What is preterm labor
Preterm labor is labor that happens before the 37th week of pregnancy 1. Preterm labor is further subcategorized into early and late preterm. Early preterm is when the baby is born before 33 weeks, and late preterm is when a baby is born between 34 and 36 weeks 2. About 8 out of 100 babies will be born prematurely. Labor is when regular contractions lead to opening up of the cervix (neck of the womb). This normally occurs at between 37 and 42 weeks of pregnancy. If it occurs before 37 weeks, it is known as premature labor. Very premature birth is much less common, with fewer than one in 100 babies being born at between 22 and 28 weeks of pregnancy. In the United States, approximately 12% of all live births occur before term, and preterm labor preceded approximately 50% of these preterm births (birth before 37 weeks’ gestation) 3, 4.
Preterm and premature mean the same thing — early. Preterm labor is labor that begins early, before 37 weeks of pregnancy. Labor is the process your body goes through to give birth to your baby. Preterm labor can lead to premature birth. Premature birth is when your baby is born early, before 37 weeks of pregnancy. Your baby needs about 40 weeks in the womb to grow and develop before birth.
Babies born before 37 weeks of pregnancy are called premature. Premature babies can have serious health problems at birth and later in life. About 1 in 10 babies is born prematurely each year in the United States. Although the causes of preterm labor are not well understood, preterm births (premature birth) account for approximately 70% of neonatal deaths and 36% of infant deaths as well as 25–50% of cases of long-term neurologic impairment in children 5, 6, 7.
- If you believe you are having preterm labor, get medical help right away. If in doubt, get checked early.
- Don’t worry about mistaking false labor for the real thing. Everyone will be pleased if it’s a false alarm.
If your preterm contractions result in preterm labor, your baby will be born early. The earlier premature birth happens, the greater the health risks for your baby. Many premature babies (preemies) need special care in the neonatal intensive care unit. Preemies can also have long-term mental and physical disabilities.
While the specific cause of preterm labor often isn’t clear, certain risk factors may up the odds of early labor. But, preterm labor can also occur in pregnant women with no known risk factors. Still, it’s a good idea to know if you’re at risk of preterm labor and how you might help prevent it.
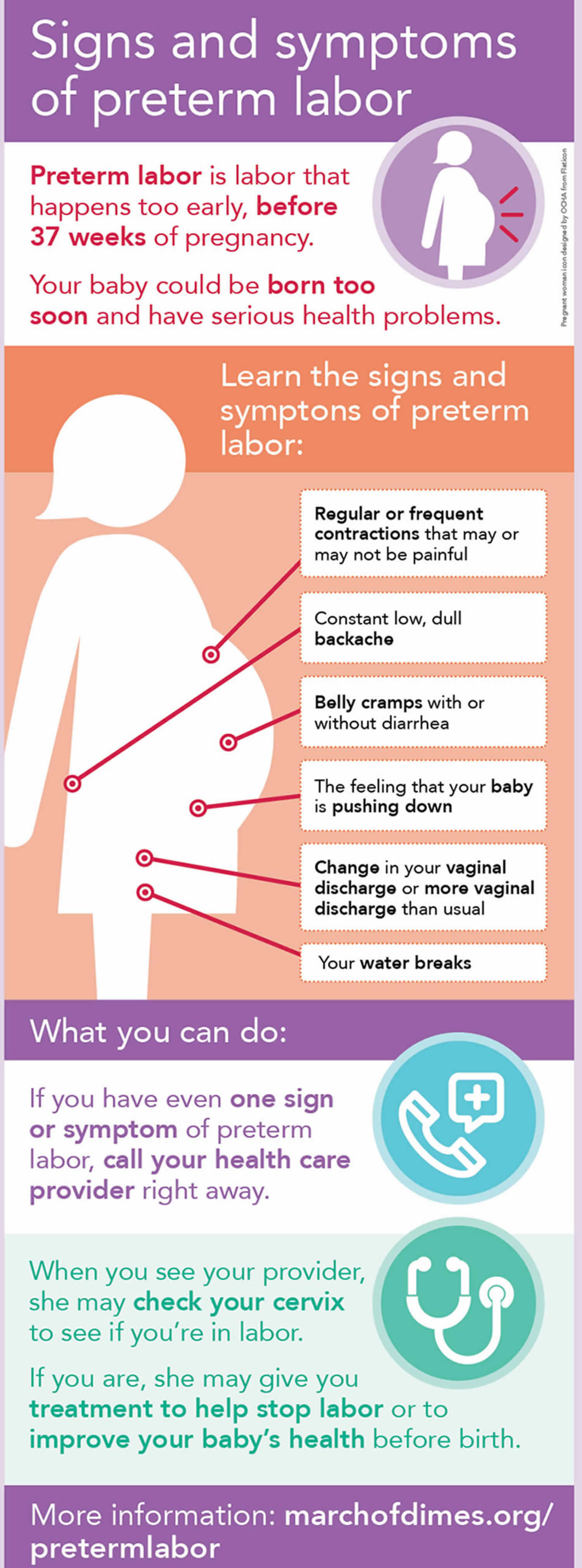
Signs of preterm labor
The signs of preterm labor can be similar to the signs of labor that starts at full term, and may include:
- Regular or frequent contractions that make your belly tighten like a fist. The contractions may or may not be painful.
- Period-type pains
- A “show” (when the plug of mucus that has sealed the cervix during pregnancy comes away and out of the vagina)
- Change in your vaginal discharge (watery, mucus or bloody) or more vaginal discharge than usual
- Breaking of the waters (rupture of membranes) – this can be a gush or a trickle
- Constant low, dull backache
- Pressure in your pelvis or lower belly, like your baby is pushing down
- Belly cramps with or without diarrhea
If you think your labor (you are having regular, painful tightenings or you think your waters have broken) might be starting and you’re less than 37 weeks pregnant, it is important that you call your doctor or hospital maternity unit straight away. You are likely to be asked to come in. They’ll need to check you and your baby to find out whether you’re in labor, and discuss your care choices with you.
Your doctor or midwife will ask whether you have had a premature birth in a previous pregnancy. You will also be asked about your general health, whether you have had any abdominal pain, tightenings or bleeding, and whether you think your waters have broken.
They’ll offer checks, tests and monitoring to find out whether:
- your waters have broken
- you’re in labor
- you have an infection
You will have a check-up that may include:
- a general examination and a check of your temperature, pulse and blood pressure
- a vaginal examination, blood test, urine test and cardiotocography to record contractions and your baby’s heartbeat
- an examination of your abdomen
- blood sample to check for signs of infection
- urine sample to test for signs of infection
You may also be offered an ultrasound scan to check your baby’s wellbeing and which way round he or she is lying.
The start of labor is usually diagnosed by vaginal examination:
- Your doctor or midwife will use a speculum (an instrument used to separate the walls of the vagina) to see whether the cervix is changing in preparation for labor or has already opened up.
- Your doctor or midwife will also be able to see whether there is fluid leaking, which may indicate that your waters have broken. Sometimes the waters break before 37 weeks but labor doesn’t start.
- A vaginal swab may be taken to check for infection.
- Another type of swab called fetal fibronectin may be taken from the top of the vagina, if you are at between 24 and 34 weeks of pregnancy. This test helps to see whether you are likely to go into labor soon or not:
- Most women who are suspected of being in premature labor have a negative swab. This is very reassuring because fewer than one in 100 women with a negative test will go into labor within the next 2 weeks.
- A positive swab means that there is an increased chance you may go into labor. One in five women who have a positive swab go into labor within 10 days.
The swab will be less accurate if you have any bleeding, if your waters have broken or if you have had sexual intercourse in the previous 24 hours.
If labor is not confirmed or if you have a negative fetal fibronectin swab, you should be able to go home if you are well and there are no concerns for you or your baby.
If labor is suspected, you will be advised to stay in hospital. You may be offered:
- A course of two to four corticosteroids injections usually over a 24–48 hour period to help with your baby’s development and reduce the chance of problems caused by being born early (unless you have already received steroids in this pregnancy).
- A course of antibiotics if it is confirmed that your waters have broken, to reduce the risk of an infection getting into the womb.
- An opportunity to talk to one of the neonatal team about the care that your baby is likely to receive, if born early. You and your partner may also wish to visit the neonatal unit.
- Medication (tablets or through a drip) to try to stop labor, if your waters have not broken and there are no concerns about you or your baby. This is only advised in the following circumstances:
- while you are having your course of corticosteroids
- if you need to be transferred to a hospital where there is a neonatal intensive care unit, which could be some distance away; this is particularly the case if you are less than 32 weeks pregnant.
- These medications are not routinely recommended for women having twins or triplets because it is not clear that they are beneficial in that situation.
