Gestational diabetes
Gestational diabetes also called gestational diabetes mellitus (GDM) is a type of diabetes that some women get during pregnancy who don’t already have diabetes. Diabetes is a condition in which your body has too much sugar (also called glucose) in your blood. Gestational diabetes occurs when a woman experiences high blood glucose levels during pregnancy. As gestational diabetes is a condition that occurs during pregnancy, it is not the same as having pre-existing diabetes during your pregnancy. Gestational diabetes occurs when your body can’t make enough insulin during your pregnancy. Insulin is a hormone made by your pancreas that acts like a key to let blood sugar into the cells in your body for use as energy. This leads to higher than normal levels of sugar in your blood, which can be unhealthy for both you and the baby. Typically, women with gestational diabetes have no symptoms. Your medical history and whether you have any risk factors may suggest to your doctor that you could have gestational diabetes, but you’ll need to be tested to know for sure. Most women are diagnosed after routine tests during pregnancy. Most pregnant women get tested for gestational diabetes at 24 to 28 weeks of pregnancy. Gestational diabetes usually goes away after your baby is born.
During pregnancy, the placenta produces hormones to sustain your pregnancy and your body goes through changes such as weight gain. These hormones and changes cause your body’s cells to use insulin less effectively, a condition called insulin resistance. Insulin resistance increases your body’s need for insulin. Normally, your pancreas responds by producing enough extra insulin to overcome this resistance. But sometimes your pancreas can’t keep up. When this happens, too little glucose gets into your cells and too much stays in your blood, resulting in gestational diabetes. Women who experience gestational diabetes have a higher risk of developing type 2 diabetes in the future.
All pregnant women have some insulin resistance during late pregnancy. However, some women have insulin resistance even before they get pregnant. They start pregnancy with an increased need for insulin and are more likely to have gestational diabetes.
Every year, 7 out of every 100 pregnancies in the United States are affected by gestational diabetes. You’re more likely than other women to have gestational diabetes (GDM) if you’re Asian, South Asian, African-American or African Caribbean, Middle Eastern, Native American, Hispanic or Pacific Islander. The rise in gestational diabetes and pregestational type 2 diabetes (having type 2 diabetes before pregnancy) in parallel with obesity both in the U.S. and worldwide is of particular concern 1.
Most of the time it can be controlled and treated during pregnancy. If it’s not treated, gestational diabetes can cause problems for you and your baby.
Having gestational diabetes increases your risk of developing it again in future pregnancies. It also increases your risk of developing type 2 diabetes after giving birth or later in life.
Babies born to women with diabetes are at risk of being born larger than average, or with a birth defect. They may also be born prematurely or even stillborn. They are also at risk of becoming overweight and going on to develop type 2 diabetes as an adult.
These risks are greatly reduced if you keep your blood sugars under good control.
Managing gestational diabetes will help make sure you have a healthy pregnancy and a healthy baby. This will include eating well and keeping active.
Gestational diabetes usually goes away after you have your baby.
For many women with gestational diabetes, an important part of managing diabetes — as well as your overall health — is maintaining a healthy weight through a healthy diet and exercise plan. Eating a healthy diet that is high in fiber and low in carbohydrates and getting regular exercise may be enough to lower blood glucose levels. However, some women may need to take insulin shots and/or a diabetes medication called metformin.
If not treated, gestational diabetes can cause pregnancy complications, including:
- Cesarean section also called C-section, is a surgery in which your baby is born through a cut that your doctor makes in your belly and uterus (womb). You may need to have a c-section if you have complications during pregnancy, like your baby being very large (macrosomia). Most women with gestational diabetes can have a vaginal birth. But they’re more likely to have a c-section than women without gestational diabetes.
- High blood pressure and preeclampsia. High blood pressure (hypertension) is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy. Preeclampsia is when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Signs of preeclampsia include having protein in the urine, changes in vision and severe headaches. High blood pressure and preeclampsia can increase your risk for premature birth.
- Macrosomia (baby being very large). This means your baby weighs more than 8 pounds, 13 ounces (4,000 grams) at birth. Weighing this much makes your baby more likely to get hurt during labor and birth. And you may need to have a c-section to keep you and your baby safe.
- Perinatal depression also called postpartum depression. This is depression that happens during pregnancy or in the first year after having a baby. Depression is a medical condition that causes feelings of sadness and a loss of interest in things you like to do. It can affect how you feel, think and act and can interfere with your daily life. It needs treatment to get better.
- Premature birth. This is birth before 37 weeks of pregnancy. Most women with gestational diabetes have a full-term pregnancy that lasts between 39 and 40 weeks. But if there are complications with your pregnancy, you may need to have your labor induced before your due date. Inducing labor means your provider gives you medicine or breaks your water (amniotic sac) to make your labor begin.
- Shoulder dystocia or other birth injuries also called birth trauma. Shoulder dystocia happens when a baby’s shoulders get stuck inside the mother’s pelvis during labor and birth. It often happens when a baby is very large. It can cause serious injury to both mom and baby. Complications for moms caused by shoulder dystocia include postpartum hemorrhage (heavy bleeding). For babies, the most common injuries are fractures to the collarbone and arm and damage to the brachial plexus nerves. These nerves go from the spinal cord in the neck down the arm. They provide feeling and movement in the shoulder, arm and hand.
- Death. Untreated gestational diabetes can result in a baby’s death either before or shortly after birth.
- Stillbirth. This is the death of a baby in the womb after 20 weeks of pregnancy.
Gestational diabetes also can cause health complications for your baby after birth, including:
- Breathing problems, including infant respiratory distress syndrome (also called RDS). This is a breathing problem caused when babies don’t have enough surfactant in their lungs. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing.
- Jaundice. This is a medical condition in which a baby’s eyes and skin look yellow. A baby has jaundice when his liver isn’t fully developed or isn’t working well.
- Low blood sugar also called hypoglycemia. Sometimes babies of mothers with gestational diabetes develop low blood sugar (hypoglycemia) shortly after birth because their own insulin production is high. Prompt feedings and sometimes an intravenous glucose solution can return the baby’s blood sugar level to normal.
- Obesity later in life
- Diabetes later in life
Gestational diabetes key points:
- Doctors use blood tests to diagnose gestational diabetes.
- If untreated, gestational diabetes can cause problems for your baby, like premature birth and stillbirth.
- You should expect more appointments, tests and scans than other pregnant women. These will help make sure your pregnancy is going as smoothly as possible.
- You should also expect to be in touch with your diabetes and antenatal team every one to two weeks throughout your pregnancy.
- Women with gestational diabetes can and do have healthy pregnancies and healthy babies.
- You are usually advised to give birth in hospital and in many cases will be able to have a vaginal birth if this is what you choose. And you will be able to breastfeed if you want to.
- Most pregnant women get a test for gestational diabetes at 24 to 28 weeks of pregnancy.
- Gestational diabetes usually goes away after you have your baby; but if you have it, you’re more likely to develop diabetes later in life.
- Talk to your health care provider about what you can do to reduce your risk for gestational diabetes and help prevent diabetes in the future.
What is insulin?
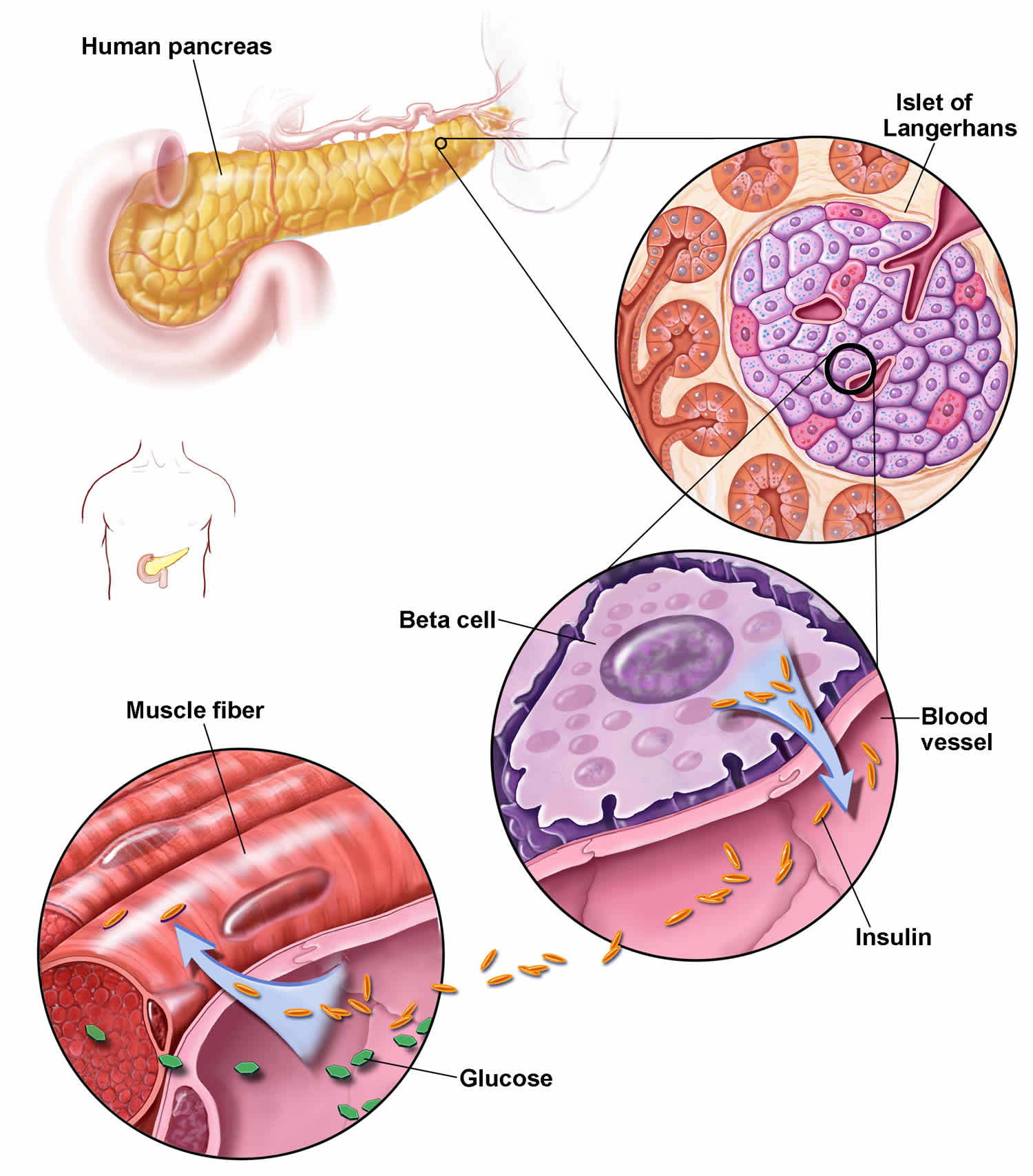
Insulin is a hormone that comes from your pancreas, a gland situated behind and below the stomach. The pancreas secretes insulin into the bloodstream. The insulin circulates, enabling sugar to enter your cells. Insulin lowers the amount of sugar in your bloodstream. As your blood sugar level drops, so does the secretion of insulin from your pancreas.
