What is oligohydramnios
Oligohydramnios is a condition when you have too little amniotic fluid for gestational age 1. Amniotic fluid is the fluid that is contained in the amniotic sac and it surrounds your baby in your uterus (womb). Amniotic fluid is very important for your baby’s development. Oligohydramnios may occur with late pregnancies, ruptured membranes, placental dysfunction, or fetal abnormalities. Oligohydramnios is usually called isolated oligohydramnios when only the amniotic fluid was decreased at term without any other fetal or maternal abnormality such as intrauterine growth restriction (IUGR), fetal anomaly, and maternal hypertensive disease 2.
While in the womb, your baby floats in the amniotic fluid. Your baby stays in this fluid throughout your pregnancy. This helps protect your baby and allows them to move and kick during development. Amniotic fluid also helps your baby’s lungs, kidneys, and gastrointestinal tract grow. The amount of amniotic fluid is greatest at about 34 weeks (gestation) into the pregnancy, when it averages 800 mL. About 600 mL of amniotic fluid surrounds the baby at full term (40 weeks gestation).
The amniotic fluid constantly moves (circulates) as the baby swallows and “inhales” the fluid, and then releases it.
During pregnancy, amniotic fluid provides a cushion that protects the baby from injury and allows room for growth, movement and development. Amniotic fluid also keeps the umbilical cord from being compressed between the baby and the uterine wall. In addition, the amount of amniotic fluid reflects the baby’s urine output — a measure of a baby’s well-being.
The amniotic fluid helps:
- The developing baby to move in the womb, which allows for proper bone growth
- The lungs to develop properly
- Prevents pressure on the umbilical cord
- Keep a constant temperature around the baby, protecting from heat loss
- Protect the baby from outside injury by cushioning sudden blows or movements
Oligohydramnios can happen at any time during pregnancy, but it’s most common in the last trimester (last 3 months). The risk of having oligohydramnios increases for people who are at least 2 weeks past their due dates. This is because the amount of amniotic fluid usually decreases by that time. In general, the earlier it happens during pregnancy, the higher the risk to the baby.
Various factors can contribute to oligohydramnios in pregnancy, including:
- Your water breaking
- The placenta peeling away from the inner wall of the uterus — either partially or completely — before delivery (placental abruption)
- Certain health conditions in the mother, such as chronic high blood pressure
- Use of certain medications, such as angiotensin-converting enzyme (ACE) inhibitors
- Certain health conditions in the baby, such as restricted growth or a genetic disorder
If you have oligohydramnios (low amniotic fluid), what happens next will depend on the cause, severity, your baby’s gestational age, your health and your baby’s health.
If you have oligohydramnios (low amniotic fluid) and you’re 36 to 37 weeks pregnant, the safest treatment might be delivery. If you’re less than 36 weeks pregnant, your doctor will review your baby’s health, discuss why you might have oligohydramnios (low amniotic fluid) and recommend monitoring your pregnancy with fetal ultrasounds. He or she also might recommend drinking more fluids — especially if you’re dehydrated.
If you have oligohydramnios (low amniotic fluid) during labor, your doctor might consider a procedure in which fluid is placed in the amniotic sac (amnioinfusion). This is typically done during labor if there are fetal heart rate abnormalities. Amnioinfusion is done by introducing saline into the amniotic sac through a catheter placed in the cervix during labor.
Oligohydramnios (low amniotic fluid) during pregnancy is a serious condition. If you have any concerns about the amount of fluid around your baby, talk with your health care provider.
Fetal health can be seriously compromised by oligohydramnios, with complications such as pulmonary hypoplasia, meconium aspiration syndrome, fetal compression and, in cases of prolonged rupture of membranes, infections 3, 4. Women with oligohydramnios are more likely to have an infant with low birth weight 5, 6, 7. In terms of burden of care, higher rates of cesarean delivery for fetal distress and neonatal admission to the intensive care unit have also been associated with oligohydramnios 8, 3. Timely identification and treatment have been associated with improvement in some maternal and fetal/neonatal outcomes. When detected, clinical management of women with oligohydramnios can include amnioinfusion, early induction of labor and even cesarean delivery 9, 10.