- Treatment with magnesium sulfate, through a drip in your arm. This would be considered if you are less than 30 weeks pregnant and likely to give birth within the next 24 hours. This treatment reduces the chance of complications for your baby, in particular cerebral palsy. You may experience minor side effects such as flushing and nausea. If you are advised to have this treatment, your doctor will discuss it fully with you.
Planned premature labor
In some cases, preterm labor is planned and induced because it’s safer for the baby to be born sooner rather than later.
This could be because of a health condition in the mother, such as pre-eclampsia, or in the baby. Your midwife and doctor will discuss with you the benefits and risks of continuing with the pregnancy versus your baby being born premature.
You can still make a birth plan, and discuss your wishes with your birth partner, midwife and doctor.
Can I reduce my risk for preterm labor and premature birth?
Yes, you may be able to reduce your risk for early labor and premature birth. Some risk factors are things you can’t change, like having a premature birth in a previous pregnancy. Others are things you can do something about, like quitting smoking.
Here’s what you can do to reduce your risk for preterm labor and premature birth:
- Get to a healthy weight before pregnancy and gain the right amount of weight during pregnancy. Talk to your doctor about the right amount of weight for you before and during pregnancy.
- Don’t smoke, drink alcohol, use street drugs or abuse prescription drugs. Ask your doctor about programs that can help you quit.
- Go to your first prenatal care checkup as soon as you think you’re pregnant. During pregnancy, go to all your prenatal care checkups, even if you’re feeling fine. Prenatal care helps your doctor make sure you and your baby are healthy.
- Get treated for chronic health conditions, like high blood pressure, diabetes, depression and thyroid problems. Depression is a medical condition in which strong feelings of sadness last for a long time and interfere with your daily life. It needs treatment to get better. The thyroid is a gland in your neck that makes hormones that help your body store and use energy from food.
- Protect yourself from infections. Talk to your doctor about vaccinations that can help protect you from certain infections. Wash your hands with soap and water after using the bathroom or blowing your nose. Don’t eat raw meat, fish or eggs. Have safe sex. Don’t touch cat poop.
- Reduce your stress. Eat healthy foods and do something active every day. Ask family and friends for help around the house or taking care of other children. Get help if your partner abuses you. Talk to your boss about how to lower your stress at work.
- Wait at least 18 months between giving birth and getting pregnant again. Use birth control until you’re ready to get pregnant again. If you’re older than 35 or you’ve had a miscarriage or stillbirth, talk to your doctor about how long to wait between pregnancies. Miscarriage is the death of a baby in the womb before 20 weeks of pregnancy. Stillbirth is the death of a baby in the womb after 20 weeks of pregnancy.
What are the risks of preterm birth?
Babies born before full term (before 37 weeks) are vulnerable to problems associated with premature birth. The earlier in the pregnancy a baby is born, the more vulnerable they are. Premature babies have an increased risk of health problems, particularly with breathing, feeding and infection. The earlier your baby is born, the more likely he or she is to have these problems and your baby may need to be looked after in a neonatal unit. However, more than eight out of ten premature babies born after 28 weeks survive and only a small number will have serious long-term disability. Many survivors (as children) who have long-term health problems still rate their quality of life as being good.
Your goal is to get as close to term (40 weeks) as you can before giving birth. The closer you get to term, the greater your chances of having a healthy baby. Work with your doctor or obstetrician. Together you can take steps to keep you from giving birth too early.
Babies are considered ‘viable’ at 24 weeks of pregnancy – this means it’s possible for them to survive being born at this stage. If you give birth before 24 weeks of pregnancy, it is sadly much less likely that your baby will survive. Babies who do survive after such a premature birth often have serious health problems. The possible treatment and outcomes for your baby in your individual situation will be discussed with you.
Premature baby is at risk of a variety of problems, such as:
- not breastfeeding well;
- having immature lungs, and not being able to breathe on their own;
- bleeding in the brain;
- life-threatening infections;
- jaundice;
- inflammation of the bowel;
- long-term health problems, such as cerebral palsy; or
- dying.
Babies born this early need special care in a hospital with specialist facilities for premature babies. This is called a neonatal unit. They may have health and development problems because they haven’t fully developed in the womb.
If your baby is likely to be delivered early, you should be admitted to a hospital with a neonatal unit.
Not all hospitals have facilities for the care of very premature babies, so it may be necessary to transfer you and your baby to another unit, ideally before delivery (if time permits) or immediately afterwards.
Twins and multiples
Twins and triplets are often born prematurely. The average delivery date for twins is 37 weeks, and 33 weeks for triplets.
If you have any reason to think that your labor may be starting early, contact your hospital straight away.
What causes preterm labor?
For most women, the cause of preterm labor is not found. It is thought that a number of factors, sometimes involving infection, can bring about a change in the cervix that causes labor to start.
However, there are certain factors that increase your risk of preterm labor.
These three risk factors make you most likely to have preterm labor and premature birth (give birth early) 8:
- You’ve had a premature baby in the past.
- You’re pregnant with multiples (twins, triplets or more).
- You have problems with your uterus or cervix now or you’ve had them in the past. Your uterus (also called the womb) is where your baby grows inside you.
Medical risk factors before pregnancy for preterm labor and premature birth 8:
- Being underweight or overweight before pregnancy. This can include having an eating disorder, like anorexia or bulimia.
- Having a family history of premature birth. This means someone in your family (like your mother, grandmother or sister) has had a premature baby. If you were born prematurely, you’re more likely than others to give birth early.
- Getting pregnant again too soon after having a baby. For most women it’s best to wait at least 18 months before getting pregnant again. Talk to your provider about the right amount of time for you.
Medical risk factors during pregnancy for preterm labor and premature birth 8:
Having certain health conditions during pregnancy can increase your risk for preterm labor and premature birth, including:
- Connective tissue disorders, like Ehlers-Danlos syndromes and vascular Ehlers-Danlos syndrome. Connective tissue is tissue that surrounds and supports other tissues and organs. Ehlers-Danlos syndrome can cause joints to be loose and easy to dislocate; skin to be thin and easily stretched and bruised; and blood vessels to be fragile and small. It also can affect your uterus and intestines. Vascular Ehlers-Danlos syndrome is the most serious kind of Ehlers-Danlos syndrome because it can cause arteries and organs (like the uterus) to rupture (burst). Ehlers-Danlos syndromes and vascular Ehlers-Danlos syndrome are genetic conditions that can be passed from parent to child through genes.
- Diabetes. Diabetes is when your body has too much sugar (called glucose) in your blood.
- High blood pressure and preeclampsia. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. This can stress your heart and cause problems during pregnancy. Preeclampsia is a kind of high blood pressure some women during or right after pregnancy. If not treated, it can cause serious problems and even death.
- Infections, including sexually transmitted infections (also called STIs) and infections of the uterus, urinary tract or vagina
- Intrahepatic cholestasis of pregnancy. Intrahepatic cholestasis is the most common liver condition that happens during pregnancy.
- Thrombophilias. These are conditions that increase your risk of making abnormal blood clots.
Other medical risk factors during pregnancy include:
- Getting late or no prenatal care. Prenatal care is medical care you get during pregnancy.
- Not gaining enough weight during pregnancy. This can include having an eating disorder, like anorexia or bulimia.