If your body isn’t able to make enough insulin or if your body’s cells have trouble accepting insulin, your blood glucose level can rise to a dangerous level. This may lead to diabetes, a serious disease that can damage your body’s organs if it is not kept under control.
How does insulin work?
Insulin is a hormone that comes from the gland situated behind and below the stomach (pancreas). Insulin regulates how the body uses sugar in the following ways:
- Sugar in the bloodstream triggers the pancreas to secrete insulin.
- Insulin circulates in the bloodstream, enabling sugar to enter your cells.
- The amount of sugar in your bloodstream drops.
- In response to this drop, the pancreas releases less insulin.
Figure 1. Insulin and gestational diabetes
What is glucose?
Glucose is the type of sugar that your body uses as its principal energy source. Glucose comes from two major sources: the food you eat and your liver. Your liver stores glucose as glycogen and makes glucose. The glucose enters your bloodstream and is taken up by your body’s cells with the help of a hormone called insulin.
If your body isn’t able to make enough insulin, or if your body’s cells have trouble accepting insulin, your blood glucose level can rise to a dangerous level. This may lead to diabetes, a serious disease that can damage your body’s organs if it is not kept under control.
When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen into glucose to keep your glucose level within a normal range.
What is normal sugar level in pregnancy?
A blood sugar level with blood sample taken at 1 hour after meal less than 140 mg/dL (7.8 mmol/L) is normal. If you’re not able to check until two hours – rather than one hour – after a meal, you should aim for below 115.2 mg/dL (6.4 mmol/L).
A fasting blood sugar level (a blood sample taken after an overnight fast) less than 95.4 mg/dL (5.3 mmol/L) is normal.
American Diabetes Association recommended daily target blood glucose levels for most women with gestational diabetes are 1, 2:
- Before a meal, at bedtime, and overnight: 95 mg/dL (5.3 mmol/L) or less
- One hour after a meal: 140 mg/dL (7.8 mmol/L) or less
- Two hours after a meal: 120 mg/dL (6.7 mmol/L) or less
Ask your doctor what targets are right for you. Your healthcare team will also talk to you about how often to test your blood sugar level, how to do it properly and how to safely meet your targets. You and your care team should also agree an ideal target blood sugar level that’s right for you, and is manageable without causing low blood sugar levels or hypoglycemia.
What is gestational diabetes blood glucose levels?
The criteria for diagnosing gestational diabetes is different than for diagnosing diabetes.
Gestational diabetes should be diagnosed if the woman has either:
- a fasting blood sugar level (a blood sample taken after an overnight fast) of 100.8 mg/dL (5.6 mmol/L) or above
- OR
- a 2-hours after a meal blood sugar level of 140.4 mg/dL (7.8mmol/L) or above.
If I have gestational diabetes, how can I prevent getting diabetes later in life?
For most women, gestational diabetes goes away after giving birth. But having gestational diabetes makes you more likely to develop type 2 diabetes later in life. Type 2 diabetes is the most common kind of diabetes. If you have type 2 diabetes, your pancreas makes too little insulin or your body becomes resistant to it (can’t use it normally).
Here’s what you can do to help reduce your risk of developing type 2 diabetes after pregnancy:
- Breastfeed. Breastfeeding is one of the ways you can help reduce your risk of developing type 2 diabetes after giving birth. Breastfeeding can help you lose weight after pregnancy. Being overweight makes you more likely to develop type 2 diabetes.
- Get tested for diabetes 4 to 12 weeks after your baby is born. If the test is normal, get tested again every 1 to 3 years.
- Get to and stay at a healthy weight.
- Talk to your family physician about medicine that may help prevent type 2 diabetes.
Can gestational diabetes increase my risk for problems during pregnancy?
Yes. If not treated, gestational diabetes can increase your risk for pregnancy complications and procedures, including:
- Macrosomia. This means your baby weighs more than 8 pounds, 13 ounces (4,000 grams) at birth. Babies who weigh this much are more likely to be hurt during labor and birth, and can cause damage to his or her mother during delivery.
- Shoulder dystocia or other birth injuries (also called birth trauma). Complications for birthing parents caused by shoulder dystocia include postpartum hemorrhage (heavy bleeding). For babies, the most common injuries are fractures to the collarbone and arm and damage to the brachial plexus nerves. These nerves go from the spinal cord in the neck down the arm. They provide feeling and movement in the shoulder, arm and hand.
- High blood pressure and preeclampsia. High blood pressure also called hypertension is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy. Preeclampsia is when a pregnant person has high blood pressure and signs that some of their organs, such as the kidneys and liver, may not be working properly.
- Perinatal depression. This is depression that happens during pregnancy or in the first year after having a baby also called postpartum depression. Depression is a medical condition that causes feelings of sadness and a loss of interest in things you like to do. It can affect how you think, feel, and act and can interfere with your daily life.
- Preterm birth. This is birth before 37 weeks of pregnancy. Most women who have gestational diabetes have a full-term pregnancy that lasts between 39 and 40 weeks. However, if there are complications, your health care provider may need to induce labor before your due date. This means your provider will give you medicine or break your water (amniotic sac) to make your labor begin.
- Stillbirth. This is the death of a baby after 20 weeks of pregnancy.
- Cesarean birth also called C-section. This is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. You may need to have a c-section if you have complications during pregnancy, or if your baby is very large also known as macrosomia. Most people who have gestational diabetes can have a vaginal birth. But they’re more likely to have a c-section than people who don’t have gestational diabetes.
Gestational diabetes also can cause health complications for your baby after birth, including:
- Breathing problems, including respiratory distress syndrome. This can happen when babies don’t have enough surfactant in their lungs. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing.
- Jaundice. This is a medical condition in which the baby’s liver isn’t fully developed or isn’t working well. A jaundiced baby’s eyes and skin look yellow.
- Low blood sugar (hypoglycemia)
- Obesity later in life
- Diabetes later in life
What happens during my labor and birth?
When you have gestational diabetes, you’ll be advised to give birth in a hospital. That’s because it’s easier to solve any problems that may happen.
You should also be advised to have your labor induced or a cesarean section if this is the best option for you, before 41 weeks of pregnancy – if you have not had your baby by this time. You may be advised to have your baby earlier than this if there are complications, such as high blood pressure or a big baby.
During your labor and childbirth, your blood sugar levels will be monitored carefully. If your levels aren’t between 4-7mmol/l, you may be given a drip.
What happens straight after my baby is born?
After birth, you and your baby will be carefully looked after. Here’s a few things you can expect to happen:
- Your baby should stay with you unless your healthcare team has any concerns. If there are concerns, they may move your baby to a special unit – called a neonatal unit.
- Your baby will need to be fed soon after birth – within 30 minutes – and then every two to three hours after that.
- Your baby’s blood sugar level will be checked regularly to help stop it from going too low.
- If your baby needs help with their blood sugar levels or they’re not feeding well, they may need a feeding tube or a drip.
- You and your baby will have to stay in hospital for at least 24 hours before you can go home. This is because your healthcare team will need to make sure that your baby’s sugar levels are OK and that they are feeding well.
I’ve had my baby. What now?
Most women’s blood sugar levels go back to normal after their labor. So, if you’re taking diabetes medication, including insulin, it will be stopped straight after birth. But, in some cases, pregnancy uncovers pre-existing diabetes also called pregestational diabetes (see below), so some women will need to carry on with their treatment.
After having gestational diabetes, you’re at an increased risk of developing it in future pregnancies, so you should be offered testing for diabetes when planning future pregnancies. You’re also more likely to develop type 2 diabetes in later life.
To reduce your risk:
- Make sure your blood sugar levels are checked regularly, including a test between 6 and 13 weeks after you’ve given birth and then an annual test to check your blood sugar levels are normal.
- Look out for the signs and symptoms of diabetes and arrange to see your doctor if you’re worried.
- During future pregnancies, tell your healthcare team that you have a history of gestational diabetes. You should be offered a blood glucose monitor to carry out early self-monitoring at home or an Oral Glucose Tolerance Test (OGTT). If the results from your first OGTT are normal, you should be offered a follow up test later in your pregnancy.
- Take steps to manage your weight, make healthier food choices and keep up your physical activity. This will help to reduce your risk future risk of developing gestational diabetes again or type 2 diabetes in the future.
Breastfeeding and your blood sugar levels
If you want to breastfeed, there’s no reason why you can’t. Breastfeeding is good for you and good for your baby. Breastmilk contains a type of sugar called lactose. Every time you feed your baby, you lose sugar. This means your blood sugar levels drop. This can mean that you need up to 25% less insulin if you’re breastfeeding.
It can also mean that you’re more likely to have a low blood sugar level (hypoglycemia) during feeding, especially if you take insulin to treat your diabetes. It’s a good idea to have a snack close by when you’re breastfeeding, and have something to treat a low blood sugar level (hypoglycemia) handy.
Pregnancy and type 2 diabetes
Preexisting diabetes also called pregestational diabetes means you have diabetes before you get pregnant. This is different from gestational diabetes, which is a kind of diabetes that some women get during pregnancy. In the United States, about 1 to 2 percent of pregnant women have preexisting diabetes. The number of women with diabetes during pregnancy has increased in recent years. High blood sugar can be harmful to your baby during the first few weeks of pregnancy when his brain, heart, kidneys and lungs begin to form. There is a chance that some of the potential complications of diabetes, like eye disease (diabetic retinopathy) and kidney disease (diabetic nephropathy), may develop while you are pregnant. Your doctors will keep an eye on this. If you are pregnant or planning a pregnancy, visit an ophthalmologist during each trimester of your pregnancy, one year postpartum or as advised. There is also a risk of developing pre-eclampsia, a condition involving high blood pressure during pregnancy, which can cause problems for the baby.
