What is kava
Kava also known as ‘kava kava’, kawa, waka, lewena, yaqona, grog (Fiji), sakau (Pohnpei), ‘awa (Hawaii), ‘ava (Samoa) and wati (New Guinea) 1. Kava is the dried rhizome and roots of Piper methysticum, a plant in the black pepper family. Kava is a shrub native to the Pacific Island region and known for its anti-anxiety and sedative properties. Kava has traditionally been cultivated by Pacific Islanders for use as a social and ceremonial drink – either ground or chewed up and mixed with water (or coconut milk). The water is then strained, served in a half coconut shell, and consumed in one mouthful. Kava is used as a means of strengthening social and familial ties, particularly among males, and assisting communication with spirits. Defining features of traditional kava practices in the South Pacific are the restrictions placed on its consumption, including who can drink kava and when. Such limitations usually promote the consumption of kava in a safe and controlled manner. The potency of the kava drink can vary greatly depending on the proportions and potency of kava lactones in the plant variety used, the method of preparation, and the degree of dilution in the preparation process 2. Heavy kava drinkers acquire a reversible ichthyosiform eruption, known as kanikani in Fijian 3.
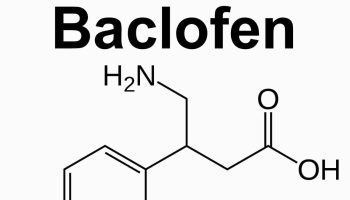
The major chemical constituents of kava are kava lactones (also known as kava pyrones) with the major lactones being kawain (1.8%), methysticin (1.2%), dihydromethysticin (0.5%), emethyoxyyangonin (1.0%), yagonin (1.0%) and dihydrokawain (1.0%). At least 13 other lactones, two chalcones and a number of free aromatic acids are known.
In the United States, kava-containing products are sold as dietary supplements and marketed for the treatment of anxiety, occasional insomnia, premenstrual syndrome, and stress. However, it is not certain whether kava is effective in treating any medical condition. Medicinal use of this product has not been approved by the FDA. Kava should not be used in place of medication prescribed for you by your doctor. Heavy usage results in some adverse effects. Kava contains alkaloids; lactones; kawain, methysticin, mucilage, starch and yangonin. Kava is also the name of the pungent beverage prepared from the plant’s roots.
Kava supplements often are in the form of raw plant material or concentrated extracts, which are obtained by using either acetone or ethanol extraction or cryoprecipitation. Preparations marketed for human consumption contain a mixture of components collectively known as kava pyrones (i.e., kavalactones). Kava-containing products might differ based on the absolute amount of kava pyrones present and on the relative distribution of kava pyrones. Several countries, including Germany, Switzerland, Canada, Australia, and France, have restricted the sale of kava-containing products based on the occurrence of hepatic adverse events and the documented hepatic toxicity following rechallenge with a kava-containing product 4.
FDA has advised consumers and health-care providers about the potential risk for hepatic toxicity associated with the use of kava-containing products 5. Additional caution by persons who have pre-existing liver disease or are at risk for liver disease might be warranted.
Cultivated kava is a dense, leafy green plant that is generally harvested when it is approximately six to eight feet in height. The plants take approximately five to seven years to mature, with a minimum of four years maturity required to produce high quality kava. The constituents of kava are a group of active chemicals known as kava lactones, which are naturally present in the root of the plant. To date, 19 kava lactones have been identified in the kava root, six of which have been described as the major active constituents. The kava lactones produce a number of effects when ingested including: analgesic, sedative, soporific, local anaesthetic, and muscle relaxant 6.
Kava root and underground stem (fresh or dried) are used to prepare drinks; they are also made into extracts, capsules, and tablets. Kava supplements may have a small effect on reducing anxiety, but they have been linked to a risk of severe liver disease. Combining kava with alcohol may increase the risk of liver damage.
Differences in dosages used, preparation methods, and study designs have resulted in mixed conclusions about kava’s usefulness.
Kava is a depressant drug, which means it slows down the messages traveling between your brain and your body. Kava is made from the root or stump of the kava (Piper methysticum) shrub 7.