- Bleeding from the vagina in the second or third trimester
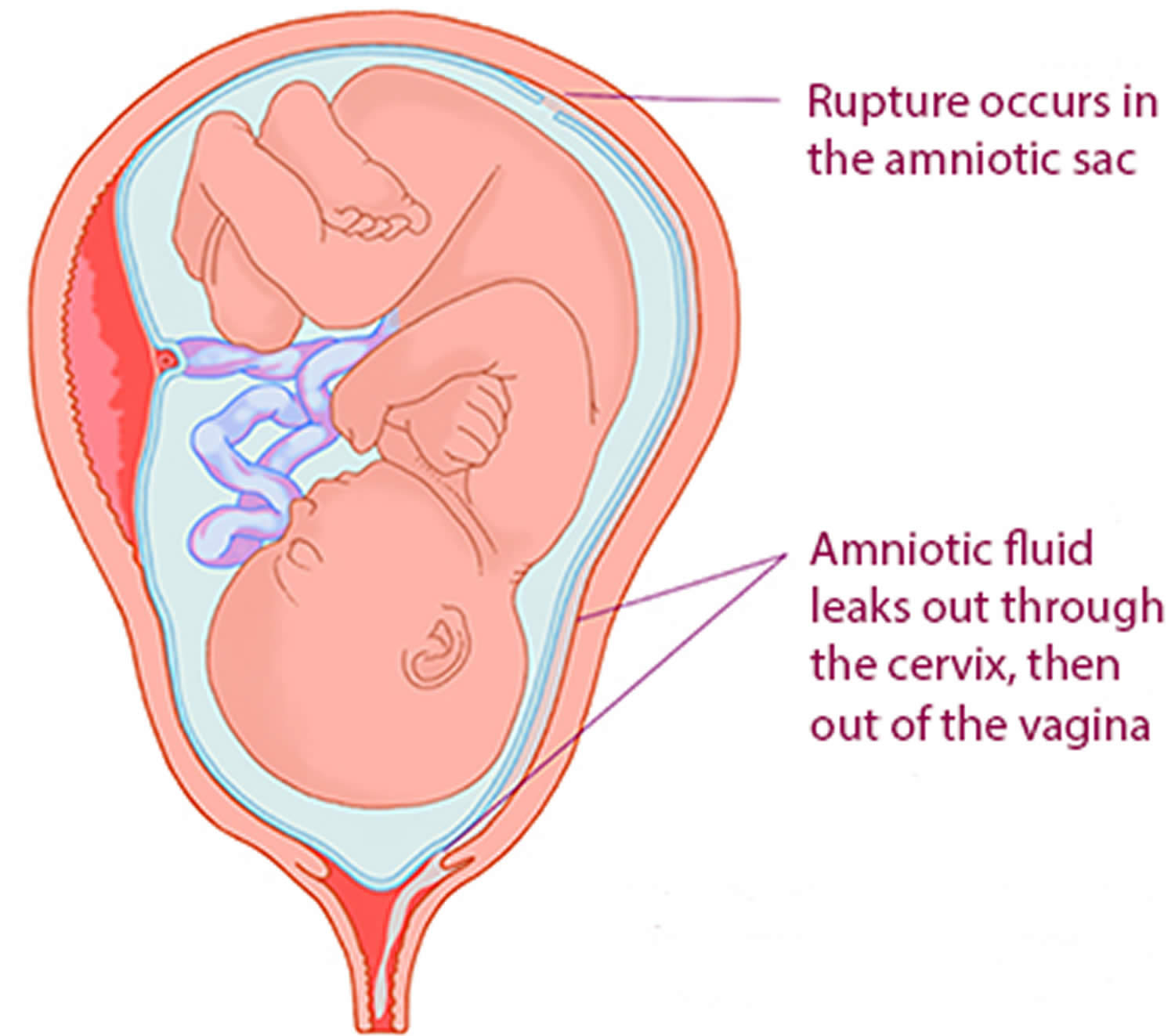
- Preterm premature rupture of the membranes (also called PPROM). Premature rupture of membranes (also called PROM) is when the amniotic sac around your baby breaks (your water breaks) before labor starts. PPROM is when this happens before 37 weeks of pregnancy. If you have any fluid leaking from your vagina, call your provider and go to the hospital.
- Being pregnant after in vitro fertilization (also called IVF). IVF is a fertility treatment used to help women get pregnant.
- Being pregnant with a baby who has certain birth defects, like heart defects or spina bifida. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works. Spina bifida is a birth defect of the spine.
Risk factors in your everyday life for preterm labor and premature birth:
- Smoking, drinking alcohol, using street drugs or abusing prescription drugs.
- Having a lot of stress in your life.
- Low socioeconomic status. Low socioeconomic status is a combination of things like your education, your job and your income (how much money you make).
- Domestic violence. This is when your partner hurts or abuses you. It includes physical, sexual and emotional abuse.
- Working long hours or having to stand a lot
- Exposure to air pollution, lead, radiation and chemicals in things like paint, plastics and secondhand smoke. Secondhand smoke is smoke from someone else’s cigarette, cigar or pipe.
- Age and race. Being younger than 17 or older than 35 makes you more likely than other women to give birth early. In the United States, black women are more likely to give birth early. Almost 17 percent of black babies are born prematurely each year. Just more than 10 percent of American Indian/Alaska Native and Hispanic babies are born early, and less than 10 percent of white and Asian babies 9. Experts don’t know why race plays a role in premature birth; researchers are working to learn more about it.
Having your baby early means that you are at an increased risk of having a premature birth in a future pregnancy. However, you are still likely to have a baby born at more than 37 weeks next time.
You will be advised to be under the care of a consultant obstetrician who will discuss with you a plan for your pregnancy. This will depend on your individual situation and on whether a cause for your early delivery, such as infection, was found.
Risk factors for preterm labor
Preterm labor can affect any pregnancy and many women who have preterm labor have no known risk factors. Many factors have been associated with an increased risk of preterm labor, however, including:
- Previous preterm labor or premature birth, particularly in the most recent pregnancy or in more than one previous pregnancy
- Pregnancy with twins, triplets or other multiples
- Certain problems with the uterus, cervix or placenta
- A lack of prenatal medical care
- Smoking cigarettes or using illicit drugs during pregnancy
- Certain infections, particularly of the genital tract, such as urinary tract infections or vaginal infections (e.g. bacterial vaginosis)
- Some chronic conditions, such as high blood pressure, diabetes or clotting disorders
- Being underweight or overweight before pregnancy, or gaining too little or too much weight during pregnancy
- Stressful life events, such as the death of a loved one
- Red blood cell deficiency (anemia), particularly during early pregnancy
- Too much amniotic fluid (polyhydramnios)
- Pregnancy complications, such as preeclampsia
- Vaginal bleeding during pregnancy
- Presence of a fetal birth defect
- Little or no prenatal care
- An interval of less than six months since the last pregnancy
- Stress
- Being under 17 or over 35 years old
Also, having a short cervical length or the presence of fetal fibronectin — a substance that acts like a glue between the fetal sac and the lining of the uterus — in your vaginal discharge has been linked to an increased risk of preterm labor.
While some past research suggested that gum disease might be linked with premature birth, treatment of periodontal disease during pregnancy hasn’t been proved to reduce the risk of premature birth.
Can preterm labor be prevented?
In some circumstances, particularly if you have had a baby born prematurely or a late miscarriage in the past, you may be offered vaginal scans in pregnancy to measure the length of your cervix or you may be advised to have a suture (stitch) put around it to prevent it opening early.
Cervical cerclage (cervical suture)
A cervical suture also known as cervical cerclage, is an operation where a suture (stitch) is placed around the cervix (neck of the womb) before or during pregnancy. Cervical cerclage is usually done at between 12 and 24 weeks of pregnancy. Cervical cerclage has been used to help correct structural defects or cervical weakening in high-risk women with a shortened cervix. Studies have shown that cervical suture is associated with a decrease in preterm delivery and in perinatal death when used in women with a prior preterm delivery and a cervical length of 25 mm or less 10. Although there are no randomized trials comparing cervical cerclage with progesterone, a meta-analysis of several studies that evaluated the methods separately suggests that both treatments are beneficial 11. There is no evidence that they are more effective when used together 11. The benefit of cerclage in women with a short cervix but no history of a preterm delivery is uncertain. Cerclage is not recommended for multiple gestation pregnancies and has been associated with a twofold increased risk of preterm delivery in twin pregnancies 12.
A cervical suture is sometimes recommended for women who are thought to have a high chance of a late miscarriage or of going into preterm labor. The purpose of the suture is to reduce the risk of your baby being born early. Premature babies have an increased risk of short- and long-term health problems.
The exact cause of preterm labor or late miscarriages is not clear, but they may be caused by changes in the cervix such as shortening and opening. A cervical suture helps to keep the cervix long and closed, thereby reducing the risk of premature birth or late miscarriage.
Insertion of the suture takes place in an operating theater. You may have a spinal anesthetic where you will stay awake but will be numb from the waist down or you may be given a general anesthetic where you will be asleep. Your team will advise which would be the best option for you.
You will be advised not to eat or drink for 4–6 hours before the operation. In the operating theater, your legs will be put in supports and sterile covers will be used to keep the operating area clean. The doctor will then insert a speculum (a plastic or metal instrument used to separate the walls of the vagina to show or reach the cervix) into the vagina and put the suture around the cervix. The operation should take less than 30 minute.
Afterwards, you may be given antibiotics to help prevent infection and you will be offered medication to ease any discomfort. You may also have a tube (catheter) inserted into your bladder that will be removed once the anesthetic has worn off.
You are likely to be able to go home the same day although you may be advised to stay in hospital longer.
After the operation, you will usually have some bleeding from the vagina, which should change to brown in color after a day or two. You may have a rise in temperature that should settle without treatment.
Once you recover from the operation, you can carry on as normal for the rest of your pregnancy. Resting in bed is not normally recommended. Sexual intercourse may be continued when you feel comfortable to do so. Your doctor can advise you about the activities you can do and those best avoided during the first few days after the procedure.
Are cervical sutures sometimes inserted through the abdomen?