If you have type 1 or type 2 diabetes and are planning a family, you should plan your pregnancy as much as possible. Controlling your blood sugars before conception and throughout pregnancy gives you the best chance of having a trouble-free pregnancy and birth and a healthy baby. Most women with diabetes have a healthy baby.
Having diabetes means that you and your baby are more at risk of serious health complications during pregnancy and childbirth. The good news is that by planning ahead and getting support from your doctor and diabetes team, you can really reduce the risks involved. So you’re more likely to enjoy a healthy pregnancy and give birth to a healthy baby.
If you have diabetes and your pregnancy is unplanned, there’s still plenty you can do to give your baby the best start in life.
Women with type 2 diabetes will likely need to change their treatment plans and adhere to diets that carefully controls carbohydrate intake. Many women will need insulin therapy during pregnancy and may need to discontinue other treatments, such as blood pressure medications.
Signs of trouble
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of signs and symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar (hyperglycemia). Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Signs and symptoms include:
- Frequent urination
- Increased thirst
- Dry mouth
- Blurred vision
- Fatigue
- Headache
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L). Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Signs and symptoms of hyperglycemic hyperosmolar nonketotic syndrome (HHNS) include:
- Dry mouth
- Extreme thirst
- Drowsiness
- Confusion
- Dark urine
- Seizures
Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medications — including the diabetes medications called SGLT2 inhibitors.
Although diabetic ketoacidosis is usually less severe in type 2 diabetes, the toxicity of the acids can be life-threatening. In addition to the signs and symptoms of low blood sugar (hypoglycemia), such as frequent urination and increased thirst, ketoacidosis may result in:
- Nausea
- Vomiting
- Abdominal pain
- Shortness of breath
- Fruity-smelling breath
Low blood sugar (hypoglycemia). If your blood sugar level drops below your target range, it’s known as low blood sugar (hypoglycemia). Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physical activity than usual. Signs and symptoms include:
- Sweating
- Shakiness
- Weakness
- Hunger
- Irritability
- Dizziness
- Headache
- Blurred vision
- Heart palpitations
- Slurred speech
- Drowsiness
- Confusion
If you have signs or symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level — fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, repeat the sugar intake. Eat a meal after levels return to normal.
If you lose consciousness, you will need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
Gestational diabetes causes
Scientists believe gestational diabetes, a type of diabetes that develops during pregnancy, is caused by the hormonal changes of pregnancy along with genetic and lifestyle factors.
When you are pregnant, your placenta produces hormones to help your baby grow. Pregnancy hormones you produce block the action of insulin in your body (called insulin resistance). This puts you at an increased risk of insulin resistance, and some women can’t produce enough insulin to overcome it. This makes it difficult to use glucose (sugar) properly for energy, so it stays in your blood and the sugar levels rise. This then leads to gestational diabetes.
- Insulin resistance: Hormones produced by the placenta contribute to insulin resistance, which occurs in all women during late pregnancy. Most pregnant women can produce enough insulin to overcome insulin resistance, but some cannot. Gestational diabetes occurs when the pancreas can’t make enough insulin.
- Extra weight is linked to gestational diabetes. Women who are overweight or obese may already have insulin resistance when they become pregnant. Gaining too much weight during pregnancy may also be a factor.
- Genes and family history: Having a family history of diabetes makes it more likely that a woman will develop gestational diabetes, which suggests that genes play a role. Genes may also explain why the disorder occurs more often in African Americans, American Indians, Asians, and Hispanics/Latinas.
You are at higher risk of developing gestational diabetes if you:
- are overweight or obese (your body mass index (BMI) is above 30) and not physically active or gaining too much weight in the first half of pregnancy
- are over the age of 35 years
- have a family history (parent, brother or sister) of type 2 diabetes
- come from a racial or ethnic group that has a higher prevalence of diabetes that isn’t entirely explained by race or ethnicity, such as Black, American Indian, Alaska Native, Asian, Hispanic/Latino or Pacific Islander
- have had gestational diabetes before
- have prediabetes. This means your blood glucose levels are higher than normal but not high enough to be diagnosed with diabetes.
- have had polycystic ovary syndrome (PCOS). This is a hormone problem that can affect reproductive and overall health.
- have had a large baby (macrosomia) in a past pregnancy
- are taking some types of anti-psychotic or steroid medications
- have high blood pressure or you’ve had heart disease
- you have had a gastric bypass or other weight-loss surgery
Risk factors for gestational diabetes
You may be more likely than other women to develop gestational diabetes if:
- You’re older than 35.
- You’re overweight or obese and not physically active.
- You had gestational diabetes or a very large baby (~ 4.5kg/10lb or more) in a previous pregnancy (baby with macrosomia in a past pregnancy).
- You have high blood pressure or you’ve had heart disease.
- You have had a gastric bypass or other weight-loss surgery
- You have polycystic ovarian syndrome (also called polycystic ovary syndrome or PCOS). This is a hormone imbalance that can affect a women’s reproductive and overall health.
- You have prediabetes. This means your blood glucose levels are higher than normal but not high enough to be diabetes.
- You have a family history of diabetes – a parent, brother or sister who has diabetes.
- You have a Asian, South Asian, African-American or African Caribbean, Middle Eastern, Native American, Hispanic or Pacific Islander background.
However, even women without any of these risk factors can develop gestational diabetes. This is why your health care provider tests you for gestational diabetes during your pregnancy.
Gestational diabetes prevention
Gestational diabetes is common. It affects at least 4–7 in 100 women during pregnancy. Some women have a higher risk of developing it. Most pregnant women get tested for gestational diabetes at 24 to 28 weeks of pregnancy.
You can’t prevent it but there are some things you can do to reduce your risk. This includes managing your weight, eating healthily and keeping active before pregnancy.
Gestational diabetes usually goes away after your baby is born.
Gestational diabetes signs and symptoms
Many women with gestational diabetes have no noticeable symptoms.
Signs and symptoms associated with gestational diabetes (when your blood sugar levels gets too high [hyperglycemia]) include:
- Going to the toilet a lot, especially at night.
- Being really thirsty.
- Dry mouth.
- Feeling more tired than usual.
- Losing weight without trying to.
- Genital itching or thrush.
- Blurred eyesight.
As some of the signs of diabetes are like symptoms experienced in pregnancy anyway – like feeling more tired or going to the toilet more – most gestational diabetes cases are diagnosed during screening for gestational diabetes. This is called a Glucose Tolerance Test, also known as an Oral Glucose Tolerance Test (OGTT).
The Oral Glucose Tolerance Test (OGTT) is done when you’re between 24-28 weeks pregnant. If you’ve had gestational diabetes before, you’ll be offered the OGTT or self monitoring of your blood sugar levels at home early in your pregnancy. You’ll be shown how to do this and given a blood monitoring kit.
Gestational diabetes complications
Most women who have gestational diabetes deliver healthy babies. However, untreated or uncontrolled blood sugar levels can cause problems for you and your baby.
Complications in your baby can be caused by gestational diabetes, including:
- Excess growth also known as macrosomia. Extra glucose can cross the placenta. Extra glucose triggers the baby’s pancreas to make extra insulin. This can cause your baby to grow too large. It can lead to a difficult birth and sometimes the need for induced labor or a cesarean section (C-section).
- Low blood sugar (hypoglycemia). Sometimes babies of mothers with gestational diabetes develop low blood sugar (hypoglycemia) shortly after birth. This is because their own insulin production is high.
- Yellowing of the skin and eyes (newborn jaundice) after he or she is born, which may require treatment in hospital
- Type 2 diabetes later in life. Babies of mothers who have gestational diabetes have a higher risk of developing obesity and type 2 diabetes later in life.
- Death. Untreated gestational diabetes can lead to a baby’s death either before or shortly after birth.
Complications in the mother also can be caused by gestational diabetes, including:
- Preeclampsia. Symptoms of this condition include high blood pressure, too much protein in the urine, and swelling in the legs and feet. Pre-eclampsia can lead to pregnancy complications if not treated.
- Gestational diabetes. If you had gestational diabetes in one pregnancy, you’re more likely to have it again with the next pregnancy.
- Polyhydramnios – too much amniotic fluid (the fluid that surrounds your baby) in the womb, which can cause premature labor or problems at delivery
- Premature birth – giving birth before the 37th week of pregnancy
Having gestational diabetes also means you’re at an increased risk of developing type 2 diabetes in the future.
Gestational diabetes diagnosis
Doctors use blood tests to diagnose gestational diabetes. Gestational diabetes testing is offered between the 24th and 28th weeks of pregnancy. Your doctor tests you for gestational diabetes with a prenatal test called a glucose challenge test (glucose screening test), the Oral Glucose Tolerance Test (OGTT), or both. In the United States, the two-step test is more commonly used. These tests show how well your body uses glucose.
Gestational diabetes test
The American College of Obstetricians and Gynecologists (ACOG) and the National Institutes of Health (NIH) consensus conference currently recommend the two-step approach, while the Endocrine Society recommends the one-step approach, and the American Diabetes Association (ADA) says either the one-step or two-step approach is appropriate 3.
- Step one of a two-step test is also called a glucose challenge test or glucose screening test. In step one, you will drink a solution with glucose and then have your blood glucose levels checked after one hour. If your blood glucose level is within the range expected for healthy people, your testing will be complete, and you will not need to perform step two. If your blood glucose level is higher than normal, you will need to return for step two.
- Step two is called a glucose tolerance test or Oral Glucose Tolerance Test (OGTT), and it is administered over three hours. For this test, you will need to go without eating or drinking anything but water for eight hours prior to the test. The glucose tolerance test begins with a blood draw to determine your baseline glucose level. Next, you will drink a solution containing even more glucose than in the solution from step one. Afterward, you will have three additional blood draws that are taken once per hour over three hours. Each blood sample will be tested for its glucose level.
Your test preparation depends on whether a one-step or two-step glucose tolerance test is done.
- One-step 2-hour oral glucose tolerance test (OGTT): you will need to fast (usually overnight for eight hours prior to the test) before an initial blood sample is drawn. You will then be given a 75-gram dose of glucose to drink and your blood will be drawn at 1 hour and 2 hours after the dose. Only one of the values (including the fasting glucose level) needs to be above a cutoff value for diagnosis of diabetes to be made.