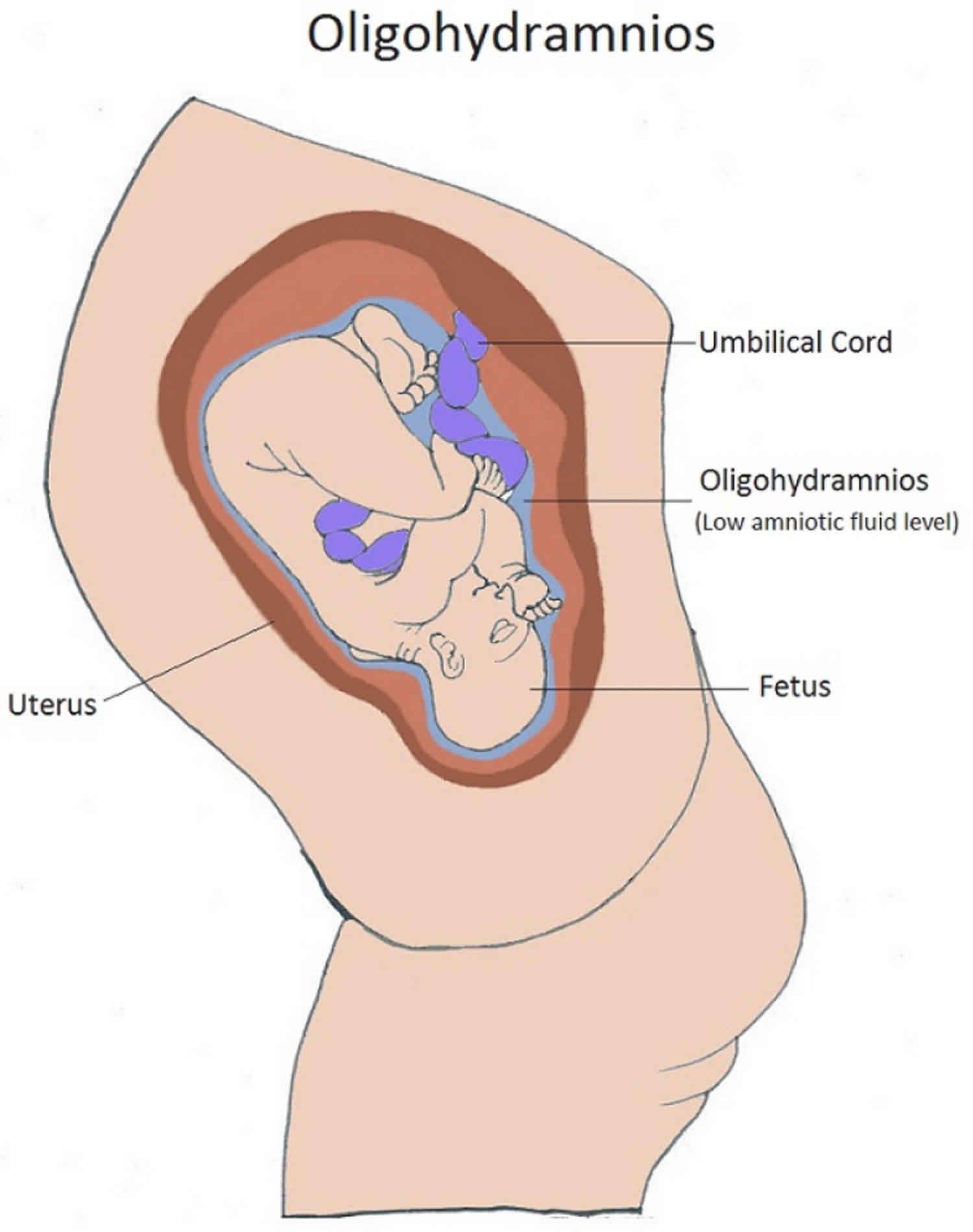
Figure 1. Amniotic fluid
How do you know if you have oligohydramnios?
If you notice that you are leaking fluid from your vagina, tell your health care provider. It may be a sign of oligohydramnios. Your provider watches out for other signs, such as if you’re not gaining enough weight or if the baby isn’t growing as fast as he should.
Your health care provider uses ultrasound to measure the amount of amniotic fluid. There are two ways to measure the fluid: amniotic fluid index (AFI) and maximum vertical pocket (MPV).
The amniotic fluid index (AFI) checks how deep the amniotic fluid is in four areas of your uterus. The amniotic fluid index (AFI) is an estimate of the amniotic fluid volume in a pregnant uterus. It is part of the fetal biophysical profile. These amounts are then added up. If your amniotic fluid index (AFI) is less than 5 centimeters, you have oligohydramnios.