Yes, if a vaginal cervical suture has not worked in the past or it is not possible to insert a vaginal suture. This would involve an operation through your abdomen and is called a ‘transabdominal cerclage’. It is done either before you become pregnant again or in early pregnancy. Such a suture is not removed and your baby would be born by caesarean section.
When might a cervical suture be advised?
You may be in one of the following situations:
- If you have had one or two late miscarriages or premature births (before 34 weeks), you may be offered ultrasound scans between 14 and 24 weeks of pregnancy to measure the length of your cervix. If the scans show that it has shortened to less than 25 mm, you may be advised to have a cervical suture.
- If you have suffered three or more late miscarriages or three or more premature births you may be advised to have a cervical suture inserted at about 12–14 weeks of pregnancy.
During pregnancy it is sometimes noticed during a vaginal examination or a routine scan that the cervix has started to open up. Depending on your circumstances, you may be offered a suture called a rescue suture. If you are in this situation, a senior obstetrician will discuss with you the risks and benefits of having a rescue suture.
Are there situations when a cervical suture would not be advised?
Sometimes a cervical suture is not advised. It would not normally improve the outcome for your baby/babies and may carry risks to you in the following circumstances:
- you are more than 24 weeks pregnant
- you are carrying twins or triplets
- your womb is an abnormal shape
- an ultrasound scan done for another reason happens to show that you have a short cervix
- you have had treatment to the cervix for an abnormal smear.
If a suture is not the right option for you, you will still be closely monitored. This may include regular vaginal ultrasound scans to measure the length of your cervix until 24 weeks of pregnancy. If the cervix is shortened, you may be offered corticosteroid injections after 23 weeks to increase the chance of your baby surviving if born early.
Are there situations when a cervical suture would not be put in?
Yes. A cervical suture would not be put in if:
- you are already in labor or your waters have broken
- you have signs of infection in your womb
- you have vaginal bleeding
- there are concerns about your baby’s wellbeing.
Are there any risks in having a cervical suture?
There is a small risk that your bladder or cervix may be damaged at the time of the operation. Rarely, your membranes may be ruptured. The risk of complications is higher if you have a rescue suture and this will be discussed with you before the operation.
A planned cervical suture does not increase your risk of infection, miscarriage, or premature labor. It does not increase your risk of having to be started off in labor (be induced) or needing a caesarean section.
Is there anything I should look out for?
If you experience any of the following symptoms, you should contact your maternity unit:
- contractions or cramping
- vaginal bleeding
- your waters breaking
- smelly vaginal discharge.
How and when will the suture be taken out?
Your suture will be taken out at the hospital. This will normally happen at around 36–37 weeks of pregnancy, unless you go into labor before then.
You will not normally need an anesthetic. A speculum is inserted into your vagina and the suture is cut and removed. It usually takes just a few minutes.
You may have a small amount of bleeding afterwards. Any red bleeding should settle within 24 hours but you may have a brown discharge for longer. If you have any concerns, tell your midwife or doctor.
If you go into labor with the cervical suture in place, it is very important to have it removed promptly to prevent damage to your cervix. If you think you are in labor, contact your maternity unit straight away.
If your waters break early but you are not in labor, the stitch will usually be removed because of the increased risk of infection. The timing of this will be decided by the team looking after you.
Progesterone therapy
In women with single gestation pregnancy and a history of spontaneous preterm delivery, antenatal progesterone therapy is the most effective strategy to decrease the risk of a recurrent preterm delivery 13. Progesterone supplementation is beneficial in these women starting at 16 to 24 weeks gestation and continuing through 34 weeks gestation 14, 15, 16, 17. The U.S. Food and Drug Administration (FDA) has approved hydroxyprogesterone caproate (Makena), 250 mg intramuscularly, as weekly injections 15, 18. Vaginal progesterone can be used in women with no history of spontaneous preterm delivery if they have a cervical length of 20 mm or less before 24 weeks gestation 13. In a randomized placebo-controlled trial, treatment with vaginal micronized progesterone, 200 mcg daily, was associated with a 44% reduction in spontaneous preterm delivery in asymptomatic women with a cervical length of 15 mm or less at 20 to 25 weeks gestation 16. Progesterone is not beneficial in multiple gestation pregnancies.
Preterm labor complications
Many women diagnosed with preterm labor deliver at or near term. However, there are no medications or surgical procedures to stop preterm labor, once it has started. In some cases, preterm labor associated with problems such as an infection or smoking can be managed by treating the infection or quitting smoking.
Preterm labor could lead to premature birth. This can pose a number of health concerns, such as low birth weight, breathing difficulties, underdeveloped organs and vision problems. Children who are born prematurely also have a higher risk of learning disabilities and behavioral problems.
With improved obstetric and neonatal care, the rate of complications in preterm births has decreased. With patient-specific education and follow up, the long-term complications and disability have improved 2.
Maternal complications
Preterm labor has been associated with an increased risk for cardiovascular death and disease, typically years after the delivery due to unclear reasons 2.
Infant complications
Preterm labor and delivery are associated with the impaired neurodevelopmental outcome which includes impaired cognitive abilities, motor deficits, cerebral palsy, and vision and hearing losses. These risks increase with decreasing gestational age. Behavioral issues such as anxiety, depression, autism spectrum disorders, and ADHD also associate to preterm labor.
Neonatal complications
These include necrotizing enterocolitis, intraventricular hemorrhage, bronchopulmonary dysplasia, retinopathy of immaturity, weak growth, and the presence of congenital anomalies.
Causes of premature birth
There are many causes of premature birth. Most occur spontaneously, however on occasions a mother or baby may necessitate an early induction of labor or caesarean birth. This can occur for medical or non-medical reasons.
Common reasons for preterm birth can be associated with different factors including medical and pregnancy; social, personal and economic; and behavioral.
Medical and Pregnancy
Cervical incompetence: This occurs when a weak cervix cannot support the weight of the uterus and begins to dilate (widen) and efface (thin) before pregnancy has reached term. Occasionally women diagnosed with an incompetent cervix may undergo a procedure in early stages of pregnancy called a cerclage. This involves placing a stitch in the cervix to prevent it opening up too soon and removing the stitch when nearing term.
Multiple births: Occurs when more than one fetus is carried in a single pregnancy. Twins and other multiple births are often induced early if labor is not spontaneous. Around 50% of twin pregnancies will be born before 37 weeks and a very high percentage of higher order multiples will be born prematurely.
Placental Accreta: Placenta accreta is a general term to describe a serious complication of pregnancy when part of the placenta, or entire placenta invades and is inseparable from the uterine wall causing severe blood loss after delivery. After giving birth the placenta should separate completely from the uterus. If part or all of the placenta remains attached it is called placenta accreta. It’s also possible for the placenta to invade the muscles of the uterus (placenta increta) or grow through the uterine wall, sometimes extending to nearby organs (placenta percreta).
Placenta Previa: A complication of pregnancy where the placenta has attached to the uterine wall close to or over the opening of the cervix. The most common complication of placenta Previa is bleeding leading to an increased risk of slow foetal growth and premature birth. Almost all babies are delivered via caesarean birth as the increased risk of severe bleeding associated with a vaginal birth can be life threatening. A woman is also at increased risk of having further premature births if this has occurred in previous pregnancies.
Placental abruption: A complication of pregnancy, where the placenta separates from the wall of the uterus. It is the most common cause of late pregnancy bleeding and if the separation is severe can contribute to fetal and maternal death. Direct trauma to the uterus is a known cause, and risk factors may be multiple pregnancies, smoking and high blood pressure including preeclampsia.
Placental insufficiency: This condition can prevent the baby from gaining essential nourishment. Symptoms may include below average weight gain, below average fetal development, or slow growth of the uterus. It can also lead to foetal distress decreasing their heart rate and in serious cases an inability to tolerate a vaginal birth, thus requiring a caesarean delivery. An ultrasound examination will determine if growth of the foetus is adequate and doctors may advise preterm delivery if necessary. Placental insufficiency can be caused by conditions such as diabetes, high blood pressure or preeclampsia, maternal blood clotting disorders, smoking or taking drugs such as cocaine.
Preeclampsia: A complication of pregnancy where hypertension, high blood pressure, occurs in conjunction with high levels of protein in the urine and oedema. The increases in blood pressure can prevent adequate oxygen reaching the foetus and possibly lead to health problems for the baby. It is most common after the 20th week of pregnancy. Risk is increased if the mother already has high blood pressure, diabetes or kidney disease. Preeclampsia is the most common of the dangerous pregnancy complications and can affect both mother and baby. A variation of preeclampsia is HELLP syndrome, a life threatening liver disorder, also related to hypertension in pregnancy. It is usually diagnosed as a direct result of being evaluated for preeclampsia. HELLP is an abbreviation of Hemolytic anemia, Elevated Liver enzymes and Low Platelet count. Approximately 10% to 20% of women who have severe preeclampsia develop HELLP and the only way to reverse this syndrome is the birth of the baby to prevent the potential death of both mother and fetus.