- Two-step oral glucose tolerance test:
- Glucose challenge test or glucose screening test: you do not need to fast. You will be given a 50-gram glucose dose to drink and your blood is drawn after 1 hour.
- If the challenge test is abnormal, a 3-hour oral glucose tolerance test (OGTT) will be performed. You will need to fast before an initial blood sample is drawn. Then you will be given a 100-gram glucose dose and your blood drawn at 1 hour, 2 hours, and 3 hours after the dose. If at least 2 of the glucose levels at fasting, 1 hour, 2 hours, or 3 hours are above a certain level, then a diagnosis of gestational diabetes is made.
Gestational diabetes testing is offered between the 24th and 28th weeks of pregnancy. However, your doctor may recommend that you get tested sooner if you have an increased risk of developing gestational diabetes. Some of the risk factors for gestational diabetes include:
- Becoming pregnant after the age of 25
- Being overweight before becoming pregnant or gaining a large amount of weight during pregnancy
- Having family members with diabetes
- Having prediabetes, which is an elevated level of blood glucose that can lead to diabetes
- Having had gestational diabetes during a previous pregnancy
- Belonging to certain racial or ethnic groups, including people who are Black or African American, American Indian or Native American, Latino/Latina, Asian, or Pacific Islander
- Previously giving birth to a baby who weighed 9 pounds or more
- Having a hormonal condition called polycystic ovary syndrome (PCOS)
- Having high blood pressure
- Having a large amount of amniotic fluid, which is the fluid that surrounds the baby in the uterus
You can discuss your risk factors and chance of gestational diabetes with your doctor. Your doctor will be able to advise you on the timing and appropriateness of testing in your specific situation.
One-Step Test
In the 2011 Standards of Care 4, the American Diabetes Association for the first time recommended that all pregnant women not known to have prior diabetes undergo a 75-g oral glucose tolerance test (OGTT) at 24–28 weeks of gestation, based on a recommendation of the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) 5. The the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) defined diagnostic cut points for gestational diabetes as the average glucose values (fasting, 1-hour, and 2-hours plasma glucose) in the HAPO study at which odds for adverse outcomes reached 1.75 times the estimated odds of these outcomes at the mean glucose levels of the study population. This one-step strategy was anticipated to significantly increase the incidence of gestational diabetes (from 5–6% to 15–20%), primarily because only one abnormal value, not two, became sufficient to make the diagnosis. The American Diabetes Association recognized that the anticipated increase in the incidence of gestational diabetes would have significant impact on the costs, medical infrastructure capacity, and potential for increased “medicalization” of pregnancies previously categorized as normal, but recommended these diagnostic criteria changes in the context of worrisome worldwide increases in obesity and diabetes rates with the intent of optimizing gestational outcomes for women and their offspring.
The expected benefits to these pregnancies and offspring are inferred from intervention trials that focused on women with lower levels of hyperglycemia than identified using older gestational diabetes diagnostic criteria and that found modest benefits including reduced rates of large-for-gestational-age births and preeclampsia 6, 7. It is important to note that 80–90% of women being treated for mild gestational diabetes in two randomized controlled trials (whose glucose values overlapped with the thresholds recommended by the IADPSG) could be managed with lifestyle therapy alone. Data are lacking on how the treatment of lower levels of hyperglycemia affects a mother’s risk for the development of type 2 diabetes in the future and her offspring’s risk for obesity, diabetes, and other metabolic dysfunction. Additional well-designed clinical studies are needed to determine the optimal intensity of monitoring and treatment of women with gestational diabetes diagnosed by the one-step strategy.
Two-Step Test
In 2013, the National Institutes of Health (NIH) convened a consensus development conference on diagnosing gestational diabetes. The 15-member panel had representatives from obstetrics/gynecology, maternal-fetal medicine, pediatrics, diabetes research, biostatistics, and other related fields to consider diagnostic criteria 8. The panel recommended the two-step approach of screening with a 1-hour 50-g glucose load test (GLT) followed by a 3-hours 100-g OGTT for those who screen positive, a strategy commonly used in the U.S.
Key factors reported in the National Institutes of Health (NIH) panel’s decision-making process were the lack of clinical trial interventions demonstrating the benefits of the one-step strategy and the potential negative consequences of identifying a large new group of women with gestational diabetes, including medicalization of pregnancy with increased interventions and costs. Moreover, screening with a 50-g glucose load test does not require fasting and is therefore easier to accomplish for many women. Treatment of higher threshold maternal hyperglycemia, as identified by the two-step approach, reduces rates of neonatal macrosomia, large-for-gestational-age births 9 and shoulder dystocia, without increasing small-for-gestational-age births. The American College of Obstetricians and Gynecologists (ACOG) updated its guidelines in 2013 and supported the two-step approach 10.
The conflicting recommendations from expert groups underscore the fact that there are data to support each strategy. The decision of which strategy to implement must therefore be made based on the relative values placed on factors that have yet to be measured (e.g., cost–benefit estimation, willingness to change practice based on correlation studies rather than clinical intervention trial results, relative role of cost considerations, and available infrastructure locally, nationally, and internationally).
As the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) criteria have been adopted internationally, further evidence has emerged to support improved pregnancy outcomes with cost savings 11 and may be the preferred approach. In addition, pregnancies complicated by gestational diabetes per IADPSG criteria, but not recognized as such, have comparable outcomes to pregnancies diagnosed as gestational diabetes by the more stringent two-step criteria 12. There remains strong consensus that establishing a uniform approach to diagnosing gestational diabetes will benefit patients, caregivers, and policymakers. Longer-term outcome studies are currently under way.
Glucose Challenge Test
You may have the glucose challenge test first also known as glucose screening test. In this test, a health care professional will draw your blood 1 hour after you drink a sweet liquid containing glucose. You do not need to fast for this test. Fasting means having nothing to eat or drink except water. If your blood glucose is too high, 140.4 mg/dL (7.8 mmol/L) or more, you may need to return for an oral glucose tolerance test (OGTT) while fasting. If your blood glucose is 200 mg/dL (11.1 mmol/L) or more, you may have type 2 diabetes.
Glucose tolerance test pregnancy (OGTT)
The Oral Glucose Tolerance Test (OGTT) measures blood glucose after you fast for at least 8 hours. First, a health care professional will draw your blood. Then you will drink the liquid containing glucose. You will need your blood drawn every hour for 2 to 3 hours for a doctor to diagnose gestational diabetes. Your health care professional may recommend an OGTT without first having the glucose challenge test.
High blood glucose levels at any two or more blood test times—fasting, 1 hour, 2 hours, or 3 hours—mean you have gestational diabetes. Your health care team will explain what your OGTT results mean. Note that different diagnostic criteria will identify different degrees of maternal hyperglycemia and maternal/fetal risk, leading some experts to debate, and disagree on, optimal strategies for the diagnosis of gestational diabetes 3.
The Oral Glucose Tolerance Test (OGTT) results are interpreted as follows:
Table 1. Gestational Diabetes One-Step Approach test results (OGTT only)
| Time of sample collection | Glucose level |
|---|---|
| Fasting | Equal to or greater than 92 mg/dL (5.1 mmol/L) |
| 1 hour | Equal to or greater than 180 mg/dL (10.0 mmol/L) |
| 2 hour | Equal to or greater than 153 mg/dL (8.5 mmol/L) |
Footnote: Samples drawn fasting and then 1 hour and 2 hours after a 75-gram glucose drink. Diagnosis of gestational diabetes is made when any of the values meet or exceed the limit.
[Source 3 ]Table 2. Gestational Diabetes Two-Step Approach: Step One (Glucose Challenge Screen) test results
| Glucose Level | Interpretation |
|---|---|
| Less than 140* mg/dL (7.8 mmol/L) | Normal screen |
| 140* mg/dL (7.8 mmol/L) or greater | Abnormal, needs OGTT (see Step Two below) |
Footnote: Sample drawn 1 hour after a 50-gram glucose drink. *Some experts recommend a cutoff of 130 mg/dL (7.2 mmol/L) because that identifies 90% of women with gestational diabetes, compared to 80% identified using the threshold of 140 mg/dL (7.8 mmol/L). The American College of Obstetricians and Gynecologists (ACOG) recommends a lower threshold of 135 mg/dL (7.5 mmol/L) in high-risk ethnic groups with higher prevalence of gestational diabetes.
[Source 3 ]Table 3. Gestational Diabetes Two-Step Approach: Step Two (Diagnostic OGTT) test results
| Time of sample collection | Target levels** |
|---|---|
| Fasting (prior to glucose load) | 95 mg/dL (5.3 mmol/L) |
| 1 hour after glucose load | 180 mg/dL (10.0 mmol/L) |
| 2 hours after glucose load | 155 mg/dL (8.6 mmol/L) |
| 3 hours after glucose load | 140 mg/dL (7.8 mmol/L) |
Footnote: **Some labs may use different numbers. Samples drawn at fasting and then 1, 2 and 3 hours after a 100-gram glucose drink. If two or more values meet or exceed the target level, gestational diabetes is diagnosed.
[Source 3 ]Gestational diabetes treatment
If you have gestational diabetes, your prenatal care provider wants to see you more often at prenatal care checkups so she can monitor you and your baby closely to help prevent problems. At each checkup, you get tests to make sure you and your baby are doing well. Tests include a nonstress test and a biophysical profile. The nonstress test checks your baby’s heart rate. The biophysical profile is a nonstress test with an ultrasound. An ultrasound uses sound waves and a computer screen to show a picture of your baby in the womb.
Your prenatal care provider also may ask you to do kick counts (also called fetal movement counts). This is way for you to keep track of how often your baby moves in the womb. Here are two ways to do kick counts:
- Every day, time how long it takes for your baby to move ten times. If it takes longer than 2 hours, tell your prenatal care provider.
- See how many movements you feel in 1 hour. Do this three times each week. If the number changes, tell your prenatal care provider.
If you have gestational diabetes, your prenatal care provider tells you how often to check your blood sugar, what your levels should be and how to manage them during pregnancy. Blood sugar is affected by pregnancy, what you eat and drink, how much physical activity you get. You may need to eat differently and be more active.