The maximum vertical pocket (MPV) measures the deepest area of your uterus to check the amniotic fluid level. If your maximum vertical pocket (MPV) is less than 2 centimeters, you have oligohydramnios.
The deepest (maximal) vertical pocket (MPV) depth is considered a reliable method for assessing amniotic fluid volume on ultrasound 11. It is performed by assessing a pocket of a maximal depth of amniotic fluid which is free of an umbilical cord and fetal parts.
The usually accepted MPV values are:
- MPV <2 cm: indicative of oligohydramnios
- MPV 2-8 cm: normal but should be taken in the context of subjective volume
- MPV >8 cm: indicative of polyhydramnios (although some centers, particularly in Australia, New Zealand and the United Kingdom, use a cut off of >10 cm)
Ask your health provider if you have questions about these measurements.
Figure 2. Oligohydramnios ultrasound
Footnote: Gestation 23+6/40, transverse lie. Estimation of fetal weight <5th percentile and abdominal circumference (AC) on 15th percentile. Amniotic fluid index (AFI) is reduced at 2.5. An AFI < 5-8 is indicative of oligohydramnios. In this case there is also reduced amniotic fluid volume subjectively. The cause in this case was preterm premature rupture of membranes (PPROM).
Amniotic fluid
Amniotic fluid is the fluid that surrounds your baby in your uterus (womb) (Figure 1). It’s very important for your baby’s development.
During pregnancy, your uterus is filled with amniotic fluid.
Here’s what the amniotic fluid does:
- Cushions and protects your baby
- Keeps a steady temperature around your baby
- Helps your baby’s lungs grow and develop because your baby breathes in the fluid
- Helps your baby’s digestive system develop because your baby swallows the fluid
- Helps your baby’s muscles and bones develop because your baby can move around in the fluid
- Keeps the umbilical cord (the cord that carries food and oxygen from the placenta to your baby) from being squeezed
The amniotic sac (bag) inside the uterus holds your growing baby. It is filled with amniotic fluid. This sac forms about 12 days after getting pregnant.
In the early weeks of pregnancy, the amniotic fluid is mostly water that comes from your body. After about 20 weeks of pregnancy, your baby’s urine makes up most of the fluid. Amniotic fluid also contains nutrients, hormones (chemicals made by the body) and antibodies (cells in the body that fight off infection).
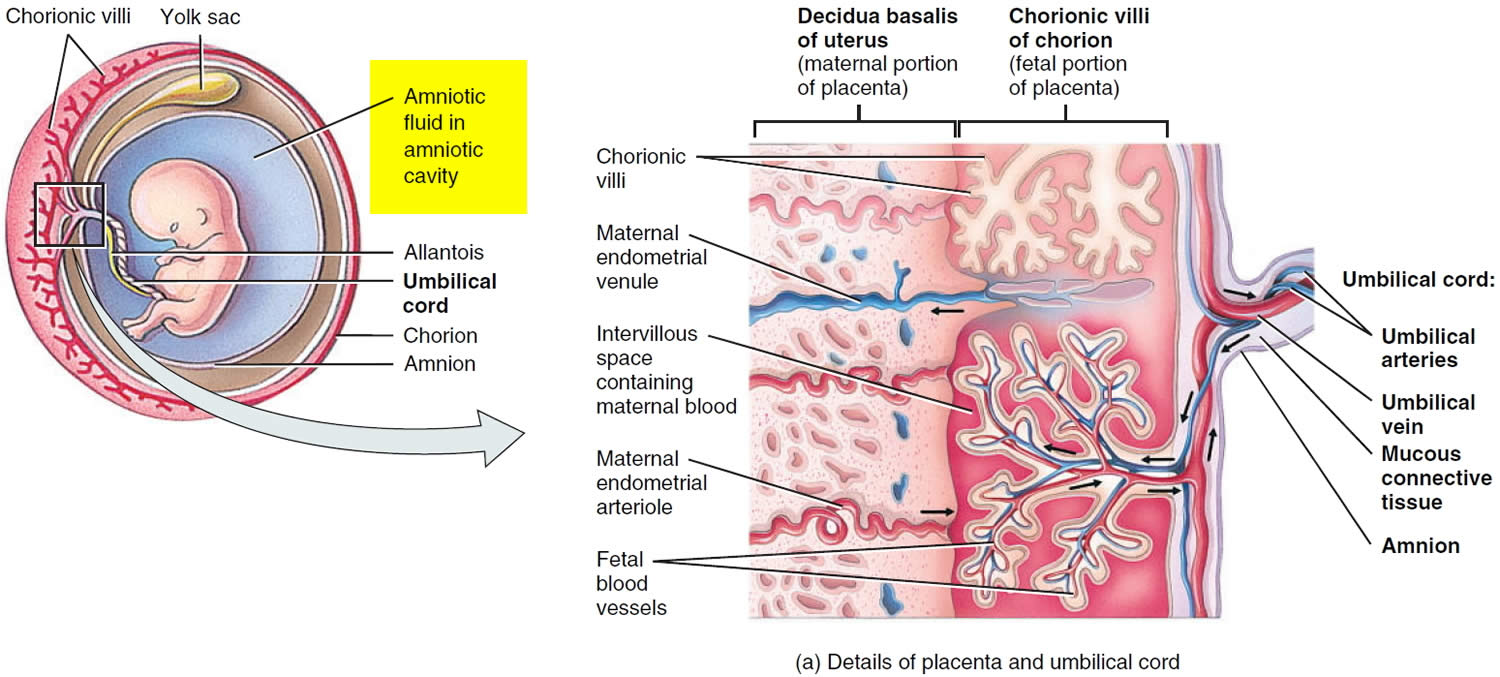
Figure 3. Amniotic fluid and sac
What is amniotic fluid index?
Amniotic fluid index or AFI is an estimate of the amniotic fluid volume in a pregnant uterus on ultrasound. The normal range for amniotic fluid volumes varies with gestational age.
Typical amniotic fluid index (AFI) values include 12, 13, 14:
- Amniotic fluid index (AFI) between 5-25 cm is considered normal; median AFI level is approximately 14 cm from week 20 to week 35, after which the amniotic fluid volume begins to reduce
