Back pain in children
Back pain in children is not like back pain in adults. Back pain in children and adolescents is a symptom of many different conditions. Compared to an adult, a child with a back pain is more likely to have a serious underlying disorder such as malignancy (cancer) or infection. All lower back pain in children should be considered serious and medical advice should always be sought if the pain persists longer than a few days. This is especially true if your child is 4 years old or younger, or if your child of any age has back pain accompanied by:
- Fever or weight loss
- Weakness or numbness
- Trouble walking
- Pain that radiates down one or both legs
- Bowel or bladder problems
- Pain that keeps the child from sleeping
More serious causes of back pain need early identification and treatment or they may become worse. Always see a doctor if your young child’s back pain lasts for more than several days or progressively worsens.
Fortunately, most back pain in children and teens improves with rest, analgesics and sometimes, physical therapy. But in some cases, the pain lingers or repeatedly returns. If this happens to your child, you should contact your child’s pediatrician or an orthopedic surgeon for further investigation.
Back pain in children is usually assessed by pediatric physicians who specialize in diagnosing and treating spine conditions and injuries in children, teens and young adults.
In rare cases, back pain in children is a symptom of a larger problem that may need surgical intervention to treat.
See your child’s doctor if:
- Your child’s back pain goes down one or both legs, especially if the pain extends below your knee
- Your child’s back pain causes weakness, numbness or tingling in one or both legs
- Your child’s leg, foot, groin or rectal area feels numb
- Your child has fever, nausea, vomiting, abdominal pain, weakness or sweating
- Your child loses control over going to the bathroom
- Your child’s pain was caused by an injury
- Your child’s pain is so intense he/she can’t move around
- Your child’s pain is constant or intense, especially at night or when he/she lies down
- Your child’s back pain occurs with unintended weight loss
- Your child’s back pain occurs with swelling or redness on his/her back
- Your child’s back pain doesn’t seem to be getting better after 1 to 2 weeks of home treatment.
If your child has any of the following symptoms in addition to the back pain, see your doctor straight away. Your child may need immediate medical help.
- Fever of 100º F (38º C) or above
- Unexplained weight loss
- Swelling of the back
- Constant back pain that does not ease after lying down
- Pain in your chest or high up in your back
- Pain down your legs and below the knees
- Pain caused by a recent trauma or injury to your back
- Loss of bladder control
- Inability to pass urine
- Loss of bowel control
- Numbness (loss of feeling, or a tingling sensation) around your genitals, buttocks or anal area
- Pain that is worse at night.
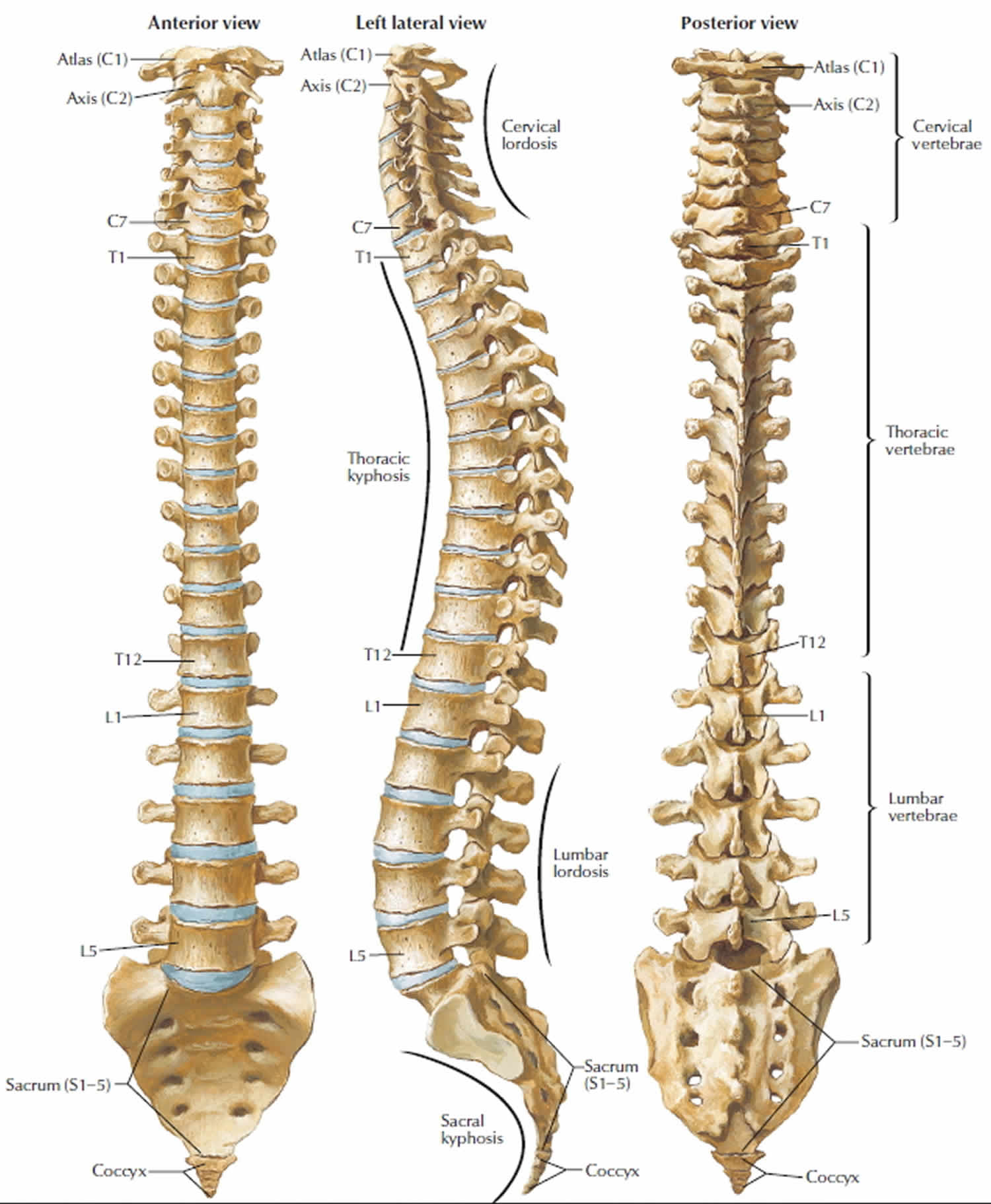
Figure 1. Vertebral column (spinal column)
Footnote: Your spine is made up of small bones, called vertebrae, which are stacked on top of one another and create the natural curves of your back.
Back pain in children causes