American Diabetes Association recommended daily target blood glucose levels for most women with gestational diabetes are 1, 2:
- Before a meal, at bedtime, and overnight: 95 mg/dL (5.3 mmol/L) or less
- One hour after a meal: 140 mg/dL (7.8 mmol/L) or less
- Two hours after a meal: 120 mg/dL (6.7 mmol/L) or less
Ask your doctor what targets are right for you. Your healthcare team will also talk to you about how often to test your blood sugar level, how to do it properly and how to safely meet your targets. You and your care team should also agree an ideal target blood sugar level that’s right for you, and is manageable without causing low blood sugar levels or hypoglycemia.
For many women with gestational diabetes, an important part of managing diabetes — as well as your overall health — is maintaining a healthy weight through a healthy diet and exercise plan. Eating a healthy diet that is high in fiber and low in carbohydrates and getting regular exercise may be enough to lower blood glucose levels. However, some women may need to take insulin shots and/or a diabetes medication called metformin.
Treatment for gestational diabetes can help reduce your risk for pregnancy complications. Your prenatal care provider begins treatment with monitoring your blood sugar levels, healthy eating and physical activity. If this doesn’t do enough to control your blood sugar, you may need medicine. Insulin is the most common medicine for gestational diabetes. It’s safe to take during pregnancy.
Here’s what you can do to help manage gestational diabetes:
- Go to all your prenatal care checkups, even if you’re feeling fine.
- Follow your prenatal care provider’s directions about how often to check your blood sugar. Your prenatal care provider shows you how to check your blood sugar on your own. She tells you how often to check it and what to do if it’s too high. Keep a log that includes your blood sugar level every time you check it. Share the log with your prenatal care provider at each checkup. Most women can check their blood sugar four times each day: once after fasting (first thing in the morning before you’ve eaten) and again after each meal.
- Eat healthy foods. Eat three regular meals and two to three snacks each day. Have one of the snacks at night. Talk to your prenatal care provider about the right kinds of foods to eat to help control your blood sugar.
- Do something active every day. Try to get 30 minutes of moderate-intensity activity at least 5 days each week. Talk to your prenatal care provider about activities that are safe during pregnancy, like walking. Walk for 10 to 15 minutes after each meal to help control your blood sugar.
- If you take medicine for diabetes, take it exactly as your prenatal care provider tells you to. If you take insulin, your prenatal care provider teaches you how to give yourself insulin shots. Tell your prenatal care provider about any medicine you take, even medicine that’s not related to gestational diabetes. Some medicines can be harmful during pregnancy, so your prenatal care provider may need to change them to ones that are safer for you and your baby. Don’t start or stop taking any medicine during pregnancy without talking to your prenatal care provider first.
- Check your weight gain during pregnancy. Gaining too much weight or gaining weight too fast can make it harder to manage your blood sugar. Talk to your prenatal care provider about the right amount of weight to gain during pregnancy.
Exercise
Everyone needs regular aerobic exercise, and people who have diabetes are no exception. Exercise lowers your blood sugar level by moving sugar into your cells, where it’s used for energy. Exercise also increases your sensitivity to insulin, which means your body needs less insulin to transport sugar to your cells. Moderate intensity physical activity — physical activity that raises your breathing or heart rate — can help you manage your blood glucose levels and reduces insulin resistance. The best form of exercise if you have gestational diabetes is to build walking into your daily routine. Always check with your doctor first before you start exercising while you are pregnant.
Aim for at least 30 minutes or more of aerobic exercise most days of the week, or at least 150 minutes of moderate physical activity a week. Bouts of activity can be as brief as 10 minutes, three times a day. If you haven’t been active for a while, start slowly and build up gradually. It’s also a good idea to avoid sitting for too long — aim to get up and move if you’ve been sitting for more than 30 minutes.
Medication
If your blood sugar levels remain high despite changes to your diet and an exercise regime, you may need medication to lower your blood sugar levels.
Both insulin injections and metformin pills have been shown to be safe for the unborn baby. Insulin is the first-line agent recommended for treatment of gestational diabetes in the U.S. 1. Individual randomized controlled trials support the efficacy and short-term safety of metformin 13, 14. If you already have diabetes when you become pregnant, discuss with your doctor whether you will need to change any of your medicines.
If you are worried about taking medicines while you are pregnant, discuss the risks with your doctor. Remember, the risks of not treating your gestational diabetes could be much higher for both you and your baby.
Gestational diabetes diet
Contrary to popular perception, there’s no specific diabetes diet. But the foods you eat not only make a difference to how you manage your diabetes, but also to how well you feel and how much energy you have. If you are diagnosed with gestational diabetes you should be referred to a dietitian for individual advice. If this has not happened ask your maternity care team to refer you.
Understanding your diet and eating healthily is an important part of your treatment for gestational diabetes. It will help you keep your blood sugar levels in the safe range so you’re more likely to enjoy a healthy pregnancy and give birth to a healthy baby.
These healthy eating tips for women with gestational diabetes are general. Your care team should talk to you about making changes to your diet and refer you to a dietitian for individual advice that’s right for you.
Healthy eating means eating more fruits, vegetables, lean proteins and whole grains — foods that are high in nutrition and fiber and low in fat and calories — and cut down on saturated fats, refined carbohydrates and sweets. In fact, it’s the best eating plan for the entire family. Sugary foods are OK once in a while, as long as they’re counted as part of your meal plan. Yet, understanding what and how much to eat can be a challenge. A registered dietitian can help you create a meal plan that fits your health goals, food preferences and lifestyle. This will likely include carbohydrate counting, especially if you have gestational diabetes or use insulin as part of your treatment.
1. Choose healthier carbohydrates (carbs)
All carbs or carbohydrates affect your blood sugar levels, so you need to know which foods contain carbs. The type and amount of carbs you eat or drink makes a difference to your blood sugar levels. The amount makes the biggest difference. And your dietitian may talk to you about reducing your carb portion sizes. It’s important too, to choose healthier carbs.
Easy swaps for healthier carbs:
- Swap white bread for multigrain, wholegrain, wholemeal, rye, linseed or pumpernickel.
- Swap chapatti and roti made with white flour to those made with wholemeal flour.
- Swap white pittas for brown pittas.
- Swap chips and mash for wholemeal pasta, baked plantain or sweet potato.
- Swap white rice for brown rice.
- Swap cereals like Cornflakes and Rice Krispies for Weetabix, Branflakes, Shredded Wheat (or supermarket brand ones) or porridge
You can check food labels when you’re looking for foods high in fiber if you’re unsure.
2. Cut down on sugar
Cutting down sugar can be really hard at the beginning, so small practical swaps are a good starting point.
Easy ways to cut down on excess sugar:
- Swap sugary drinks, energy drinks and fruit juices with water, plain skimmed or semi-skimmed milk, or decaffeinated tea and coffee.
- Try low or zero-calorie sweeteners, also known as artificial sweeteners, instead of using sugar.
- Have fewer foods like cakes, chocolates, ice cream and biscuits.
- Know the other names for sugar on the food label. These are sucrose, glucose, dextrose, fructose, lactose, maltose, honey, invert sugar, syrup, corn sweetener and molasses.
3. Perfect your portion sizes
It isn’t always easy to get portion sizes right, and it can make managing your weight and blood glucose levels more difficult. Using everyday items and household utensils to get your portion sizes right can be really useful. It’s an easy way to visualize what a portion should look like.
However, everybody’s needs are different so the number of portion sizes you need is individual – and your weight, pregnancy, body composition and activity levels all make a difference. Your dietitian will be able to advise you on the amount of portions that are right for you.
Top tips for managing portion sizes:
- Use smaller plates and bowls to help make your portion sizes look bigger.
- Weigh food if you find it hard to gauge portion sizes. Foods like muesli, pasta and rice can be difficult to get right at first, so try using the same container to measure out certain foods.
- Be mindful of what you’re eating. It takes about 20 minutes before your brain registers that you’re full, so eat slowly, putting your knife and fork down in between mouthfuls.
Starchy food
Starchy food includes rice, pasta, bread and chapattis for energy. Choose wholegrain where possible.
One portion is:
- Cooked rice = 2 heaped tablespoons
- Half a jacket potato = 1 computer mouse
- Breakfast cereal = 3 tablespoons
- Boiled pasta or cooked noodles = 3 heaped tablespoons
Dairy food
Includes milk, cheese and yogurt for calcium, which is essential for strong bones and teeth.
One portion is:
- Semi or skimmed milk = one medium glass (200ml or 1/3 pint)
- Hard cheese = small matchbox (30g)
- Reduced or low-fat cream cheese = two small matchboxes (60g)
- Low-sugar, low-fat fromage frais/yogurt = 125g pot
Meat, fish, eggs, pulses, beans and nuts
These foods are high in protein, essential to build and replace muscle.
One portion is:
- Cooked lean meat (e.g., chicken, beef or pork) = deck of playing cards (60–90g)
- Beans and pulses (e.g., red kidney beans, butter beans, chickpeas or lentils) = 4 tablespoons
- Nuts or peanut butter (unsalted) = golf ball (2 level tablespoons)
- Quorn, tofu or soya = snooker ball (120g)
Fruits
Fruits provide you with important vitamins, minerals and fiber that help protect you against stroke, high blood pressure, heart disease and certain cancers.
One portion is:
- One handful of grapes
- One small glass (150ml) of fruit juice (limit to one portion a day)
- Two small satsumas, clementines or tangerines
- Two medium plums
- Two tinned pineapple rings or 12 chunks in natural juice
- One heaped tbsp raisins, sultanas, currants or dried cranberries
- Seven strawberries
Vegetables
An important source of fiber, minerals and vitamins, and an important part of any five-a-day plan.
One portion is:
- Three heaped tablespoons cooked veg (e.g., carrots, peas, sweetcorn, mixed veg)
- One medium onion
- One large sweet potato
- Two broccoli spears
- One heaped tablespoon tomato purée
- One piece of cucumber (5cm)
- Four large mushrooms or 14 button mushrooms
- Three heaped tablespoons beans or pulses (e.g., kidney beans, chickpeas or lentils)
Foods high in fat and sugar
You can enjoy foods from this group as an occasional treat, but they will add extra calories so it’s best to keep them to a minimum, especially if you are trying to lose weight. However, evidence suggests that pregnancy isn’t the time to be on a really strict diet and you shouldn’t aim to lose weight. But it’s important that your weight is monitored by your care team and you don’t gain too much weight, which could cause problems for you and your baby.