Preterm premature rupture of membranes (PPROM): A condition which occurs in pregnancy when the amniotic sac spontaneously ruptures before the onset of labor. This can lead to spontaneous delivery of the baby within hours or can take weeks until birth. The mother is usually confined to hospital to monitor the pregnancy and prevent complications. There may be no known cause or it could be related to risk factors such as an infection, lower socioeconomic conditions where it is more common adequate antenatal care has not been received, vaginal bleeding from conditions such as placental abruption and smoking.
Previous premature birth: Women who have had a premature delivery previously have an increased chance of having another pre-term delivery.
Having a family history of premature birth. This means someone in your family (like your mother, grandmother or sister) has had a premature baby. If you were born prematurely, you’re more likely than others to give birth early.
Serious or an existing medical condition and other reasons: Conditions such as rhesus negative blood group, gestational diabetes, diabetes, kidney disease and high blood pressure can all affect a developing baby. In some cases, the decision to deliver a baby prematurely is because either they or the mother are medically unwell due to a health problem, congenital abnormality or surgical need.
Twin to twin transfusion syndrome (TTTS): A complication where two or more fetuses share a common placenta and associated with high morbidity and mortality.
Urine infection: Sometimes during the middle to later months of a pregnancy a serious uterine infection can trigger preterm labor. It is important that any possible urine infection be brought to the attention of your health care professional.
Uterine abnormalities: Women with an abnormally shaped uterus such as a bicornuate uterus could be at risk of preterm labor. The baby may have less room to grow and when there isn’t enough room for the baby, the stretching of the uterus can cause labor to begin.
Connective tissue disorders, like Ehlers-Danlos syndromes (also called EDS) and vascular Ehlers-Danlos syndrome (also called vEDS). Connective tissue is tissue that surrounds and supports other tissues and organs. Ehlers-Danlos syndromes can cause joints to be loose and easy to dislocate; skin to be thin and easily stretched and bruised; and blood vessels to be fragile and small. It also can affect your uterus and intestines. Vascular Ehlers-Danlos syndrome is the most serious kind of Ehlers-Danlos syndromes because it can cause arteries and organs (like the uterus) to rupture (burst). Ehlers-Danlos syndromes and vascular Ehlers-Danlos syndrome are genetic conditions that can be passed from parent to child through genes.
Being pregnant with a baby who has certain birth defects, like heart defects or spina bifida. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works. Spina bifida is a birth defect of the spine.
Thrombophilias. These are conditions that increase your risk of making abnormal blood clots.
Getting pregnant again too soon after having a baby. For most women it’s best to wait at least 18 months before getting pregnant again. Talk to your provider about the right amount of time for you.
Social, personal and economic
Mother’s Age: Younger than 17 years or over 35 years
Lower socioeconomic situations: even after assessing other variables such as maternal age, race, behavioral issues and medical situations, low income and social disadvantages lead to higher rates of premature birth. Studies continue to determine optimal means to address this issue.
Race: there is a greater risk of women of African descent to have premature births. This risk is seen to be as much as five times more than Caucasian women despite similar health care provision.
Behavioral
Substance use and abuse: This includes smoking, drinking alcohol or using illicit drugs. The use of some substances can lead to decreased oxygenation to the fetus and small for gestational age babies, birth defects and sadly fetal death if a baby is not delivered in time to prevent irreversible complications.
Late antenatal care: Situations that can potentially lead to premature birth can be better treated if early antenatal care is sought.
Stress: Certain hormones and proteins in the blood that help control the contraction of the uterus and the production of infection fighting cells are increased in times of stress. These can lead to increased risk of infections, uterine irritability and thereby increasing the risk of premature birth.
Preterm labor prevention
You might not be able to prevent preterm labor — but there’s much you can do to promote a healthy, full-term pregnancy. For example:
- Seek regular prenatal care. Prenatal visits can help your health care provider monitor your health and your baby’s health. Mention any signs or symptoms that concern you, even if you think they’re silly or unimportant. If you have a history of preterm labor or develop signs or symptoms of preterm labor, you might need to see your health care provider more often during pregnancy for exams and tests.
- Eat a healthy diet. During pregnancy, you’ll need more folic acid, calcium, iron and other essential nutrients. A daily prenatal vitamin — ideally starting a few months before conception — can help fill any gaps.
- Avoid risky substances. If you smoke, quit. Smoking might trigger preterm labor. Illicit drugs are off-limits, too. In addition, medications of any type — even those available over-the-counter — deserve caution. Get your health care provider’s OK before taking any medications or supplements.
- Protect yourself from infections. Talk to your provider about vaccinations that can help protect you from certain infections. Wash your hands with soap and water after using the bathroom or blowing your nose. Don’t eat raw meat, fish or eggs. Have safe sex. Don’t touch cat poop.
- Be cautious when using assisted reproductive technology (ART). If you’re planning to use ART to get pregnant, consider how many embryos will be implanted. Multiple pregnancies carry a higher risk of preterm labor.
- Wait at least 18 months between giving birth and getting pregnant again. Use birth control until you’re ready to get pregnant again. If you’re older than 35 or you’ve had a miscarriage or stillbirth, talk to your provider about how long to wait between pregnancies. Miscarriage is the death of a baby in the womb before 20 weeks of pregnancy. Stillbirth is the death of a baby in the womb after 20 weeks of pregnancy.
If your health care provider determines that you’re at increased risk of preterm labor, he or she might recommend taking additional steps to reduce your risk, such as:
- Taking preventive medications. If you have a history of premature birth, your health care provider might suggest weekly shots of a form of the hormone progesterone called hydroxyprogesterone caproate (Makena) during your second trimester. In additional, your doctor might offer progesterone, which is inserted in the vagina, as a preventive measure against preterm birth.
- Limiting certain physical activities. If you’re at risk of preterm labor or develop signs or symptoms of preterm labor, your health care provider might suggest avoiding heavy lifting or spending too much time on your feet.
- Managing chronic conditions. Certain conditions, such as diabetes and high blood pressure, increase the risk of preterm labor. Work with your health care provider to keep any chronic conditions under control.
If you have a history of preterm labor or premature birth, you’re at risk of a subsequent preterm labor. Work with your health care provider to manage any risk factors and respond to early warning signs and symptoms.
Preterm labor signs and symptoms
For some women, the signs and symptoms of preterm labor are unmistakable. For others, they’re more subtle.
If you have any of the following signs and symptoms before your 37th week of pregnancy, contact your doctor or midwife straight away, as you could be in labor:
- either a slow trickle or a gush of clear or pinkish fluid from your vagina (watery, mucus or bloody) or any increase in vaginal discharge
- your water breaks
- constant low, dull backache
- belly cramps like strong period pains with or without diarrhea
- regular or frequent painful contractions — a tightening sensation in the abdomen
- mild abdominal cramps
- a frequent need to urinate
- a feeling of pressure in your pelvis or lower abdomen (feeling like your baby is pushing down)
- vaginal spotting or bleeding
- a change in vaginal discharge – watery, mucous, or bloody vaginal discharge
- nausea, vomiting or diarrhea
- 4 or more contractions per hour (contractions that make your belly tighten like a fist. The contractions may or may not be painful)
- bleeding or blood spotting after 3 months into your pregnancy
Don’t delay if you have strong pain, a smelly discharge or bleeding from your vagina, or if you are feeling feverish, sick or have a temperature, call immediately as you may need urgent medical attention.
- Don’t worry about mistaking false labor for the real thing. Everyone will be pleased if it’s a false alarm.
You may have some of the symptoms but not others. For example, your waters may have broken but with no contractions, or vice versa. Contractions don’t always indicate that you’re in labor, so your healthcare team will carry out checks to find out.
Many women experience Braxton Hicks contractions, sometimes known as practice contractions. These can become quite strong and painful during the third trimester, and it’s easy to mistake them for the real thing.
Your healthcare team will check
- whether you are actually in labor
- if labor hasn’t started, whether your symptoms are due to some other cause that needs treating
- if you are definitely in labor, whether this has been caused by something (such as an infection) that needs treating, and how far the labor is progressing, so they can line up the facilities you need, either to delay the birth or to deliver the baby.
When you see your doctor, he/she may do a pelvic exam or a transvaginal ultrasound to see if your cervix has started to become thinner and open for labor. Your cervix is the opening to the uterus (womb) that sits at the top of the vagina (birth canal). A transvaginal ultrasound is done inside the vagina instead of on the outside of your belly. Like a regular ultrasound, it uses sound waves and a computer to make a picture of your baby. If you’re having contractions, your doctor will monitor them to see how strong and far apart they are. You may have other tests to help your doctor determine whether you really are in labor.