- Amniotic fluid index (AFI) <5 cm is considered to be oligohydramnios
- Value changes with age: the 5th percentile for gestational ages is most often taken as the cut-off value, and this is around an AFI of 7 cm for second and third-trimester pregnancies; an AFI of 5 cm is two standard deviations from the mean
- Amniotic fluid index (AFI) >25 cm is considered to be polyhydramnios
How much amniotic fluid should there be?
The amount of amniotic fluid increases until about 36 weeks of pregnancy. At that time, it makes up about 1 quart (946 ml). After that, the amount of amniotic fluid usually begins to decrease.
Sometimes you can have too little or too much amniotic fluid. Too little fluid is called oligohydramnios. Too much fluid is called polyhydramnios. Either one can cause problems for a pregnant woman and her baby. Even with these conditions, though, most babies are born healthy.
Does the color of amniotic fluid mean anything?
Normal amniotic fluid is clear or tinted yellow. Fluid that looks green or brown usually means that the baby has passed his first bowel movement (meconium) while in the womb. Usually, the baby has his first bowel movement after birth.
If the baby passes meconium in the womb, it can get into his lungs through the amniotic fluid. This can cause serious breathing problems, called meconium aspiration syndrome, especially if the fluid is thick.
Some babies with meconium in the amniotic fluid may need treatment right away after birth to prevent breathing problems. Babies who appear healthy at birth may not need treatment, even if the amniotic fluid has meconium.
What is maximal vertical pocket?
The maximal vertical pocket (MVP) also called the deepest vertical pocket depth is considered a reliable method for assessing amniotic fluid volume on ultrasound 15, 16. The maximal vertical pocket (MVP) depth is performed by assessing a pocket of a maximal depth of amniotic fluid which is free of an umbilical cord and fetal parts 17.
The usually accepted maximal vertical pocket (MVP) values are 17:
- <2 cm: indicative of oligohydramnios
- 2-8 cm: normal but should be taken in the context of subjective volume
- >8 cm: indicative of polyhydramnios (although some centers, particularly in Australia, New Zealand and the United Kingdom, use a cut off of >10 cm)
What causes oligohydramnios
Sometimes the causes of oligohydramnios are not known. Some known causes are 18:
- Mother’s health problems, such as high blood pressure, preeclampsia, or preexisting diabetes (having too much sugar in the blood before pregnancy) (8% of all pregnancies)
- Certain medications, like those used to treat high blood pressure called ACE inhibitors and pain relievers called non-steroidal anti-inflammatory drugs (NSAIDs) and cocaine use. If you have high blood pressure, talk to your doctor before getting pregnant to make sure your blood pressure is under control.