Kava can affect people differently. Initial effects commonly include:
- feeling happy
- sleepiness
- numbness around the mouth
- reduced or loss of appetite 8
If a larger amount of kava is consumed, effects may also include:
- drowsiness
- nausea
- fever
- bloodshot eyes or dilated pupils.
Long-term use of kava has been associated with a range of health problems including kidney and liver damage, loss of appetite, breathing difficulties and skin lesions.
There is no safe level of kava use. The effects of kava when mixed with other drugs and medicines can be especially unpredictable and dangerous.
Recent research detailing the detrimental health effects of kava consumption is provided by Clough and colleagues 9 in an investigation in an Indigenous community in Arnhem Land. In line with the previous study, it was found that current kava users were more likely than others to experience the following undesirable health effects: kava dermopathy (a rash); low body mass index (BMI); and high cholesterol levels. Kava use was also shown to have a negative impact on the immune system, with current kava users showing greater susceptibility to certain infections. This, with the earlier study by Mathews and colleagues 10, confirm kava use is associated with specific adverse health effects, namely skin rash and weight loss.
FDA Issues Consumer Advisory for Dietary Supplements Containing Kava
On March 25, 2002, the Food and Drug Administration (FDA) issued an advisory notifying consumers that kava-containing dietary supplements may be associated with severe liver injury. The FDA reported that kava-containing products have been associated with liver-related injuries, including hepatitis, cirrhosis, and liver failure, in over 25 reports of adverse events in other countries. In the U.S., FDA received a report of a previously healthy young female who required liver transplantation, as well as several reports of liver-related injuries.
Eight liver transplant cases following liver failure associated with the use of kava-containing products have been reported in Europe (six in Germany and two in Switzerland) 11. Two male patients aged 32 and 50 years and six females aged 22–61 years required liver transplants after using kava-containing products. The duration of kava use ranged from 8 weeks to 12 months. The products were used at doses ranging from 60 mg to 240 mg per day 11. Seven patients used kava prepared either by ethanol or acetone extraction methods; one patient used an unspecified type of kava-containing product. The patients had varying symptoms, including influenza-like symptoms and jaundice. Each patient’s condition worsened and progressed to fulminant hepatic failure. Four of these cases have been reported in medical literature 12, 13, 14, 15. Additional information about these cases is available from the German regulatory authority, the Federal Institute for Drugs and Medical Devices, Bonn, Germany, at https://www.bfarm.de/EN/Home/home_node.html. A ninth European transplant case was reported directly to FDA’s MedWatch System by a U.S. pharmaceutical manufacturer (https://www.fda.gov/Safety/MedWatch/default.htm).
Since 1999, health-care professionals in Germany, Switzerland, and the United States have reported the occurrence of severe hepatic toxicity possibly associated with the consumption of products containing kava (i.e., kava kava or Piper methysticum). A total of 11 patients who used kava products had liver failure and underwent subsequent liver transplantation. On March 25, 2002, in response to five such case reports (four in Europe and one in the United States), the Food and Drug Administration (FDA) issued a consumer advisory and subsequently completed an investigation already underway of a similar U.S. case. This report presents the investigation of the two U.S. cases of liver failure associated with kava-containing dietary supplement products and summarizes the European cases. FDA continues to advise consumers and health-care providers about the potential risk associated with the use of kava-containing products.
Long-term use of high doses of kava has been associated with dry, scaly skin or yellowing of the skin.
Heavy consumption of kava has been associated with heart problems and eye irritation.
Health-care providers should consider questioning patients with evidence of hepatic injury about the use of dietary supplements and herbal products.
Perhaps one of the greatest health concerns regarding kava consumption has been its potential impact on the liver 10. This concern has largely been generated by reports of liver toxicity and liver failure in people using herbal products containing kava 16, 17. Case examples of this have occurred in various countries, most notably Europe, but an isolated case has been recorded in United States. The emergence of such serious health effects from the ingestion of herbal medicines containing kava has since led to the prohibition of kava products in many Western countries. The potential for liver toxicity and liver failure from therapeutically recommended dosages of kava (reported as 840mg kava lactones) raises the question of the impact of recreational kava use on liver functioning 18.