One portion is:
- Butter/margarine = one dice (5g)
- Low fat spread = two dice (10g)
- Unsaturated oil (e.g., sunflower, rapeseed, olive oil) = 1 teaspoon
- Chocolate = one fun size bar
4. Plan for snack attacks
If you do need to snack when you have gestational diabetes, swap cake, biscuits, crisps and chocolate for:
- plain or low sugar yogurt
- unsalted nuts
- seeds, fruit and veg
But watch your portion sizes still – it’ll help you keep an eye on your weight.
5. Avoid diabetic foods
The law has changed and manufacturers are no longer allowed to label food as diabetic or suitable for diabetics. They don’t have any special health benefits, they’re expensive, could still affect your blood sugar and may cause an upset stomach.
6. Understand the glycemic index
The gylcemic index (GI) is a measure of how quickly foods containing carbs affect your blood sugar levels after you eat them. Some foods affect sugars levels quickly and so have a high gylcemic index and others take longer to affect blood sugar levels and so have a low gylcemic index. To help you manage your blood sugar levels, go for carbs with a lower GI. You’ll still need to think about your portion sizes. It’s the amount of carbs in the meal that will affect your blood sugar levels the most. And not all low gylcemic index foods are healthy, so make sure you read food labels and make a healthy choice.
7. Manage your weight
If you gain too much weight in pregnancy it can affect your health and increase your blood pressure. However, evidence suggests that pregnancy isn’t the time to be on a really strict diet and you shouldn’t aim to lose weight. But it’s important that your weight is monitored by your care team and you don’t gain too much weight, which could cause problems for you and your baby.
Making changes to your diet and physical activity levels can help you avoid gaining too much weight. It’ll also help you to keep your blood sugar within a safe range.
It’s important to keep going with your healthier lifestyle after you’ve had your baby and keep to a healthy weight. This will reduce your risk of developing gestational diabetes in future pregnancies. And, it will also help to reduce your future risk of developing type 2 diabetes too.
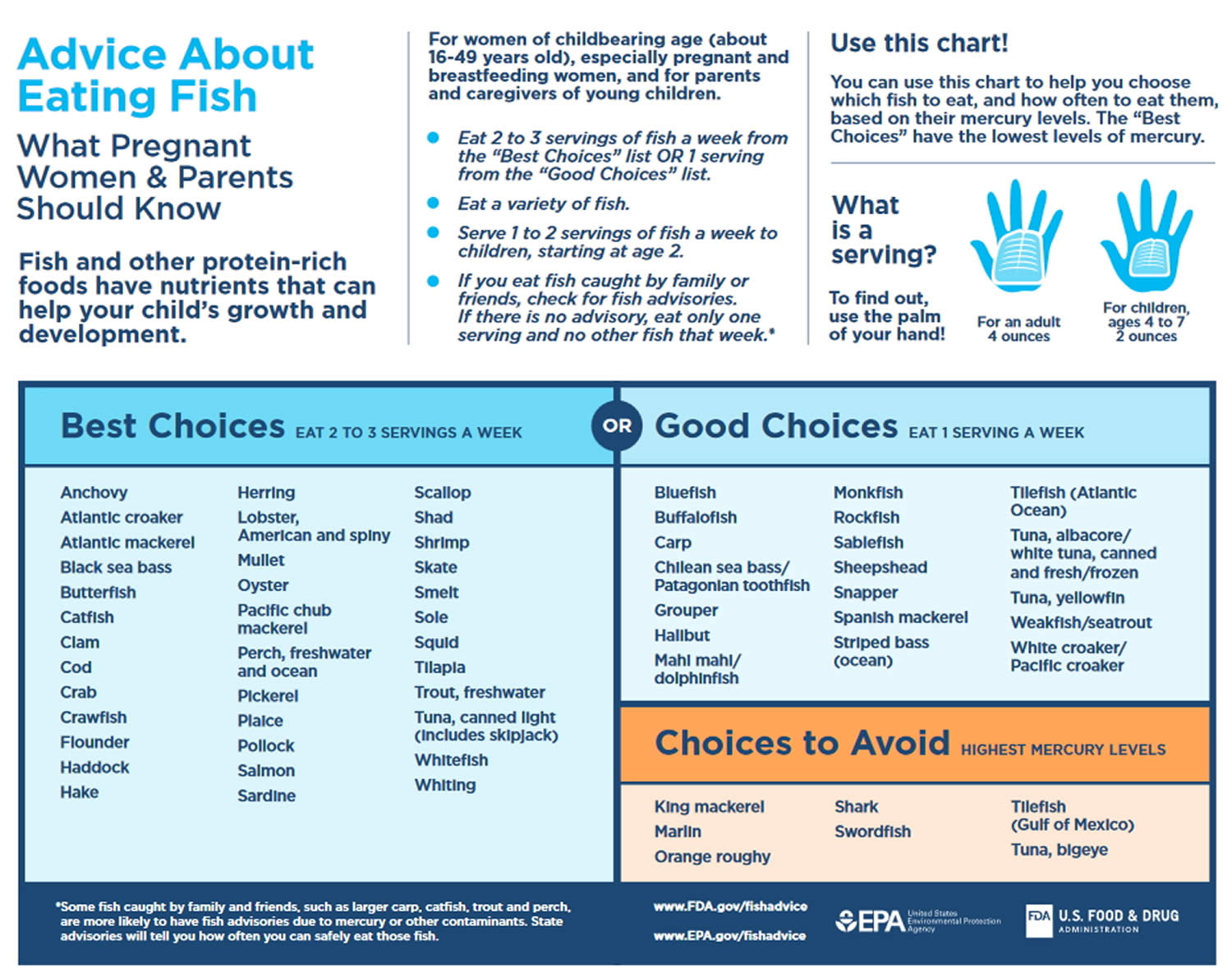
8. Eat more fish
Try to eat fish regularly, as it’s good for you and the development of your baby. The advice is to eat at least two portions a week, including at least one portion of oily fish – like mackerel, sardines, salmon, herrings, trout or pilchards. Oily fish is really good for heart health, but don’t have more than two portions a week because it contains low levels of pollutants (toxins). A portion is about 140g.
Avoid fish which tend to have higher levels of mercury, like swordfish, shark and marlin. And, don’t have more than four medium-sized cans of tuna, or two tuna steaks a week, as it can have relatively high amounts of mercury compared to other fish.
Fruit and vegetables
Fruit and veg are naturally low in calories and packed full of vitamins, minerals and fiber. They also add flavor and variety to every meal. Fruit and vegetables can help protect against stroke, heart disease, high blood pressure and some cancers – and when you have diabetes, you’re more at risk of developing these conditions.
Fruit and vegetables benefits
- Help to keep your digestive system working well
- Help protect the body from heart disease, stroke and some cancers
Examples of what to try:
- sliced melon or grapefruit topped with unsweetened yogurt, or a handful of berries, or fresh dates, apricots or prunes for breakfast
- mix carrots, peas and green beans into your pasta bake
- add an extra handful of peas to rice, spinach to lamb or onions to chicken
- try mushrooms, cucumber, spinach, cabbage, cauliflower, broccoli, celery and lettuce for lower carb vegetable options
- try avocados, blackberries, raspberries, strawberries, plums, peaches and watermelon for lower carb fruit options
Fresh, frozen, dried and canned – they all count. Go for a rainbow of colors to get as wide a range of vitamins and minerals as possible. Try to avoid fruit juices and smoothies as they don’t have as much fiber.
Everyone should aim to eat at least five portions a day. A portion is roughly what fits in the palm of your hand.
Starchy foods
Starchy foods are things like potatoes, rice, pasta, bread, chapattis, naan and plantain. They all contain carbohydrate, which is broken down into glucose and used by our cells as fuel. The problem with some starchy foods is that it can raise blood glucose levels quickly, which can make it harder for you to manage your diabetes. These foods have something called a high glycemic index (GI).
There are some better options for starchy foods – ones that affect blood glucose levels more slowly. These are foods with a low glycemic index (GI), like wholegrain bread, whole-wheat pasta and basmati, brown or wild rice. They also have more fiber, which helps to keep your digestive system working well. So if you’re trying to cut down on carbs, cut down on things like white bread, pasta and rice first.
Starchy foods benefits
- The fiber helps to keep your digestive system healthy
- Some affect your blood sugar levels more slowly
- Wholegrains help protect your heart
Examples of what to try
- two slices of multigrain toast with a bit of spread and Marmite or peanut butter
- brown rice, pasta or noodles in risottos, salads or stir-fries
- baked sweet potato with the skin left on – add toppings like cottage cheese or beans
- boiled cassava, flavored with chilli and lemon
- chapatti made with brown or wholemeal atta.
Proteins
Meat and fish are high in protein, which keeps your muscles healthy. But a healthy diet means less red and processed meat – they’ve been linked to cancer and heart disease. Oily fish like mackerel, salmon and sardines have a lot of omega-3 oil, which can help protect the heart.
Protein foods benefits
- Helps keep your muscles healthy
- Oily fish protects your heart
Aim to have some food from this group every day. Specifically at least 1 or 2 portions of oily fish each week. But you don’t need to eat meat every day.
Examples of what to try
- a small handful of raw nuts and seeds as a snack or chopped with a green salad
- using beans and pulses in a casserole to replace some – or all – of the meat
- eggs scrambled, poached, dry fried or boiled – the choice is yours
- grilled fish with masala, fish pie, or make your own fishcakes
- chicken grilled, roasted or stir-fried
Dairy foods
Milk, cheese and yogurt have lots of calcium and protein in – great for your bones, teeth and muscles. But some dairy foods are high in fat, particularly saturated fat, so choose lower-fat alternatives.
Check for added sugar in lower-fat versions of dairy foods, like yoghurt. It’s better to go for unsweetened yoghurt and add some berries if you want it sweeter. If you prefer a dairy alternative like soya milk, choose one that’s unsweetened and calcium-fortified.
Dairy foods Benefits
- Good for bones and teeth
- Keeps your muscles healthy
Examples of what to try
- a glass of milk straight, flavored with a little cinnamon or added to porridge
- natural or unsweetened yogurt with fruit or on curry
- cottage cheese scooped on carrot sticks
- a bowl of breakfast cereal in the morning, with skimmed or semi-skimmed milk
- a cheese sandwich for lunch, packed with salad
- a refreshing lassi or some plain yogurt with your evening meal
Oils and fats
You need some healthy fat in your diet but you need less saturated fat. This is because some saturated fats can increase cholesterol in your blood, increasing your risk of heart diseases and stroke. These less healthy options are butter, palm nut oil and coconut oil.