If you’re having preterm labor, your doctor may give you treatment to help stop it or to help improve your baby’s health before birth. Talk with your doctor about which treatments may be right for you.
Preterm labor diagnosis
To help diagnose preterm labor, your doctor will document your signs and symptoms. If you’re experiencing regular, painful contractions and your cervix has begun to soften, thin and open before 37 weeks of pregnancy, you’ll likely be diagnosed with preterm labor.
Tests and procedures to diagnose preterm labor include:
- Pelvic exam. Your health care provider might evaluate the firmness and tenderness of your uterus and the baby’s size and position. He or she might also do a pelvic exam to determine if your cervix has begun to open — if your water hasn’t broken and the placenta isn’t covering your cervix (placenta previa).
- Ultrasound. An ultrasound might be used to measure the length of your cervix and determine your baby’s size, age, weight and position in your uterus. You might need to be monitored for a period of time and then have another ultrasound to measure any changes in your cervix, including cervical length.
- Uterine monitoring. Your health care provider might use a uterine monitor to measure the duration and spacing of your contractions.
- Lab tests. Your health care provider might take a swab of your vaginal secretions to check for the presence of certain infections and fetal fibronectin — a substance that acts like a glue between the fetal sac and the lining of the uterus and is discharged during labor. However, this test isn’t reliable enough to be used on its own to assess the risk of preterm labor.
- Maturity amniocentesis. Your health care provider might recommend a procedure in which amniotic fluid is removed from the uterus (amniocentesis) to determine your baby’s lung maturity. The technique can also be used to detect an infection in the amniotic fluid.
If you’re in preterm labor, your health care provider will explain the risks and benefits of trying to stop your labor. Keep in mind that preterm labor sometimes stops on its own.
Preterm labor treatment
Preterm labor is labor that happens too early, before 37 weeks of pregnancy. If you have preterm labor, your doctor may recommend some treatments that may help stop your contractions and prevent health problems for you and your baby. They aren’t guaranteed, but research shows that they do help some people.
Preterm labor at >34 weeks, you’ll be admitted into the hospital for observation for 4-6 hours. If you do not have progressive cervical dilation and effacement, and your baby’s well-being is noted on a reactive non-stress test, and complications in pregnancy have been excluded, your doctor may send you home with instructions for follow-up in 1-2 weeks and return if there are additional signs and symptoms of preterm labor or other pregnancy concerns.
Mothers presenting at <34 weeks with signs and symptoms of preterm labor are hospitalized. In preterm labor with intact membranes, tocolytic drugs for up to 48 hours are used to inhibit labor 19.
If your waters have broken
Your unborn baby lies in an amniotic sac of fluid or ‘waters’. ‘Waters breaking’ means that the sac has ruptured or broken. Your waters normally break around the time labor is due but in around 2% of pregnancies they break early for various reasons.
If your waters break before your baby has reached full term (37 weeks), the medical name for it is preterm prelabour rupture of the membranes, or PPROM. If this happens early, before the contractions start, it can (but does not always) trigger early labor.
If your waters have broken early, you will experience it as a trickle or a gush of water from your vagina. It is likely to continue leaking once it has started. If it isn’t too heavy you can use a sanitary towel to catch it. This will also allow you to see what color it is, which will be helpful information for health professionals. It may be pinkish if it contains some blood, or it may be clear. If it greenish or brown go to the maternity unit as soon as possible. If it is heavy, you may need to use a towel.
Does it hurt when my waters break?
No it shouldn’t hurt when your waters break or when they are broken for you. The amniotic sac, which is the part that ‘breaks’ doesn’t have pain receptors, which are the things that cause you to feel pain when you get a cut for example.
You are likely to have an internal examination. This will allow the doctor to look at your cervix and check:
- if the leaking fluid is amniotic fluid
- if it is changing in preparation for labor
- to check for infection by taking a swab.
You might have an ultrasound scan to estimate the amount of fluid left around your baby.
If only a very small amount of amniotic fluid leaks, it is not always easy to be sure whether your waters have broken.
- You may be advised to wear a pad and stay in hospital for a few hours to monitor the situation.
- If you go home but continue to leak fluid at home, you should return to the hospital again.
If your waters are shown to have broken, you will be advised to come into hospital for at least 48 hours. You and your unborn baby will be closely monitored for signs of infection. This will include having your temperature and pulse taken regularly, and your baby’s heart rate will also be monitored.
What are the risks if my waters break early (PPROM)?
If your waters break early the risks and treatment are dependent on the stage of pregnancy you are at.
- You are at risk of going into preterm labor – the health risks for the baby of early birth are greater the younger they are.
- If you do not go into labor, you and the baby are at risk of infection.
The doctors have to balance these two considerations. If the waters have broken because of infection, you and the baby have a high risk of getting the infection and you may need to deliver sooner to prevent this.
If the waters have broken but there is no infection currently present, you and the baby are still at risk but the immediate risk is lesser and your treatment will depend on your stage of pregnancy.
- If you are under 24 weeks of pregnancy and the baby is born, sadly, it is unlikely the baby will survive.
- If you are over 30 weeks and the baby is born, the likelihood of your baby surviving is much higher – over 95%.
If your waters have broken there’s an increased risk of infection for you and your baby. You’ll be offered:
- antibiotics to take for a maximum of 10 days, or until labor starts – whichever is sooner
- tests for infection, which may include blood and urine tests
Figure 1. Preterm labor – pre-labor rupture of membranes (P-PROM)
Preterm pre-labor rupture of membranes (P-PROM) doesn’t definitely mean you’re going into labor. You may be able to go home if there’s no infection and you don’t go into labor within 48 hours.
If you go home, you’ll be advised to tell your midwife immediately if:
- your temperature is raised (a raised temperature is usually over 99.5 °F (37.5 °C) but check with your midwife – they may need you to call before it gets to 99.5 °F (37.5 °C). You should take your temperature every four hours when you’re awake
- any fluid coming from your vagina (called vaginal loss) is colored or smelly
- you bleed from your vagina
- your baby’s movements slow down or stop.
You should avoid having sexual intercourse.
Contact your doctor or midwife and return to the hospital immediately if you have:
- a raised temperature (more than 98.6 °F or 37 °C)
- flu-like symptoms (feeling hot and shivery)
- vaginal bleeding
- if the leaking fluid becomes greenish or smelly
- contractions
- abdominal pain
- if you are worried that the baby is not moving as normal.
Inducing labor or preterm labor with PPROM
If you are past 34 weeks the doctor will weigh up the benefits of inducing labor before the due date to avoid the risk of infection with the disadvantages of being born premature, and may make a recommendation for early delivery.
You may need to stay in a hospital that has a neonatal unit and be monitored carefully for any sign of infection. You may also be treated with antibiotics, corticosteroids and magnesium sulfate (if you are less than 30 weeks) to help prepare your baby in case the are born prematurely.
Over 80% of women who have pre-labor rupture of membranes (PPROM) deliver their baby within seven days of their waters breaking.
Causes of waters breaking early (PPROM)
Intrauterine infection is present in around a third of women with pre-labor rupture of membranes (PPROM). In many cases however it happens without any infection being present. The reason for these cases is unclear, however it has been linked to heavy smoking (more than 10 cigarettes a day) in pregnancy.
What if there are no waters left in my womb?
Your baby’s amniotic sac has to have the right amount of amniotic fluid for the pregnancy to continue normally. If there is a break in the waters your baby will continue to produce amniotic fluid.
Before 23 weeks, the baby needs ‘waters’ to be present for their lungs to develop normally. Loss of water before this can lead to severe problems with lung development that can be critical after birth. After 23 weeks your baby does not need the amniotic fluid so much, so low levels of fluid may not be a problem in itself, but if the low levels are due to your waters breaking then there is a risk of infection.
If your waters haven’t broken
Your midwife or doctor should discuss with you the symptoms of preterm labor and offer checks to see if you’re in labor. These checks can include asking you about your medical and pregnancy history, and about possible labor signs, such as:
- contractions – how long, how strong and how far apart they are
- any pain
- vaginal loss, such as waters or a show
You may be offered a vaginal examination, and your pulse, blood pressure and temperature may also be checked.
Your midwife or doctor will also check your baby. They’ll probably feel your bump to find out the baby’s position and how far into your pelvis the baby’s head is.
They should also ask about your baby’s movements in the last 24 hours. If they don’t ask, tell them about the baby’s movements.