Many things can cause low back pain or back pain in children. Your spine is a column of bones (vertebrae) held together by muscles, tendons and ligaments and cushioned by shock-absorbing disks. A problem in any part of your spine can cause back pain. A precise cause for the back pain is only identifiable in around 15% of cases.
Most back pain is what’s known as “non-specific” (there’s no obvious cause) or “mechanical” (the pain originates from the joints, bones or soft tissues in and around the spine).
A common cause of back pain is injury to a muscle (strain) or ligament (sprain). Strains and sprains can occur for many reasons, including improper lifting, poor posture and lack of regular exercise. Being overweight may increase your risk of strains and sprains affecting your back.
This type of back pain “non-specific” (there’s no obvious cause):
- tends to get better or worse depending on your position – for example, it may feel better when sitting or lying down
- typically feels worse when moving – but it’s not a good idea to avoid moving your back completely, as this can make things worse
- can develop suddenly or gradually
- might sometimes be the result of poor posture or lifting something awkwardly, but often occurs for no apparent reason
- may be due to a minor injury such as sprain (pulled ligament) or strain (pulled muscle)
- can be associated with feeling stressed or run down
- will usually start to get better within a few weeks
Back pain can also result from more-serious injuries, such as a vertebral fracture or ruptured disk; from arthritis and other age-related changes in your spine; and from certain infections.
Back pain in children is more likely to have a serious cause. The following may be present:
- Developmental disorders: Arthritis of the spine (spondylolysis) or slipping of the vertebral bodies across one another (spondylolisthesis);
- Disc herniation (slipped disc);
- Scheuermann disease: Typically in adolescent males where there is weakening of the vertebral end-plates causing crushing and painless kyphosis (increased curvature of the back producing a ‘hunch’);
- Tumors of the bone or spinal cord;
- Infection of the discs (discitis) or bone (osteomyelitis) mostly in children less than 10 years old;
- Congenital disorders such as scoliosis (lateral curvature of the spine).
Common back pain conditions in children
Muscle strain and imbalances
Musculoskeletal strain is most often responsible for back pain in children and adolescents. This type of pain frequently responds to rest, anti-inflammatory medications, and an exercise program.
Many teenagers may have more persistent back pain. This is often related to tight hamstring muscles and weak abdominal muscles. Having poor posture and carrying a heavy backpack can contribute to this pain. These children seem to improve with a physical therapy program that stresses hamstring stretching, abdominal strengthening and posture correction.
Rounded back or Scheuermann’s kyphosis
In adolescents, increased roundness of the back (when viewed from the side) also called Scheuermann’s kyphosis — is a common cause of pain in the middle of the back (the thoracic spine). Vertebrae become wedged, causing a rounded, or hunched, back. The curved part of the back may ache, and pain may get worse with activity.