In investigating the relationship between recreational kava use and liver functioning, Clough and colleagues 19 conducted health assessments on men and women from an Arnhem Land community. The participants identified themselves as either current kava users, recent kava users, or non-kava users. The average quantity of powdered kava consumed was reported at 118g per week which equated to approximately 12g of kava lactones a week. Controlling for the effects of alcohol and other substance use, the findings indicated that kava use altered liver functioning with kava users showing abnormally elevated liver enzymes. Of particular interest, however, were the findings that such liver abnormalities abated with the cessation of kava consumption. This suggests that the consumption of powdered kava does negatively impact on liver functioning, but such changes are reversible with abstinence from kava use.
Reports of liver toxicity and liver failure from the ingestion of herbal products containing small quantities of kava together with research showing no lasting liver damage from high dosage rates of recreationaly consumed kava are compelling 19. In an attempt to explain these health disparities, several suggestions have been offered. It is plausible that the practice of using ethanol and acetone to extract the kava lactones used in herbal products contribute to liver problems. This preparation procedure may lead to toxic compounds that do not normally present when kava is prepared using traditional procedures 19. It is also possible that the interplay of other medications and/or herbs may account for liver damage in persons taking herbal products containing kava 17. Some have also suggested genetic differences in liver metabolism may play a role in determining why some individuals develop liver abnormalities from consuming kava and others do not 17. However, in a more recent study by Teschke et al. 20 kava hepatotoxicity has been shown to also occur with traditional aqueous kava extracts of the South Pacific islands and thereby independently from ethanol or acetone as chemical solvents, suggesting that the toxicity is linked to the kava plant itself with a possibly low quality of the used kava cultivar or kava plant part rather than to chemical solvents.
It has been reported that, besides exhibiting hepatotoxicity, kava also possesses photosensitivity and induces dermopathy in humans. In this study, Xia et al. 21 determined that UVA irradiation of kava in the presence of a lipid, methyl linoleate, generated lipid peroxidation which was mediated by singlet oxygen generated during photoirradiation. The six major kavalactones (yangonin, 7,8-dihydrokawa in, kawain, 7,8-dihydromethysticin, methysticin, and 5,6-dehydrokawain) were also studied in parallel; only 5,6-dehydrokawain and yangonin-induced a low level of lipid peroxidation. UVA irradiation of kava in human HaCaT skin keratinocytes induced cytotoxicity which was mediated by oxidative stress, led to DNA strand cleavage, and produced 8-hydroxy-2′-deoxyguanosine (8-OHdG) adduct. Study by the electron spin resonance (ESR) method revealed that UVA irradiation of kava produced singlet oxygen and carbon-centered radicals. The overall results suggest that kava is photocytotoxic and photogenotoxic, both mediated by free radicals generated during photoirradiation 21.
In addition to the negative physical health effects caused by kava use, there is also evidence suggesting that kava consumption may impair neurological functioning. Research carried out by Cairney and colleagues 22 utilized multiple brain functioning tests to investigate the acute effects of kava on neurological functioning. Participants involved in the study included intoxicated kava users as well as individuals who use kava but had not done so in the week prior to testing. The results showed kava intoxication was associated with neurobehavioural changes, specifically motor incoordination and impaired visual attention. Worth noting was the lack of interference kava intoxication had on other cognitive functions, such as thought processes. These findings suggest that while kava intoxication disrupts neurological functioning, it is limited to motor coordination and visual attention.
The availability of evidence showing an association between kava intoxication and neurological impairment warrants the question of the long-term impact of kava consumption on neurological functioning. A study conducted by Cairney and others 23 sought to investigate this issue by administering a series of brain functioning tests on current kava users, past kava users, and non-kava users. In comparing the participants’ performances on the tests, no differences were found between the three participant groups. These findings indicate that heavy, long term kava use does not adversely affect neurological functioning.