- Post-term pregnancy – A pregnancy that goes 2 or more weeks past the due date. A full-term pregnancy lasts between 39 weeks, 0 days and 40 weeks, 6 days. Post-term pregnancy is when your baby is born after 42 weeks, 0 days. Post-term pregnancies, fetal growth restriction (5% of the second trimester and 20.5% of third-trimester diagnoses).
- Birth defects, especially ones that affect the baby’s kidneys, stomach, bladder, or urethra. Genitourinary tract abnormalities (renal agenesis, obstructive nephropathy) are associated with oligohydramnios and occur at an incidence of 3 to 7 per 1000 live births.
- Issues with the baby’s placenta, which supplies the baby with food and oxygen through the umbilical cord
- Having a baby who is growing too slowly
- Being pregnant with identical twins who share one placenta with twin to twin transfusion syndrome (oligohydramnios-polyhydramnios sequence).
- Placental causes. Placental causes of oligohydramnios include placenta abruption (8.6% of all oligohydramnios cases)
- Preterm premature rupture of membranes (PPROM) – When the amniotic sac breaks after 37 weeks of pregnancy but before labor starts. Preterm premature rupture of membranes (PPROM) alone accounts for greater than 37% of oligohydramnios cases diagnosed in the second and third trimesters.
- Idiopathic (unexplained). The majority of oligohydramnios cases, 50.7% diagnosed in the third trimester, are of unexplained cause and, typically, associated with better outcomes 19.
A helpful mnemonic for remembering some causes of oligohydramnios is DRIPPC 20:
- D: Demise and drugs (e.g. prostaglandin inhibitors [indomethacin])
- R: Renal abnormalities (decreased urine output)
- renal agenesis
- renal dysplasia
- posterior urethral valves
- polycystic kidneys
- multicystic dysplastic kidney
- urethral atresia
- I: Intrauterine Growth Restriction (IUGR), 80% may occur from decreased renal perfusion due to sparing effect
- P: Premature rupture of membranes
- premature rupture of membranes (PROM)
- preterm premature rupture of membranes (PPROM)
- P: Post-dates. Post dates fetus is when there is prolonged gestation when the fetus remains in-utero beyond 2 weeks beyond expected date of delivery (>42 weeks gestation).
- C: Chromosomal anomalies (especially if other anomalies are found). Chromosomal abnormalities (10% of oligohydramnios cases in the second trimester)
- Trisomy 18. Edwards syndrome, also known as trisomy 18 fetuses can have multiple anomalies in multiple systems
- Trisomy 13. Patau syndrome also known as trisomy 13 is considered the 3rd commonest autosomal trisomy.
- Triploidy. Triploidy is a rare lethal chromosomal (aneupliodic) abnormality caused by the presence of an entire extra chromosomal set.
Associations
- Potter Sequence
- Underlying fetal hypoxia and fetal cardiovascular compromise: from preferential flow to the fetal brain at the expense of diminished renal blood flow
- Twin pregnancy-related complications: twin to twin transfusion syndrome: in pump twin
- Maternal dehydration
About 4 out of 100 (4 percent) pregnant women have oligohydramnios. It can happen at any time during pregnancy, but it’s most common in the last trimester (last 3 months). It happens in about 12 out of 100 (12 percent) women whose pregnancies last about 2 weeks past their due dates. This is because the amount of amniotic fluid usually decreases by that time.
Oligohydramnios symptoms
Some of oligohydramnios symptoms may include:
- Fluid leaking from your vagina.
- Your uterus not growing as expected or your uterus is smaller than expected compared with how far along you are in your pregnancy
- Your baby’s movements slowing down or your baby isn’t moving around enough
Other signs of oligohydramnios can include:
- Your baby isn’t growing as fast as they should
- You’re not gaining enough weight
If you notice fluid leaking from your vagina, see your health care provider right away.