Stress fracture of the spine
Spondylolysis or stress fracture, may cause lower back pain in adolescents. The pain occurs in otherwise healthy children or adolescents, and usually happens with vigorous activity. Stress fractures may occur during adolescent growth spurts or in sports that repeatedly twist and hyperextend the spine, like gymnastics, diving, and football.
Pain is usually mild and may radiate to the buttocks and legs. The pain feels worse with activity and better with rest. A child with spondylolysis may walk with a stiff legged gait and only be able to take short steps.
Most children and teens with spondylolysis can be managed with nonoperative treatment such as pain relievers. However, in some cases surgical treatment is necessary to provide pain relief.
If surgery is necessary, the procedure will most likely be a spinal fusion, or less commonly, a reconstruction of the stress fracture.
Slipped vertebra or spondylolisthesis
A slipped vertebra, or spondylolisthesis, occurs when one vertebra shifts forward on the next vertebra directly below. This may sometimes represent progression of a spondylolysis. It usually occurs at the base of the spine (lumbosacral junction). In severe cases, the bone narrows the spinal canal, which presses on the nerves.
Infection
Back pain also can be caused by an infection that involves the disc space, vertebra or the posterior part on the pelvis. In young children, infection in a disk space (diskitis) can lead to back pain. Discitis typically affects children between the ages of 1 and 5 years, although older children and teenagers can also be affected.
A child with discitis may have the following symptoms:
- Pain in the lower back or abdomen and stiffness of the spine
- Walking with a limp, or simply refusing to walk
- Squatting with a straight spine when reaching for something on the floor, rather than bending from the waist
Once diagnosed, the infection usually responds to medications. If diagnosis is delayed, an abscess can develop that may require surgical drainage.
Tumor
On rare occasion, tumors, such as osteoid osteoma, can be responsible for back pain. When they occur, tumors of the spine are most often found in the middle or lower back. Pain is constant and usually becomes worse over time. This pain is progressive; it is unrelated to activity and/or happens at night.
Scoliosis
Though not common, back pain can be caused by a form of scoliosis — including idiopathic scoliosis, congenital scoliosis, neuromuscular scoliosis and early-onset scoliosis.
In many cases, scoliosis can be treated with braces, physical therapy and medication for occasional pain. If your child is experiencing severe back pain due to scoliosis, surgical intervention may be necessary.
Treatments include spinal fusion, growing rods and, in special circumstances, vertical expandable prosthetic titanium ribs (VEPTR).
Adolescent intervertebral disc herniation
Sometimes one of the discs that cushions your child’s vertebrae ruptures or herniates. This puts pressure on your child’s spinal nerves or the spinal cord.
Although less common than the disc problems observed in adults, some adolescents do develop disc disease which can lead to considerable pain and disability.
If your child has long lasting, unrelieved pain caused by a disc herniation, he may require surgical removal of the disc.
Back pain in children diagnosis
Back pain is a symptom of many different conditions. Because of that, doctors use a variety of imaging modalities to help them better pinpoint the source of your child’s back pain.
At your first appointment, the doctor will discuss your symptoms with you and examine your back. An accurate history and physical examination are essential for evaluating acute low back pain.
Often, patients awaken with morning pain or develop pain after minor forward bending, twisting, or lifting. It is also important to note whether it is a first episode or a recurrent episode. Recurrent episodes usually are more painful with increased symptoms. Red flags are often used to distinguish a common, benign episode from a more significant problem that requires urgent workup and treatment. A recent study shows that some red flags are more important than others, and that red flags overall are poor at ruling in more serious causes of low back pain. Patients with back pain in the primary care setting (80 percent) tend to have one or more red flags, but rarely have a serious condition. There are certain signs and symptoms of more serious causes of lower back pain such as cauda equina syndrome, major intra-abdominal pathology, infections, malignancy, and fractures. Cauda equina syndrome and infections require immediate referral.
They will usually assess your ability to sit, stand, walk and lift your legs as well as test the range of movement in your back. To help them diagnose the cause of the pain, they may ask questions about any illnesses or injuries you may have had, your lifestyle and your work. Your back is a complex structure, so finding the exact cause can often be difficult.
Below are some of the questions your doctor may ask. It might be helpful to consider these before your appointment:
- When did the back pain start?
- Where are you feeling pain?
- Is your pain worse at night?
- Constant back pain that does not ease after lying down?
- Numbness (loss of feeling, or a tingling sensation) around your genitals, buttocks or anal area?
- Have you had any back problems before?
- Can you describe the pain?
- What makes the pain better or worse?
- Do you have any weakness or numbness?
- Loss of bowel or bladder function?
- Inability to pass urine
- Do you use illicit drugs (intravenous drug use)?
- Severe pain?
- Do you have fever?
- Do you have unexplained weight loss?