Further research into the neurological effects of kava has revealed a possible correlation between kava use and seizures. Clough and colleagues 24 used a hospital database to identify 21 kava users who had documented episodes of seizures. In interviewing health workers and analyzing the patient records, it was found that a significant proportion of these patients experienced impaired consciousness during the seizure with some also displaying abnormal movements. In approximately one-half of the reported seizures, kava use or kava misuse was recorded as the cause of the seizure. It is important to note, however, that the incidence of seizures in the kava-using population is relatively low and the findings from this study must be interpreted with great caution as variables such as a family history of epilepsy, a predisposition to seizures, and the influence of licit and illicit drug use were not considered.
Kava uses
Important Information
- Kava is considered unsafe due to many reports of fatal effects on the liver, including hepatitis, cirrhosis, and liver failure.
- You should not use kava if you have liver disease.
Kava is considered unsafe due to many reports of fatal effects on the liver, including hepatitis, cirrhosis, and liver failure. Even short-term use (1 to 3 months) may increase your risk of liver damage.
You should not use kava if you have liver disease.
Ask a doctor, pharmacist, or other healthcare provider if it is safe for you to use this product if you have:
- depression (especially if you take an antidepressant).
You should not take kava if you are pregnant. Kava may cause weaken muscle tone in the uterus.
Kava can pass into breast milk and may harm a nursing baby. You should not breast-feed while using kava.
Do not give any herbal/health supplement to a child without medical advice.
Avoid using kava together with other herbal/health supplements that can also harm the liver. This includes androstenedione, chaparral, comfrey, DHEA, germander, niacin (vitamin B3), pennyroyal oil, red yeast, and others.
Avoid drinking alcohol while taking kava. Alcohol may increase your risk of liver damage.
Avoid using kava with other herbal/health supplements that can also cause drowsiness. This includes 5-HTP (5-hydroxytryptophan), calamus, California poppy, catnip, gotu kola, Jamaican dogwood, melatonin, St. John’s wort, skullcap (or scullcap), valerian, yerba mansa, and others.
The recommended dosage of kava is dependent upon the concentrations of the kavalactones, the active constituents of kava.
The Australian Therapeutic Goods Administration (similar to the FDA) limitation on kava supplements 25: There is a limit on the maximum amount of Piper methysticum permitted per dosage form – for a tablet or a capsule, there is a limit of 125mg of kavalactones (a group of consistuents found in Piper methysticum); and for a tea bag, there is a limit of 3g of dried rhizome (of Piper methysticum). In addition, all products containing Piper methysticum (any dosage form) must comply with a maximum daily dose of not more than 250mg of kavalactones.
Kava (Piper methysticum) in preparations for human use except when included on the Australian Register of Therapeutic Goods in preparations:
- for oral use when present in tablet, capsule, powder, liquid or teabag form that is labelled with a recommended maximum daily dose of 250 mg or less of kavalactones and:
- the tablet or capsule form contains 125 mg or less of kavalactones per tablet or capsule; or
- the amount of dried whole or peeled rhizome in the teabag does not exceed 3 g; and, where containing more than 25 mg of kavalactones per dose, compliant with the requirements of the Required Advisory Statements for Medicine Labels; or
- the amount of dried whole or peeled rhizome in the unit dose of powder does not exceed 3 g; and
- where containing more than 25 mg of kavalactones per dose, compliant with the requirements of the Medicines Advisory Statements Specification 2014;
- and is packaged with a dose controlled measuring device (Scoop);
- and is limited to a maximum quantity of 200 g of powder per package; or
- the liquid form contains 125 mg or less of kavalactones per unit dose of liquid;
- and, where containing more than 25 mg of kavalactones per dose, compliant with the Medicines Advisory Statements Specification 2014;
- and is packaged in a single serve packaging.
- in topical preparations for use on the rectum, vagina or throat containing dried whole or peeled rhizome or containing aqueous dispersions or aqueous extracts of whole or peeled rhizome; or
- in dermal preparations.