Oligohydramnios complications
If oligohydramnios happens in the first 2 trimesters (first 6 months) of pregnancy, it is more likely to cause serious problems than if it happens in the last trimester. These problems can be 21, 22:
- Birth defects – Problems with a baby’s body that are present at birth
- Miscarriage – When a baby dies in the womb before 20 weeks of pregnancy
- Premature birth – Birth before 37 weeks of pregnancy
- Stillbirth – When a baby dies in the womb after 20 weeks of pregnancy
- Infection if the amniotic sac is leaking
In general, babies who develop oligohydramnios after 23 to 24 weeks (6 months of pregnancy) usually don’t have breathing issues or other long-term problems.
If oligohydramnios happens in the third trimester of pregnancy, it can cause 21, 22:
- The baby to grow slowly
- Problems during labor and birth, such as the umbilical cord being squeezed. The umbilical cord carries food and oxygen from the placenta to the baby. If it’s squeezed, the baby doesn’t get enough food and oxygen.
- The baby to breathe their first bowel movement (meconium) into their lungs, which can cause breathing issues.
- Joint issues because the baby wasn’t able to move around enough
- A greater chance of needing a cesarean section (when your baby is born through a cut the doctor makes in your belly and uterus)
Getting early and regular prenatal care can help you have a healthy pregnancy and a full-term baby. Prenatal care is medical care you get during pregnancy. At each visit, your health care provider checks on you and your growing baby, including your amniotic fluid levels.
Call your doctor and go for your first prenatal care checkup as soon as you know you’re pregnant. And go to all your prenatal care checkups, even if you’re feeling fine.
Oligohydramnios diagnosis
Oligohydramnios may be discovered incidentally during routine ultrasonography and noted during antepartum surveillance for other conditions. The diagnosis may be prompted by a lag in sequential fundal height measurements (size less than that expected for the dates) or by fetal parts that are easily palpated through the maternal abdomen 23.
During ultrasonography of the fetal anatomy, normal-appearing fetal kidneys and fluid-filled bladder may be observed to rule out renal agenesis, cystic dysplasia, and ureteral obstruction. Check fetal growth to rule out intrauterine growth restriction (IUGR) leading to oliguria.
Other examinations
MRI and 3-dimensional (3D) ultrasonography are newer (and more expensive) modalities for accurately assessing the amniotic fluid volume 24.
Fetal MRI can complement ultrasonography by providing better visualization in the fetus when ultrasound may be limited, in cases such as severe maternal obesity. Although MRI may offer a larger field of view and better tissue contrast and not be limited by shadowing from osseous structures, it has a limited resolution when compared with ultrasonography and is less readily available and is more expensive 25.
In 35 women with healthy singleton pregnancies, rapid MRI-based projection hydrography measurement was found to be a better predictor of amniotic fluid volume than ultrasonography (in utero at 28-32 weeks’ gestation). For the ultrasound measurements, single deepest vertical pocket (SDVP) measurement related most closely to amniotic fluid volume, with amniotic fluid index (AFI) demonstrating a weaker relationship. Manual multisection planimetry (MSP)-based measurement of amniotic fluid volume was used as a proxy reference standard 24.
Oligohydramnios treatment
The management of oligohydramnios vary greatly depending on the underlying cause, the gestational age at diagnosis, your symptoms, and the severity of the oligohydramnios 1. Treatment will focus on keeping you pregnant for as long as it’s safe. This will enable your baby to continue to grow and develop before birth.
Oligohydramnios treatment may include the following:
- Drinking water. Drinking lots of water may help increase the amount of amniotic fluid.
- Resting. Your doctor may recommend less physical activity or going on bed rest.
- Monitoring. Your provider may want to see you more often. They may want to do ultrasounds weekly or more often to check the amount of amniotic fluid.
- Amnioinfusion. This is when the provider adds fluid by putting a saline solution (salty water) into the uterus through the cervix (the opening to the uterus that sits at the top of your vagina). You may need this if you’re in labor and your water has broken. It can help prevent some problems, such as the umbilical cord being squeezed. If the umbilical cord is squeezed, the baby doesn’t get enough food and oxygen.
- Medication. If you have diabetes or high blood pressure, your provider may treat those conditions. You may be given antibiotics to prevent infection if your amniotic sac has burst, or medication to help your baby’s lungs if the placenta isn’t working properly.
- Starting labor early. If the fluid gets too low or if your baby is having trouble staying healthy, your provider may recommend starting labor early to help prevent problems during labor and birth.
If you have a healthy pregnancy and get oligohydramnios near the end of your pregnancy, you probably don’t need treatment. Your doctor may want to see you more often. She may want to do ultrasounds weekly or more often to check the amount of amniotic fluid.