If you’re in preterm labor
Your midwife or doctor may offer you:
- medicine to try to slow down or stop your labor (tocolytic). Examples of this are magnesium sulphate, terbutaline and nifedipine.
- corticosteroid injections, which can help your baby’s lungs
Tocolytics
Your doctor might give you a medication called a tocolytic to temporarily slow or stop your labor contractions. Tocolytic medications won’t halt preterm labor for longer than two days because they don’t address the underlying cause of preterm labor. However, tocolytics might delay preterm labor long enough for corticosteroids to provide the maximum benefit or, if necessary, for you to be transported to a hospital that has a NICU (neonatal intensive care unit) that can provide specialized care for your premature baby. A NICU is a specialized nursery where newborns get medical care.
There are several types of tocolytic, including:
- Beta-adrenergic receptor agonists: Most commonly used beta-2 agonist is terbutaline
- Calcium channel blockers: Nifedipine is preferred as it has fewer side effects than other drugs
- Magnesium sulfate: Magnesium sulfate is one of the most commonly used drugs in preterm labor. Because of its neuroprotective effect, administration of antenatal magnesium sulfate in women at risk of preterm delivery has been associated with a decrease in occurrence and severity of cerebral palsy in infants 20, 21, 22. Because magnesium sulfate can cause maternal complications (e.g., respiratory depression, cardiac arrest), following institutional protocols is suggested for determining appropriate use 1. Mothers on magnesium sulfate should have monitoring for the following: deep tendon reflexes, vital signs, magnesium levels, urine output, and respiratory depression.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Indomethacin is safest if given no longer than the recommended 48 hours due to the risk of patent ductus arteriosis (PDA) closure
Typically, tocolytics are a consideration between 22 and 34 weeks of gestational age and only when there are no contraindications. Contraindications to tocolytic drug use include preeclampsia with severe features, intrauterine fetal demise, lethal fetal anomaly, chorioamnionitis, hemorrhage, the presence of fetal distress and significant maternal heart disease 1, 19. The continuous or long-term use of tocolytics has not been shown to further delay delivery or improve neonatal outcomes and is not recommended 1.
First-line agents used to delay delivery up to 48 hours include calcium channel blockers (e.g., nifedipine, nicardipine), beta-adrenergic receptor agonists (e.g., terbutaline), and nonsteroidal anti-inflammatory drugs such as prostaglandin inhibitors (e.g., indomethacin, ketorolac) 19. A systematic review and meta-analysis show that prostaglandin inhibitors and calcium channel blockers are the best tocolytics based on four outcomes: delay of delivery by 48 hours, neonatal mortality, neonatal respiratory distress syndrome, and maternal adverse effects (all causes) 23. Magnesium sulfate can be used as a tocolytic but is associated with significant maternal adverse effects. Caution must be used if combining magnesium sulfate with beta-adrenergic receptor agonists or calcium channel blockers because of possible maternal complications. Prostaglandin inhibitors may be used in combination with magnesium sulfate with lower maternal adverse effects; however, use of prostaglandin inhibitors after 32 weeks’ gestation may be associated with premature closure of the ductus arteriosus in the infant 1.
Your doctor can help you weigh the risks and benefits of using a tocolytic. In addition, your doctor won’t recommend a tocolytic if you have health conditions, such as pregnancy-induced high blood pressure (preeclampsia) and heart problem. Preeclampsia is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Some of these signs include having protein in the urine, changes in vision and severe headache.
What side effects can tocolytics cause?
Several kinds of tocolytics may be used during preterm labor, each with different side effects.
Beta-adrenergic receptor agonists, like terbutaline. Possible side effects for your baby may include having a fast heartbeat. Possible side effects for you may include:
- Chest pain; fast or irregular heartbeat
- Breathing trouble; fluid in the lungs
- Diarrhea, nausea (feeling sick to your stomach), throwing up
- Feeling dizzy; shaking or feeling nervous; seizures
- Fever, headache
- High blood sugar
- Low blood pressure; low blood potassium
Calcium channel blockers, like nifedipine. There are no side effects for your baby. Possible side effects for you may include:
- Constipation, diarrhea, nausea
- Feeling dizzy or faint
- Headache
- Low blood pressure
- Redness of the skin
Magnesium sulfate. If you’re in premature labor and you’re between 24 and 29 weeks pregnant you should be offered magnesium sulfate. This can help protect your baby’s brain development. You may also be offered it if you’re in labor between 30 and 34 weeks. This is to protect your baby against problems linked to being born too soon, such as cerebral palsy. Side effects for your baby may include:
- Being tired and drowsy
- Slowed breathing
- Weak muscles
- Low levels of calcium and bone problems, if the drug is used for more than 5 to 7 days.
Side effects for you may include:
- Breathing problems, fluid in the lungs
- Dry mouth
- Fatigue (being very tired), weak muscle
- Headache, double vision, slurred speech
- Heart attack
- Nausea or throwing up
- Redness of the skin, heavy sweating
Nonsteroidal anti-inflammatory drugs (also called NSAIDs), like indomethacin. Side effects for your baby may include:
- Bleeding in the brain or heart
- Patent ductus arteriosis, also called PDA. This is a heart problem that’s common in premature babies.
- Jaundice. This is a common condition caused by the build-up of a substance called bilirubin in the blood that makes a baby’s skin and the white parts of his eyes look yellow.
- Kidney problems, like making too little urine
- Necrotizing enterocolitis (also called NEC). This is a problem in a baby’s intestines.
- Rising blood pressure in the lungs
Side effects for you include:
- Feeling dizzy
- Heartburn
- Nausea or throwing up
- Oligohydramnios. This is when you have too little amniotic fluid. Amniotic fluid is the fluid that surrounds your baby in the womb.
- Swollen stomach lining
- Vaginal bleeding
Slowing down labor or stopping it isn’t appropriate in all circumstances – your midwife or doctor can discuss your situation with you. They will consider:
- how many weeks pregnant you are
- whether it might be safer for the baby to be born – for example, if you have an infection or you’re bleeding
- local neonatal (newborn) care facilities and whether you might need to be moved to another hospital
- your wishes
Antenatal corticosteroid injections
Antenatal corticosteroid injections with medicines such as betamethasone and dexamethasone can help speed up your baby’s lungs development in order to get ready for breathing if they’re born prematurely. Antenatal corticosteroid injections also help reduce your baby’s chances of having certain health problems after birth, including infant respiratory distress syndrome, intraventricular hemorrhage (also called IVH) and necrotizing enterocolitis (also called NEC) 24. Infant respiratory distress syndrome is a condition that affects a baby’s breathing. Intraventricular hemorrhage is bleeding in the brain. Necrotizing enterocolitis is a condition that affects a baby’s intestines. Once preterm labor is confirmed, a single course of corticosteroids is the only intervention for improving neonatal outcomes.
The use of corticosteroids is associated with decreased neonatal morbidity and mortality 1. Infants whose mothers receive antenatal corticosteroids are less likely to exhibit respiratory distress syndrome, intraventricular hemorrhage, and necrotizing enterocolitis compared with those whose mothers did not receive corticosteroids 1, 24. Recent data suggest that a second rescue course of antenatal corticosteroids may be considered if the first dose was given more than seven days earlier and there is still a risk of preterm delivery before 34 weeks gestation 1.
There are two injections, given 12 hours apart – your midwife or doctor will discuss the benefits and risks with you. Betamethasone, two 12-mg doses given intramuscularly (IM) 24 hours apart, or dexamethasone, four 6-mg doses given intramuscularly (IM) every 12 hours, is recommended between 24 and 34 weeks’ gestation, and may be considered as early as 23 weeks’ gestation, in women likely to deliver within seven days regardless of membrane status 24.
A single course of corticosteroids has been shown to help with a baby’s development and therefore will increase the chance of your baby surviving, once born. Corticosteroid injection also lessens the chance of your baby having serious complications after birth such as breathing problems owing to the lungs not being fully developed, bleeding into the brain, serious infection or bowel inflammation.
Corticosteroids probably won’t be offered after 36 weeks as your baby’s lungs are likely to be ready for breathing on their own.
Can corticosteroids harm me or my baby?
A single course of two to four injections is considered to be safe for you and your baby. More evidence is needed to say whether two or more courses of corticosteroids during pregnancy are safe for your baby.
At what stage of pregnancy should corticosteroids be given?
Corticosteroids help most if they are given to you between 24 weeks and 34 weeks plus 6 days of pregnancy. If you are having a planned caesarean section between 35 and 38 weeks plus 6 days, corticosteroids are usually recommended. Corticosteroids may be given earlier than 24 weeks, but the evidence that they will be helpful for your baby in that situation is less clear; your obstetrician doctor will discuss this with you.
How long are corticosteroids effective for?