It is also proposed that there is the addition of the mandatory warning statement “Do not exceed recommended daily dose” to be added to all kava packaging as follows:
Medicines Advisory Statements Specification – New warning statement
WARNING: Do not exceed recommended daily dose.
CNS effects
Chewing kava causes numbness in the mouth because of the local anesthetic action of the kavalactones, which is similar to that produced by cocaine, and lasts longer than benzocaine 26. In addition, it produces a mild euphoria characterized by feelings of contentment and fluent and lively speech. Sight, smell, and sound are also heightened 27. Higher doses may lead to muscle weakness, especially in the legs, although some observers relate this to sitting for long periods during the “kava ceremony” rather than to kava itself. Very high doses may induce a deep sleep. CNS effects appear to be mediated by the blockage of voltage-gated sodium and calcium channels ultimately suppressing glutamate release. The kavalactones desmethoxyyangonin and methysticin are believed to block the metabolism of monoamine oxidase-B, producing psychotropic effects 28. Sedative and antianxiety properties may result from kava’s effects on facilitating gamma-aminobutyric acid (GABA)ergic transmission 29.
The molecular mechanism of action of kavalactones and kava is not entirely clear.
Concerns about impaired performance under the influence of kava have motivated several studies in humans. One small study found insignificant decreases in cognitive function when using kava, with only the extent of body sway showing an increase. Subjects’ rating of intoxication under kava was low to moderate, while respiration, heart rate, and blood pressure were unaffected. Kava lowered arousal rating without affecting stress rating, although the decrease was not statistically significant 30. Another small study of 12 patients compared the effects of kava and oxazepam on behavior and event-related potentials in a word recognition task. While oxazepam produced pronounced negative effects on performance, no effects were seen with kava 31. A study of reaction time by the same authors concluded that kava may increase attention slightly, in contrast to oxazepam, which impaired attention 32. Kawain in EEG studies showed mild sedation at high doses (600 mg) but not at lower doses (200 mg) 33. Kava had no effect on alertness and long-term memory in a subsequent trial 34. Minor changes in vision and balance were detected with kava in one subject 35.
Anxiety
Clinical studies of kava have produced evidence of substantial efficacy in mild to moderate anxiety.
In Germany, several investigations have reviewed kava in comparison with other CNS-active herbal products 36. Kawain was compared with oxazepam in a double-blind study of 58 patients and was equally effective and safe 37. Over 4 weeks, kava extract progressively reduced anxiety compared with placebo in 60 patients with no reported adverse reactions 38. A longer 25-week, double-blind, placebo-controlled study of 101 patients with anxiety disorders found that Hamilton Anxiety Scale (HAMA) scores decreased faster with kava than with placebo 39. A similar 4-week study found kava extract effective using both HAMA and Clinical Global Impression Scale scores 40.
The first US study of kava in anxiety was reported at a conference but has not been published. The study found similar therapeutic effects of kava extract under double-blind, placebo-controlled conditions 41. A combination of kava and hormone replacement therapy for menopause symptoms was undertaken in Italy over a period of 6 months. Kava with hormone therapy accelerated the improvement in anxiety scores over single treatments alone 42.
Positive results in a sleep study involving 12 patients were found with kava extract WS 1490, as measured by EEG, electromyography, and subjective measures. No adverse effects on rapid eye movement sleep were found 43. A clinical study of kava’s ability to moderate cardiac symptoms in generalized anxiety disorder found that it improved baroreflex control (BRC) of heart rate, but not respiratory sinus arrhythmia, and improvement in BRC was associated with overall clinical improvement in kava-treated patients 44.
The effects of kava extract WS 1490 were assessed on sleep disturbances associated with anxiety disorders. After 4 weeks of double-blind treatment, the assessment of quality of sleep and recuperative effect after sleep were statistically significant in comparison with placebo. Thus, a potential role for kava in improving sleep in patients with anxiety was suggested 45.