Sometimes amnioinfusion can help prevent problems in the baby. Amnioinfusion is when your doctor puts a saline solution (salty water) into the uterus through your cervix (the opening to the uterus that sits at the top of your vagina). This treatment can help prevent some problems, such as the umbilical cord being squeezed. If the umbilical cord is squeezed, the baby doesn’t get enough food and oxygen.
If the fluid gets too low or if your baby is having trouble staying healthy, your doctor may recommend starting labor early to help prevent problems during labor and birth. However, with regular prenatal care, chances are that your baby will be born healthy.
Drinking lots of water may help increase the amount of amniotic fluid. Your doctor may recommend less physical activity or going on bed rest.
Oligohydramnios prognosis
Prognosis of oligohydramnios vary greatly depending on the underlying cause, the gestational age at diagnosis, and the severity of oligohydramnios. Oligohydramnios is associated with higher rates of maternal hemorrhage, fetal malposition and cesarean delivery than in pregnancies without oligohydramnios 26. Higher rates of poor fetal or neonatal outcomes were also associated with oligohydramnios, including a 5-fold increase in stillbirths and a 3-fold increase in deaths among babies less than 28 days of age 26. The babies were also twice as likely to be born prematurely or to be low birth weight (weigh less than 2500 g). The babies from pregnancies complicated by oligohydramnios weighed on average 162 g less than those from pregnancies without oligohydramnios 26.
Diagnosis of oligohydramnios during the second trimester is more likely to be associated with fetal or maternal anomalies, whereas diagnosis in the third trimester is more likely to be of unexplained origin. In one study, the cause of oligohydramnios was unexplained in just 4% of second-trimester gestations, whereas 52% of those diagnosed in the third trimester were idiopathic. Only 10.2% of fetuses diagnosed in the second trimester survived, while the survival rate was 85.3% in those diagnosed in the third trimester 19.
In cases of oligohydramnios diagnosed in the second trimester, pulmonary hypoplasia is the most significant predictor of fetal mortality. The mortality rate of second-trimester oligohydramnios can be as high as 90%, with pulmonary hypoplasia accounting for 87% of those deaths. The most severe pulmonary hypoplasia occurs with oligohydramnios before or during 16 to 24 weeks gestational age, when the terminal sacs of the fetal lung are developing. Low amniotic fluid index (AFI) during the second and early third trimester also increases the likelihood of limb contractures and birth defects due to compression of fetal parts 19.
References- Keilman C, Shanks AL. Oligohydramnios. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562326
- Seol HJ, Kim HY, Cho GJ, Oh MJ. Hourly fetal urine production rate in isolated oligohydramnios at term. PLoS One. 2021 May 21;16(5):e0250659. doi: 10.1371/journal.pone.0250659
- Patel A, Patel HV. Role of amniotic fluid index in pregnancy outcome. 2015. pp. 1–12.
- Voxman EG, Tran S, Wing DA. Low amniotic fluid index as a predictor of adverse perinatal outcome. J Perinatol. 2002;22:282–285. doi: 10.1038/sj.jp.7210697
- Mathuriya G, Verma M, Rajpoot S. Comparative study of maternal and fetal outcome between low and normal amniotic fluid index at term. Int J Reprod contraception. Obstet Gynecol. 2017;6:640.
- Rabie N, Magann E, Steelman S, Ounpraseuth S. Oligohydramnios in complicated and uncomplicated pregnancy: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017;49:442–449. doi: 10.1002/uog.15929
- Madhavi K, Pc R, Professor A. Clinical study of oligohydramnios, mode of delivery and perinatal outcome. IOSR J Dent Med Sci. 2015;14:2279–2861.