Healthier unsaturated fats are foods like olive oil, vegetable oil, rapeseed oil, spreads made from these oils, and nut butters.
Examples of what to try
- A drizzle of olive oil on your salad
- Peanut butter on your wholemeal toast
Avoid foods high in saturated fat, salt and sugar
You don’t need any of these as part of a healthy diet. The less often, the better. But we know you’re bound to eat these foods from time to time, so it’s really important to know how they might affect your body.
These foods include biscuits, crisps, chocolates, cakes, ice cream, butter and sugary drinks. These sugary foods and drinks are high in calories and raise blood sugar levels, so go for diet, light or low-calorie alternatives. And the best drink to choose is water – it’s calorie free.
They’re also high in unhealthy saturated fats, so they aren’t good for cholesterol levels and your heart.
And they can also be full of salt – processed foods especially. Too much salt can make you more at risk of high blood pressure and stroke. You should have no more than 1 tsp (6g) of salt a day.
Experts don’t recommend ‘diabetic’ ice cream or sweets. It’s now against the law to label any food as diabetic and there’s no evidence to suggest that food for diabetics offer any benefits over eating a healthy balanced diet.
Tips for cutting out saturated fat, salt and sugar
- Cook more meals from scratch at home, where you can control the amount of salt you use.
- Check food labels – look for green and orange colors.
- Try unsweetened teas and coffees – they’re better than fruit juices and smoothies as they don’t add any extra calories and carbs.
- Banish the salt shaker from the table – black pepper, herbs and spices are great ways of adding extra flavor to your food.
- Making your own sauces, like tomato ketchup and tandoori marinades.
Gestational diabetes meal plan
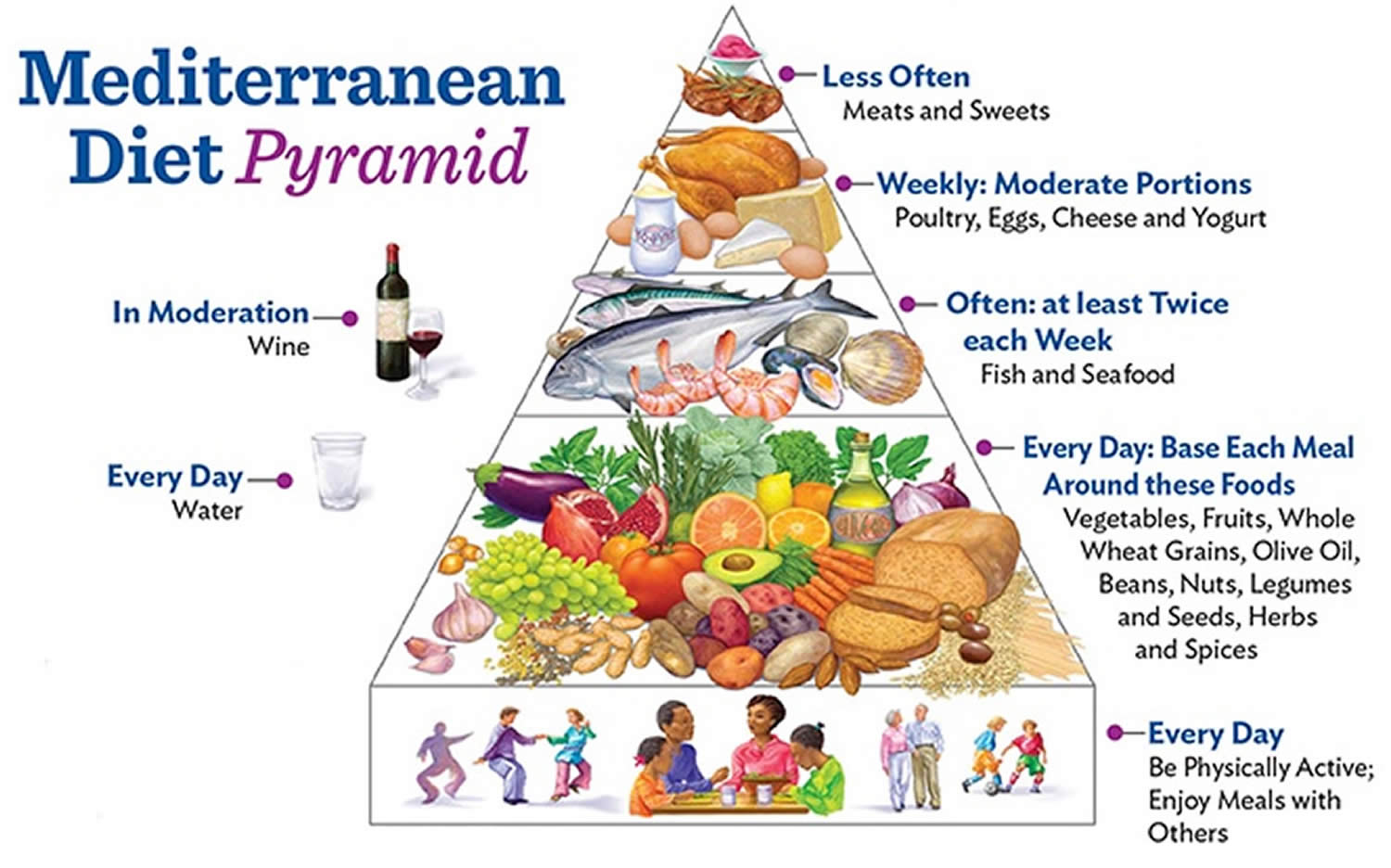
Mediterranean diet
The Mediterranean Diet is a way of eating rather than a formal diet plan. The Mediterranean Diet features foods eaten in more than 20 countries bordering the Mediterranean Sea including Greece, Spain, southern Italy, Portugal, Morocco, Cyprus, Croatia and France and each has their own unique culture and cuisine. In reality there is no “one” Mediterranean Diet 15, which in 2010 was recognized by UNESCO as an intangible cultural heritage of humanity. The “Mediterranean diet” encompasses all of them—it’s not one size fits all 16. Despite regional variations, common components and cultural aspects can be identified, namely olive oil as the main source of lipids, the consumption of large amounts of seasonal vegetables, fruits and aromatic herbs (some of them gathered from the wild), as well as small intakes of meat and fish, often replaced or complemented with pulses, as sources of protein.
A Mediterranean-style diet typically includes:
- plenty of fruits, vegetables, bread and other grains, potatoes, beans, nuts and seeds are eaten daily and make up the majority of food consumed;
- olive oil as a primary fat source, may account for up to 40% of daily calories; and
- small portions of cheese or yogurt are usually eaten each day, along with a serving of fish, poultry, or eggs.
Fish and poultry are more common than red meat in the Mediterranean diet. The Mediterranean diet also centers on minimally processed, plant-based foods. Wine may be consumed in low to moderate amounts, usually with meals. Fruit is a common dessert instead of sweets.
Main meals consumed daily should be a combination of three elements: cereals, vegetables and fruits, and a small quantity of legumes, beans or other (though not in every meal). Cereals in the form of bread, pasta, rice, couscous or bulgur (cracked wheat) should be consumed as one–two servings per meal, preferably using whole or partly refined grains. Vegetable consumption should amount to two or more servings per day, in raw form for at least one of the two main meals (lunch and dinner). Fruit should be considered as the primary form of dessert, with one–two servings per meal. Consuming a variety of colors of both vegetables and fruit is strongly recommended to help ensure intake of a broad range of micronutrients and phytochemicals. The less these foods are cooked, the higher the retention of vitamins and the lower use of fuel, thus minimizing environmental impact.
The Mediterranean Diet is characterized by 17:
- An abundance of plant food (fruit, vegetables, breads, cereals, potatoes, beans, nuts, and seeds);
- Minimally processed, seasonally fresh, locally grown foods;
- Desserts comprised typically of fresh fruit daily and occasional sweets containing refined sugars or honey;
- Olive oil (high in polyunsaturated fat) as the principal source of fat;
- Daily dairy products (mainly cheese and yogurt) in low to moderate amounts;
- Fish and poultry in low to moderate amounts;
- Up to four eggs weekly;
- Red meat rarely; and
- Wine in low to moderate amounts with meals.
Here are some things you can do to switch from a traditional Western-style diet to a more Mediterranean way of eating.
- Dip bread in a mix of olive oil and fresh herbs instead of using butter.
- Add avocado slices to your sandwich instead of bacon.
- Have fish for lunch or dinner instead of red meat. Brush it with olive oil, and broil or grill it.
- Sprinkle your salad with seeds or nuts instead of cheese.
- Cook with olive or canola oil instead of butter or oils that are high in saturated fat.
- Choose whole-grain bread, pasta, rice, and flour instead of foods made with white flour.
- Add ground flaxseed to cereal, low-fat yogurt, and soups.
- Cut back on meat in meals. Instead of having pasta with meat sauce, try pasta tossed with olive oil and topped with pine nuts and a sprinkle of Parmesan cheese.
- Dip raw vegetables in a vinaigrette dressing or hummus instead of dips made from mayonnaise or sour cream.
- Have a piece of fruit for dessert instead of a piece of cake.
- Use herbs and spices instead of salt to add flavor to foods.
A Mediterranean-style diet can help you achieve the American Heart Association’s recommendations for a healthy dietary pattern that:
- emphasizes vegetables, fruits, whole grains, beans and legumes;
- includes low-fat or fat-free dairy products, fish, poultry, non-tropical vegetable oils and nuts; and
- limits added sugars, sugary beverages, sodium, highly processed foods, refined carbohydrates, saturated fats, and fatty or processed meats.
This style of eating can play a big role in preventing heart disease and stroke and reducing risk factors such as obesity, diabetes, high cholesterol and high blood pressure. There is some evidence that a Mediterranean diet rich in virgin olive oil may help the body remove excess cholesterol from arteries and keep blood vessels open.
The traditional Mediterranean dietary pattern is of particular interest to healthcare providers and dietary scientists, because of observations from the 1960s that populations in countries of the Mediterranean region, such as Greece and Italy, had lower mortality from cardiovascular disease compared with northern European populations or the US, probably as a result of different eating habits.
However, adherence to the Mediterranean diet dietary pattern has been rapidly decreasing in the region since 2000, particularly in Greece, Portugal and Spain – due to the wide dissemination of the fast-food culture. These observations point to a nutrition transition period that encompasses considerable changes in diet and physical activity patterns, which may be leading to an increase in the incidence of chronic and degenerative diseases in the Mediterranean region.