The transition from benzodiazepines to kava extract WS 1490 in treatment of anxiety was monitored in a 5-week study involving 40 patients. While symptoms of benzodiazepine withdrawal were not controlled by kava, anxiety was reduced and symptoms decreased after kava treatment compared with during benzodiazepine therapy 46. A meta-analysis of clinical trials of kava extracts in anxiety has been conducted. Seven trials met the acceptance criteria for inclusion and found kava superior to placebo in the treatment of anxiety as noted by a reduction in the total score of the HAMA 47.
A randomized, double-blind, placebo-controlled study was conducted to assess the effects of kava (total kavalactones 100 mg 3 times daily for 4 weeks) on anxiety. When compared with placebo, there were no statistically significant differences in reductions of anxiety as measured by the State subtest of the State-Trait Anxiety Inventory. Kava also does not appear to improve measures of insomnia 48.
Additionally, data from 3 randomized, double-blind, placebo-controlled trials assessing the efficacy of kava for the treatment of generalized anxiety disorder were analyzed. From these studies, it did not appear that kava was efficacious for the treatment of generalized anxiety disorder 49.
Menopausal symptoms
Kavalactones are purportedly used to relieve anxiolytic effects associated with menopause through modulation of GABA-A receptors in nerve endings 50.
Menopause-related anxiety was successfully treated with kava extract in an 8-week study of 40 women, with rapid onset of efficacy 51. A 12-week study also found improvement in menopausal symptoms; however, poor compliance in the placebo group confounded interpretation 52. In a randomized, prospective study, 68 perimenopausal women requiring therapy for climacteric symptoms were randomized to receive 3 months of calcium 1 g/day plus either kava 100 mg/day (kavapyrones 55 mg), 200 mg/day (kavapyrones 110 mg), or no other therapies. Perimenopause was defined as amenorrhea for 6 to 24 months in women between 47 and 53 years of age with hot flushes occurring at least 3 times daily for at least 1 week and a follicle-stimulating hormone level of greater than 30 units/L. In the control group, there were no differences with regard to anxiety, depression, or climacteric symptoms after 1 and 3 months. Patients treated with kava 100 mg/day had a significant decline in anxiety after 1 and 3 months of therapy. A similar effect was noted in patients treated with kava 200 mg/day for anxiety at 1 and 3 months. Patients treated with both doses of kava experienced improvements in depression after 1 and 3 months of treatment as compared with baseline. Climacteric symptoms were also reduced in both kava treatment groups after 1 and 3 months. The authors concluded that kava may be an effective short-term alternative for improving mood disturbances and climacteric symptoms in women with perimenopausal symptoms 53.
In another study, the effects of hormone replacement therapy with and without kava were assessed for a total of 6 months in 40 women with menopausal anxiety. Subjects with physiological menopause were randomized to receive 50 mcg/day of estrogen with progestin plus either kava extract 100 mg/day or placebo. Subjects with surgically induced menopause were randomly assigned to receive estrogen 50 mcg/day plus either kava 100 mg/day or placebo. A reduction in anxiety scores as measured by the HAMA was noted after 3 and 6 months of treatment for all 4 treatment groups. However, the groups receiving kava extract had a larger reduction in anxiety scores compared with those who did not. Specifically, after 6 months of therapy, HAMA scores were reduced 55% compared with baseline for the patients with physiologically induced menopause receiving kava and hormone placement therapy and reduced 23% for those receiving only hormone replacement therapy. In the surgically induced menopause group, HAMA scores were reduced 53% for those receiving hormone replacement therapy and kava, compared with baseline, and reduced 26% for those receiving only hormone replacement therapy 42.
Kava side effects
Manufactured products such as herbal remedies that contain kava extract have been linked to irreversible liver damage. In the past few years, about 35 cases of severe liver toxicity associated with kava intake have been reported in Europe and the US. However, a direct causal relationship with kava use has been difficult to establish in the majority of the cases, and there is insufficient evidence to implicate kava as the responsible agent. Nevertheless, until further research clarifies any causality, kava should be used with caution.
