum.
[Source 3 ]Xia Gibbs syndrome treatment
Treatment and management is supportive, and ideally, should involve several specialists. This may include careful monitoring of the airways, continuous positive airway pressure at night, frequent growth assessments, physical therapy and early interventions to maximize developmental potential 3.
Xia Gibbs syndrome life expectancy
Xia-Gibbs syndrome was discovered in 2014 2 and only a small number of people around the world have been diagnosed, most of them children. This means that little is known about the condition and how it might affect people in adulthood. However, recently the oldest individual diagnosed with Xia Gibbs syndrome to date was a 55 years of age man with severe intellectual disability, behavioral problems, kyphoscoliosis, and dysmorphic features 9.
References- Xia-Gibbs syndrome. https://ghr.nlm.nih.gov/condition/xia-gibbs-syndrome
- Xia F, Bainbridge MN, Tan TY, et al. De novo truncating mutations in AHDC1 in individuals with syndromic expressive language delay, hypotonia, and sleep apnea. Am J Hum Genet. 2014;94(5):784-789. doi:10.1016/j.ajhg.2014.04.006 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4067559
- Jiang Y, Wangler MF, McGuire AL, et al. The phenotypic spectrum of Xia-Gibbs syndrome. Am J Med Genet A. 2018;176(6):1315-1326. doi:10.1002/ajmg.a.38699 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6231716
- Ritter AL, McDougall C, Skraban C, Medne L, Bedoukian EC, Asher SB, Balciuniene J, Campbell CD, Baker SW, Denenberg EH, et al. 2018. Variable clinical manifestations of Xia–Gibbs syndrome: findings of consecutively identified cases at a single children’s hospital. Am J Med Genet Part A 176: 1890–1896. 10.1002/ajmg.a.40380
- Konieczny MR, Senyurt H, & Krauspe R (2013). Epidemiology of adolescent idiopathic scoliosis. Journal of Children’s Orthopaedics, 7(1), 3–9. 10.1007/s11832-012-0457-4
- Yang H, Douglas G, Monaghan KG, et al. De novo truncating variants in the AHDC1 gene encoding the AT-hook DNA-binding motif-containing protein 1 are associated with intellectual disability and developmental delay. Cold Spring Harb Mol Case Stud. 2015;1(1):a000562. doi:10.1101/mcs.a000562
- Yang Y, Muzny DM, Xia F, Niu Z, Person R, Ding Y, Ward P, Braxton A, Wang M, Buhay C, et al. 2014. Molecular findings among patients referred for clinical whole-exome sequencing. J Am Med Assoc 312: 1870–1879. 10.1001/jama.2014.14601
- Posey JE, Rosenfeld JA, James RA, Bainbridge M, Niu Z, Wang X, Dhar S, Wiszniewski W, Akdemir ZHC, Gambin T, et al. 2016. Molecular diagnostic experience of whole-exome sequencing in adult patients. Genet Med 18: 678–685. 10.1038/gim.2015.142
- Murdock DR, Jiang Y, Wangler M, et al. Xia-Gibbs syndrome in adulthood: a case report with insight into the natural history of the condition. Cold Spring Harb Mol Case Stud. 2019;5(3):a003608. Published 2019 Jun 3. doi:10.1101/mcs.a003608 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6549549