They will first want to make sure your pain is not being caused by a more serious condition. They will ask questions to rule out cancer, a fracture or an infection, although these conditions are uncommon.
If your doctor thinks there may be a more serious cause you will be referred for further tests.
Without signs and symptoms indicating a serious underlying condition, imaging (x-ray or an MRI scan) won’t help the diagnosis of your back pain and does not improve clinical outcomes in these patients 1.
Even with a few weaker red flags, four to six weeks of treatment is appropriate before consideration of imaging studies 2. If a serious condition is suspected, magnetic resonance imaging (MRI) is usually most appropriate. Computed tomography is an alternative if MRI is contraindicated or unavailable 2. Clinical correlation of MRI or computed tomography findings is essential because the likelihood of false-positive results increases with age 3. Radiography may be helpful to screen for serious conditions, but usually has little diagnostic value because of its low sensitivity and specificity.
Laboratory tests such as complete blood count with differential, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level may be beneficial if infection or bone marrow neoplasm is suspected. These tests may be most sensitive in cases of spinal infection because lack of fever and a normal complete blood count are common in patients with spinal infection 4. Because laboratory testing lacks specificity, MRI with and without contrast media and, in many cases, biopsy are essential for accurate diagnosis 4.
Physical examination
During the physical examination, your doctor will carefully check the following:
- Spine. This will include feeling each vertebra and looking for deformities in the alignment and mobility of the spine. Increased roundness of the back (when viewed from the side) or a curve to the side (when viewed from the back) could be important. Your doctor will check posture and walking gait, the ability to bend over to touch the toes, and bending to the right and left. Difficulty with movement may indicate that there is a problem with the joints of the spine.
- Nerves in the back. Problems with the intervertebral disks can cause pressure on the nerves that exit the spine, so your doctor will perform specific tests for that. With your child lying face up, your doctor will raise the legs (straight leg raising test) and may also raise the legs with your child lying face down (reverse straight leg raising test). Testing reflexes and feeling in the legs will be done for the same reason.
- Muscles. The muscles in the back and legs wil be tested. Tightness of the back muscles or the hamstring muscles at the back of the thigh will show that your child is trying to protect himself or herself from movements and positions that might be painful. Tenderness of the muscles will indicate a muscle injury, such as a strain.
- Balance, flexibility, coordination, and muscle strength. Other tests may be done to ensure that the back pain is not part of a bigger picture.
Imaging tests
Pediatrician or an orthopedic surgeon use a variety of imaging modalities to help them better pinpoint the source of your child’s back pain.
Imaging tests include:
- X-rays. X-rays provide images of dense structures, such as bones. X-rays of your child’s spine will show if there are fractures, displacements, or other problems within the bones.
- Computerized tomography (CT scan). This is a special x-ray technique that provides a three-dimensional image. It allows your doctor to see things that are not visible on two-dimensional x-rays, and is particularly helpful for understanding the complex anatomy of the spine.
- Magnetic resonance imaging (MRI). An MRI shows the body’s soft tissues. It can be used to see the spinal cord, nerve roots, disks, and other structures that can be very important in back pain.
- EOS imaging (3-D imaging system that scans your child standing up). EOS delivers a radiation dose that is two to three times less than a general computed radiography X-ray and 20 times less than basic computed tomography (CT) scans.
- Bone scan. A bone scan involves injecting a substance into a vein, then using a special camera to see where it is picked up. It can pinpoint inflammation, infections, tumors, and fractures. Since the anatomy of the spine is very complicated and since these disease processes are not always visible on x-ray, a bone scan can be very useful.
- Positron emission tomography (PET). PET scan can help your doctor understand more about how the body’s tissues and organs are functioning.
Laboratory tests
Blood tests, including the complete blood-cell count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), can be affected by the presence of inflammation or infection.
Back pain in children treatment
Back pain in children treatment involves treating the underlying cause of the back pain.
Most cases of back pain don’t require medical attention and can be treated with over-the-counter pain relief medication and self-care.
Most people prefer to take acetaminophen (paracetamol) or anti-inflammatory drugs such as ibuprofen.
Back pain in children prognosis
Many children who experience back pain will quickly heal and move on with their lives. For children who experienced an infection that caused the back pain, recovery is generally complete after treatment.
For children diagnosed with spine conditions — scoliosis, spondylolysis or disc herniation — that required surgery, ongoing clinical follow-up is encouraged.
- Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009;60(10):3072–3080.[↩]
- https://www.acr.org/[↩][↩]
- Cheung KM, Karppinen J, Chan D, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine (Phila Pa 1976). 2009;34(9):934–940.[↩]
- Acosta FL Jr, Galvez LF, Aryan HE, Ames CP. Recent advances: infections of the spine. Curr Infect Dis Rep. 2006;8(5):390–393.[↩][↩]