Corticosteroids are of most help if the last dose is given to you between 24 hours and 1 week before you have your baby. There may still be benefit even if your baby is born within 24 hours of the first dose.
Who should be given corticosteroids in pregnancy?
You may be advised to have corticosteroids if there is an increased chance that your baby will be born before 35 weeks of pregnancy.
This includes:
- if you are in preterm labor
- if you are suspected to be in preterm labor but this has not been confirmed yet
- if your waters break even if you are not having contractions
- if it may benefit your baby to be delivered early, for example if your baby is not growing
- if it may benefit you to have your baby early, for example if you are seriously unwell, are bleeding heavily or have severe pre-eclampsia.
If you are having a planned caesarean section before 39 weeks of pregnancy, corticosteroids are recommended to lessen the chance of breathing problems for your baby. If you have diabetes or gestational diabetes, you may need to be in hospital since corticosteroids increase the blood sugar level.
When are corticosteroids not necessary?
Giving treatment just in case an event occurs is known as prophylactic treatment. If you have previously had a baby born early, have a multiple pregnancy or have had treatment to your cervix (entrance to the womb), prophylactic treatment with corticosteroids early in pregnancy is not recommended because there is no evidence that it will help your baby.
Are there any circumstances where you wouldn’t be able to have corticosteroids?
Corticosteroids can suppress the mother’s immune system, but there is no evidence that a single course of corticosteroids will cause harm even if you have a severe infection. If you or your baby are unwell, corticosteroids will usually be started but delivery of your baby will not be delayed to allow you to complete the course.
Antibiotics
Antibiotics include ceftriaxone, clarithromycin, and metronidazole, kill infections caused by bacteria. If you have a positive Group B streptococcus test, or if you have preterm premature rupture of membranes (PPROM), your doctor may give you antibiotics to help prevent infections in you and your baby, especially before 32 weeks’ gestation. PPROM is when the sac around your baby breaks before 37 weeks of pregnancy.
Although several trials have been conducted, no studies have shown that use of antibiotics during preterm labor is effective in delaying delivery or reducing neonatal morbidity associated with preterm delivery 1. This lack of benefit has no bearing on established guidelines recommending the use of antibiotics for group B streptococcus prophylaxis and in women with premature rupture of membranes (PROM).
- American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice Bulletin No. 171: Management of Preterm Labor. Obstet Gynecol. 2016 Oct;128(4):e155-64. doi: 10.1097/AOG.0000000000001711[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Suman V, Luther EE. Preterm Labor. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536939[↩][↩][↩]
- Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2009. Natl Vital Stat Rep 2010;59(3):1–19. https://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_03.pdf[↩]
- Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008 Jan 5;371(9606):75-84. doi: 10.1016/S0140-6736(08)60074-4[↩]
- MacDorman MF, Callaghan WM, Mathews TJ, Hoyert DL, Kochanek KD. Trends in preterm-related infant mortality by race and ethnicity: United States, 1999–2004. NCHS Health E-Stat . Hyattsville (MD): National Center for Health Statistics; 2007. https://www.cdc.gov/nchs/data/hestat/infantmort99-04/infantmort99-04.htm[↩]
- Mathews TJ, MacDorman MF. Infant mortality statistics from the 2006 period linked birth/infant death data set. Natl Vital Stat Rep. 2010 Apr 30;58(17):1-31. https://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_17.pdf[↩]
- Management of Preterm Labor. Practice Bulletin. Number 171, October 2016. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2016/10/management-of-preterm-labor[↩]
- Preterm labor and premature birth: Are you at risk? https://www.marchofdimes.org/find-support/topics/birth/preterm-labor-and-premature-birth-are-you-risk[↩][↩][↩]
- Hamilton BE, Martin JA, Osterman MJ. Births: Preliminary Data for 2015. Natl Vital Stat Rep. 2016 Jun;65(3):1-15.[↩]
- Owen J, Hankins G, Iams JD, Berghella V, Sheffield JS, Perez-Delboy A, Egerman RS, Wing DA, Tomlinson M, Silver R, Ramin SM, Guzman ER, Gordon M, How HY, Knudtson EJ, Szychowski JM, Cliver S, Hauth JC. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009 Oct;201(4):375.e1-8. doi: 10.1016/j.ajog.2009.08.015[↩]
- Conde-Agudelo A, Romero R, Nicolaides K, Chaiworapongsa T, O’Brien JM, Cetingoz E, da Fonseca E, Creasy G, Soma-Pillay P, Fusey S, Cam C, Alfirevic Z, Hassan SS. Vaginal progesterone vs. cervical cerclage for the prevention of preterm birth in women with a sonographic short cervix, previous preterm birth, and singleton gestation: a systematic review and indirect comparison metaanalysis. Am J Obstet Gynecol. 2013 Jan;208(1):42.e1-42.e18. doi: 10.1016/j.ajog.2012.10.877[↩][↩]
- Committee on Practice Bulletins—Obstetrics, The American College of Obstetricians and Gynecologists. Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012 Oct;120(4):964-73. doi: 10.1097/AOG.0b013e3182723b1b[↩]
- Preterm Labor: Prevention and Management. Am Fam Physician. 2017;95(6):366-372. https://www.aafp.org/pubs/afp/issues/2017/0315/p366.html[↩][↩]
- Hassan SS, Romero R, Vidyadhari D, Fusey S, Baxter JK, Khandelwal M, Vijayaraghavan J, Trivedi Y, Soma-Pillay P, Sambarey P, Dayal A, Potapov V, O’Brien J, Astakhov V, Yuzko O, Kinzler W, Dattel B, Sehdev H, Mazheika L, Manchulenko D, Gervasi MT, Sullivan L, Conde-Agudelo A, Phillips JA, Creasy GW; PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011 Jul;38(1):18-31. doi: 10.1002/uog.9017[↩]
- Keirse MJ. Progestogen administration in pregnancy may prevent preterm delivery. Br J Obstet Gynaecol. 1990 Feb;97(2):149-54. doi: 10.1111/j.1471-0528.1990.tb01740.x[↩][↩]
- Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007 Aug 2;357(5):462-9. doi: 10.1056/NEJMoa067815[↩][↩]
- Iams JD. Clinical practice. Prevention of preterm parturition. N Engl J Med. 2014 Jan 16;370(3):254-61. doi: 10.1056/NEJMcp1103640[↩]
- Werner, E.F., Han, C.S., Pettker, C.M., Buhimschi, C.S., Copel, J.A., Funai, E.F. and Thung, S.F. (2011), Universal cervical-length screening to prevent preterm birth: a cost-effectiveness analysis. Ultrasound Obstet Gynecol, 38: 32-37. https://doi.org/10.1002/uog.8911[↩]
- Haas DM, Imperiale TF, Kirkpatrick PR, Klein RW, Zollinger TW, Golichowski AM. Tocolytic therapy: a meta-analysis and decision analysis. Obstet Gynecol. 2009 Mar;113(3):585-594. doi: 10.1097/AOG.0b013e318199924a[↩][↩][↩]
- Doyle LW, Crowther CA, Middleton P, Marret S. Antenatal magnesium sulfate and neurologic outcome in preterm infants: a systematic review. Obstet Gynecol. 2009 Jun;113(6):1327-1333. doi: 10.1097/AOG.0b013e3181a60495[↩]
- Marret, S., Marpeau, L., Zupan-Simunek, V., Eurin, D., Lévêque, C., Hellot, M.-F., Bénichou, J. and (2007), Magnesium sulphate given before very-preterm birth to protect infant brain: the randomised controlled PREMAG trial. BJOG: An International Journal of Obstetrics & Gynaecology, 114: 310-318. https://doi.org/10.1111/j.1471-0528.2006.01162.x[↩]
- Rouse DJ, Hirtz DG, Thom E, Varner MW, Spong CY, Mercer BM, Iams JD, Wapner RJ, Sorokin Y, Alexander JM, Harper M, Thorp JM Jr, Ramin SM, Malone FD, Carpenter M, Miodovnik M, Moawad A, O’Sullivan MJ, Peaceman AM, Hankins GD, Langer O, Caritis SN, Roberts JM; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. A randomized, controlled trial of magnesium sulfate for the prevention of cerebral palsy. N Engl J Med. 2008 Aug 28;359(9):895-905. doi: 10.1056/NEJMoa0801187[↩]
- Haas DM, Caldwell DM, Kirkpatrick P, McIntosh JJ, Welton NJ. Tocolytic therapy for preterm delivery: systematic review and network meta-analysis. BMJ. 2012 Oct 9;345:e6226. doi: 10.1136/bmj.e6226[↩]
- McGoldrick E, Stewart F, Parker R, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020 Dec 25;12(12):CD004454. doi: 10.1002/14651858.CD004454.pub4[↩][↩][↩]