Traditionally characterized by vegetables, legumes, beans, fruits, nuts, seeds, olives, lots of extra virgin olive oil, high-fiber breads and whole grains and fish, this way of eating not only involves a low consumption of processed food, processed carbohydrates, sweets, chocolate and red meat. The recommended foods are rich with monounsaturated fats, fiber, and omega-3 fatty acids.
The Mediterranean Diet is associated with a lower incidence of mortality from all-causes 18 and is also related to lower incidence of cardiovascular diseases 19, type 2 diabetes 20, certain types of cancer 21, and neurodegenerative diseases 22. The Mediterranean diet is now recognized as one of the most healthy food patterns in the world.
The Mediterranean diet is like other heart-healthy diets in that it recommends eating plenty of fruits, vegetables, and high-fiber grains. But in the Mediterranean diet, an average of 35% to 40% of calories can come from fat. Most other heart-healthy guidelines recommend getting less than 35% of your calories from fat. The fats allowed in the Mediterranean diet are mainly from unsaturated oils such as fish oils, olive oil, and certain nut or seed oils (such as canola, soybean, or flaxseed oil) and from nuts (walnuts, hazelnuts, and almonds). These types of oils may have a protective effect on the heart.
Mediterranean Diet Food List
There’s no one “Mediterranean diet food list” because there are more than 20 countries bordering the Mediterranean Sea. Diets vary between these countries and also between regions within a country. Many differences in culture, ethnic background, religion, economy and agricultural production result in different diets. But the common Mediterranean dietary meal plan (source 23) has these characteristics:
- High consumption of fruits, vegetables, bread and other cereals, potatoes, beans, nuts and seeds
- Olive oil is an important monounsaturated fat source
- Dairy products, fish and poultry are consumed in low to moderate amounts, and little red meat is eaten
- Eggs are consumed zero to four times a week
- Wine is consumed in low to moderate amounts
Mediterranean Diet Meal Plan:
- Eating a variety of fruits and vegetables each day, such as grapes, blueberries, tomatoes, broccoli, peppers, figs, olives, spinach, eggplant, beans, lentils, and chickpeas.
- Eating a variety of whole-grain foods each day, such as oats, brown rice, and whole wheat bread, pasta, and couscous.
- Choosing healthy (unsaturated) fats, such as nuts, olive oil, and certain nut or seed oils like canola, soybean, and flaxseed. About 35% to 40% of daily calories can come from fat, mainly from unsaturated fats. More than half the fat calories in a Mediterranean diet come from monounsaturated fats (mainly from olive oil). Monounsaturated fat doesn’t raise blood cholesterol levels the way saturated fat does. (source 23).
- Limiting unhealthy (saturated) fats, such as butter, palm oil, and coconut oil. And limit fats found in animal products, such as meat and dairy products made with whole milk.
- Eating mostly vegetarian meals that include whole grains, beans, lentils, and vegetables.
- Eating fish at least 2 times a week, such as tuna, salmon, mackerel, lake trout, herring, or sardines.
- Eating moderate amounts of low-fat dairy products each day or weekly, such as milk, cheese, or yogurt.
- Eating moderate amounts of poultry and eggs every 2 days or weekly.
- Limiting red meat to only a few times a month in very small amounts. For example, a serving of meat is 3 ounces. This is about the size of a deck of cards.
- Limiting sweets and desserts to only a few times a week. This includes sugar-sweetened drinks like soda.
Figure 2. Mediterranean diet meal plan
Gestational diabetes food list
You may worry that having diabetes means going without foods you enjoy. The good news is that you can still eat your favorite foods, but you might need to eat smaller portions or enjoy them less often. Your health care team will help create a diabetes meal plan for you that meets your needs and likes.
The key to eating with diabetes is to eat a variety of healthy foods from all food groups, in the amounts your meal plan outlines.
The food groups are:
- Vegetables
- nonstarchy: includes broccoli, carrots, greens, peppers, and tomatoes
- starchy: includes potatoes, corn, and green peas
- Fruits—includes oranges, melon, berries, apples, bananas, and grapes
- Grains—at least half of your grains for the day should be whole grains
- includes wheat, rice, oats, cornmeal, barley, and quinoa
- examples: bread, pasta, cereal, and tortillas
- Protein
- lean meat
- chicken or turkey without the skin
- fish
- eggs
- nuts and peanuts
- dried beans and certain peas, such as chickpeas and split peas
- meat substitutes, such as tofu
- Dairy—nonfat or low fat
- milk or lactose-free milk if you have lactose intolerance
- yogurt
- cheese
- Heart-healthy fats. Eat foods with heart-healthy fats, which mainly come from these foods:
- oils that are liquid at room temperature, such as canola and olive oil
- nuts and seeds
- heart-healthy fish such as salmon, tuna, and mackerel
- avocado
Use oils when cooking food instead of butter, cream, shortening, lard, or stick margarine.
Foods and drinks to limit include:
- fried foods and other foods high in saturated fat and trans fat
- foods high in salt, also called sodium
- sweets, such as baked goods, candy, and ice cream
- beverages with added sugars, such as juice, regular soda, and regular sports or energy drinks
Drink water instead of sweetened beverages. Consider using a sugar substitute in your coffee or tea.
If you drink alcohol, drink moderately—no more than one drink a day if you’re a woman or two drinks a day if you’re a man. If you use insulin or diabetes medicines that increase the amount of insulin your body makes, alcohol can make your blood glucose level drop too low. This is especially true if you haven’t eaten in a while. It’s best to eat some food when you drink alcohol.
References- American Diabetes Association; 12. Management of Diabetes in Pregnancy. Diabetes Care 1 January 2016; 39 (Supplement_1): S94–S98. https://doi.org/10.2337/dc16-S015
- Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 2007;30(Suppl. 2):S251–S260
- American Diabetes Association; 2. Classification and Diagnosis of Diabetes. Diabetes Care 1 January 2016; 39 (Supplement_1): S13–S22. https://doi.org/10.2337/dc16-S005
- American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care 2011;34(Suppl. 1):S11–S61
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel; Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, Dyer AR, Leiva Ad, Hod M, Kitzmiler JL, Lowe LP, McIntyre HD, Oats JJ, Omori Y, Schmidt MI. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010 Mar;33(3):676-82. doi: 10.2337/dc09-1848
- Landon MB, Spong CY, Thom E, et al.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 2009;361:1339–1348
- Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS; Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 2005;352:2477–2486
- Vandorsten JP, Dodson WC, Espeland MA, Grobman WA, Guise JM, Mercer BM, Minkoff HL, Poindexter B, Prosser LA, Sawaya GF, Scott JR, Silver RM, Smith L, Thomas A, Tita AT. NIH consensus development conference: diagnosing gestational diabetes mellitus. NIH Consens State Sci Statements. 2013 Mar 6;29(1):1-31.
- Horvath K, Koch K, Jeitler K, Matyas E, Bender R, Bastian H, Lange S, Siebenhofer A. Effects of treatment in women with gestational diabetes mellitus: systematic review and meta-analysis. BMJ. 2010 Apr 1;340:c1395. doi: 10.1136/bmj.c1395
- Practice Bulletin No. 137: Gestational diabetes mellitus. Obstet Gynecol. 2013 Aug;122(2 Pt 1):406-416. doi: 10.1097/01.AOG.0000433006.09219.f1
- Alejandra Duran, Sofía Sáenz, María J. Torrejón, et al.; Introduction of IADPSG Criteria for the Screening and Diagnosis of Gestational Diabetes Mellitus Results in Improved Pregnancy Outcomes at a Lower Cost in a Large Cohort of Pregnant Women: The St. Carlos Gestational Diabetes Study. Diabetes Care 1 September 2014; 37 (9): 2442–2450. https://doi.org/10.2337/dc14-0179
- Ethridge JK Jr, Catalano PM, Waters TP. Perinatal outcomes associated with the diagnosis of gestational diabetes made by the international association of the diabetes and pregnancy study groups criteria. Obstet Gynecol. 2014 Sep;124(3):571-578. doi: 10.1097/AOG.0000000000000412
- Rowan JA, Hague WM, Gao W, Battin MR, Moore MP; MiG Trial Investigators. Metformin versus insulin for the treatment of gestational diabetes. N Engl J Med 2008;358:2003–2015
- Gui J, Liu Q, Feng L. Metformin vs insulin in the management of gestational diabetes: a meta-analysis. PLoS One 2013;8:e64585
- Altomare, R., Cacciabaudo, F., Damiano, G., Palumbo, V. D., Gioviale, M. C., Bellavia, M., Tomasello, G., & Lo Monte, A. I. (2013). The mediterranean diet: a history of health. Iranian journal of public health, 42(5), 449–457. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3684452
- Castro-Quezada, I., Román-Viñas, B., & Serra-Majem, L. (2014). The Mediterranean diet and nutritional adequacy: a review. Nutrients, 6(1), 231–248. https://doi.org/10.3390/nu6010231
- F.B. Hu. The Mediterranean Diet and mortality—olive oil and beyond. N Engl J Med, 348 (2003), pp. 2595-2596
- Sofi F., Macchi C., Abbate R., Gensini G.F., Casini A. Mediterranean diet and health. Biofactors. 2013;39:335–342. doi: 10.1002/biof.1096
- Estruch R., Ros E., Salas-Salvadó J., Covas M.I., Corella D., Arós F., Gómez-Gracia E., Ruiz-Gutiérrez V., Fiol M., Lapetra J., et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303
- Mitrou P.N., Kipnis V., Thiébaut A.C., Reedy J., Subar A.F., Wirfält E., Flood A., Mouw T., Hollenbeck A.R., Leitzmann M.F., et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: Results from the NIH-AARP Diet and Health Study. Arch. Intern. Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461
- Couto E., Boffetta P., Lagiou P., Ferrari P., Buckland G., Overvad K., Dahm C.C., Tjønneland A., Olsen A., Clavel-Chapelon F., et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br. J. Cancer. 2011;104:1493–1499. doi: 10.1038/bjc.2011.106
- Sofi F., Abbate R., Gensini G.F., Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010;92:1189–1196. doi: 10.3945/ajcn.2010.29673
- American Heart Association – Mediterranean Diet – http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Nutrition/Mediterranean-Diet_UCM_306004_Article.jsp