- Locatelli A, Zagarella A, Toso L, Assi F, Ghidini A, Biffi A. Serial assessment of amniotic fluid index in uncomplicated term pregnancies: prognostic value of amniotic fluid reduction. J Matern Neonatal Med. 2004;15:233–236. doi: 10.1080/14767050410001668671
- Butt FT, Ahmed B. The role of antepartum transabdominal amnioinfusion in the management of oligohydramnios in pregnancy. J Matern Fetal Neonatal Med. 2011;24:453–457. doi: 10.3109/14767058.2010.497574
- Turhan NÖ, Atacan N. Antepartum prophylactic transabdominal amnioinfusion in preterm pregnancies complicated by oligohydramnios. Int J Gynecol Obstet. 2002;76:15–21. doi: 10.1016/S0020-7292(01)00504-5
- Magann EF, Chauhan SP, Doherty DA et-al. The evidence for abandoning the amniotic fluid index in favor of the single deepest pocket. Am J Perinatol. 2007;24 (9): 549-55. doi:10.1055/s-2007-986689
- Magann EF, Sanderson M, Martin JN, Chauhan S. The amniotic fluid index, single deepest pocket, and two-diameter pocket in normal human pregnancy. Am J Obstet Gynecol. 2000 Jun;182(6):1581-8. doi: 10.1067/mob.2000.107325
- Hallak M, Kirshon B, Smith EO, Cotton DB. Amniotic fluid index. Gestational age-specific values for normal human pregnancy. J Reprod Med. 1993 Nov;38(11):853-6.
- Porter TF, Dildy GA, Blanchard JR, Kochenour NK, Clark SL. Normal values for amniotic fluid index during uncomplicated twin pregnancy. Obstet Gynecol. 1996 May;87(5 Pt 1):699-702. doi: 10.1016/0029-7844(96)00006-3
- Magann EF, Chauhan SP, Doherty DA, Magann MI, Morrison JC. The evidence for abandoning the amniotic fluid index in favor of the single deepest pocket. Am J Perinatol. 2007 Oct;24(9):549-55. doi: 10.1055/s-2007-986689
- Magann, E.F., Chauhan, S.P., Washington, W., Whitworth, N.S., Martin, J.N., JR and Morrison, J.C. (2002), Ultrasound estimation of amniotic fluid volume using the largest vertical pocket containing umbilical cord: measure to or through the cord?. Ultrasound Obstet Gynecol, 20: 464-467. https://doi.org/10.1046/j.1469-0705.2002.00802.x
- Radswiki T, Haouimi A, Jones J, et al. Deepest vertical pocket method. Reference article, Radiopaedia.org https://doi.org/10.53347/rID-14752
- Peipert JF, Donnenfeld AE. Oligohydramnios: a review. Obstet Gynecol Surv. 1991 Jun;46(6):325-39. doi: 10.1097/00006254-199106000-00002
- Shipp, T.D., Bromley, B., Pauker, S., Frigoletto, F.D., Jr and Benacerraf, B.R. (1996), Outcome of singleton pregnancies with severe oligohydramnios in the second and third trimesters. Ultrasound Obstet Gynecol, 7: 108-113. https://doi.org/10.1046/j.1469-0705.1996.07020108.x
- Weissleder R, Wittenberg J, Harisinghani MM et-al. Primer of Diagnostic Imaging, Expert Consult- Online and Print. Mosby Inc. (2011) ISBN:0323065384
- Rabie, N., Magann, E., Steelman, S. and Ounpraseuth, S. (2017), Oligohydramnios in complicated and uncomplicated pregnancy: a systematic review and meta-analysis. Ultrasound Obstet Gynecol, 49: 442-449. https://doi.org/10.1002/uog.15929
- Oligohydramnios. https://www.marchofdimes.org/find-support/topics/planning-baby/oligohydramnios
- Vink J, Hickey K, Ghidini A, Deering S, Mora A, Poggi S. Earlier gestational age at ultrasound evaluation predicts adverse neonatal outcomes in the preterm appropriate-for-gestational-age fetus with idiopathic oligohydramnios. Am J Perinatol. 2009 Jan. 26(1):21-5.
- Hilliard NJ, Hawkes R, Patterson AJ, Graves MJ, Priest AN, Hunter S, et al. Amniotic fluid volume: Rapid MR-based assessment at 28-32 weeks gestation. Eur Radiol. 2016 Jan 20.
- Rubesova E, Barth RA. Advances in fetal imaging. Am J Perinatol. 2014 Aug. 31 (7):567-76.
- Figueroa L, McClure EM, Swanson J, Nathan R, Garces AL, Moore JL, Krebs NF, Hambidge KM, Bauserman M, Lokangaka A, Tshefu A, Mirza W, Saleem S, Naqvi F, Carlo WA, Chomba E, Liechty EA, Esamai F, Swanson D, Bose CL, Goldenberg RL. Oligohydramnios: a prospective study of fetal, neonatal and maternal outcomes in low-middle income countries. Reprod Health. 2020 Jan 30;17(1):19. doi: 10.1186/s12978-020-0854-y