In December 2000, a previously healthy girl aged 14 years reported the onset of nausea, vomiting, decreased appetite, weight loss, and fatigue 11. One week later, the patient had scleral icterus and was hospitalized with acute hepatitis. During late August to mid-December 2000, the patient reportedly used two kava-containing products. One product was taken intermittently in accordance with package directions (two capsules once daily). The patient estimated that she used the product on approximately 44 days during this period. The patient reported taking the second product in accordance with package directions (two capsules once daily) for 7 consecutive days at the beginning of the 4-month period. Because the product labels were unavailable, other product ingredients were unknown. The patient reported no use of alcohol or medications other than occasional ibuprofen. At the time of hospitalization, the patient’s liver-function tests were markedly abnormal (alanine aminotransferase [ALT]: 4,076 U/L, aspartate aminotransfease [AST]: 3,355 U/L, gamma-glutamyltransferase [GGT]: 148 U/L, total bilirubin: 16.2 mg/dL, ammonia: 17 mg/dL, and prothrombin time: 29.4 seconds). Tests for human immunodeficiency virus (HIV), cytomegalovirus, Epstein-Barr virus, Wilson’s disease, a-antitrypsin deficiency, antinuclear antibodies, and hepatitis A, B, C, and E were negative. Initial liver biopsy revealed active fulminant hepatitis with extensive centrilobular necrosis, approximately 25% hepatocellular viability, and mixed inflammatory infiltrates consisting of lymphocytes, histiocytes, scattered eosinophils, and occasional neutrophils. No viral cytopathic changes were identified, and immunohistochemical stains for hepatitis B surface and core antigens were negative. The patient underwent successful orthotopic liver transplantation. Pathological examination of the native liver revealed active fulminant hepatitis with total hepatocyte necrosis and extensive parenchymal infiltration by lymphocytes, histocytes, and occasional eosinophils. The patient resumed daily activities following recovery from the procedure 11.
In May 2001, a previously healthy woman aged 45 years reported the onset of nausea and weakness approximately 8 weeks after beginning use of a kava-containing dietary supplement that listed on the package label, “Kava kava extract (root), standardized to 30% kavalactones (75 mg), hops (strobiles), German chamomile (flower head), passion flower (flower and fruit), gelatin, and natural vegetable fiber” 11. The patient reported taking one tablet twice daily, which was less than the package label recommendation of one tablet three times daily. The patient reported no concomitant medication or dietary supplement use and rare alcohol ingestion (one to two drinks a year). The patient was initially prescribed rabeprazole for acid reflux symptoms, and this drug was taken for 4 days. In addition, the patient discontinued use of the kava-containing supplement. Several days later, the patient was hospitalized with jaundice and hepatitis. Liver biopsy demonstrated subfulminant hepatic necrosis. Autoimmune and infectious hepatitis tests were negative. Liver transplantation was performed in July 2001, and the patient resumed daily activities following recovery from the procedure 11.
Summary of European Case Reports: Eight liver transplant cases following liver failure associated with the use of kava-containing products have been reported in Europe (six in Germany and two in Switzerland) 11. Two male patients aged 32 and 50 years and six females aged 22–61 years required liver transplants after using kava-containing products. The duration of kava use ranged from 8 weeks to 12 months. The products were used at doses ranging from 60 mg to 240 mg per day 11. Seven patients used kava prepared either by ethanol or acetone extraction methods; one patient used an unspecified type of kava-containing product. The patients had varying symptoms, including influenza-like symptoms and jaundice. Each patient’s condition worsened and progressed to fulminant hepatic failure. Four of these cases have been reported in medical literature 12, 13, 14, 15. Additional information about these cases is available from the German regulatory authority, the Federal Institute for Drugs and Medical Devices, Bonn, Germany, at https://www.bfarm.de/EN/Home/home_node.html. A ninth European transplant case was reported directly to FDA’s MedWatch System by a U.S. pharmaceutical manufacturer (https://www.fda.gov/Safety/MedWatch/default.htm).
By January 2003 kava extracts had been banned in the entire European Union and Canada, and were subject to cautions and advisories by the US FDA as a result of 11 cases of hepatic failure leading to liver transplants, including four deaths 54. A total of 78 cases of hepatotoxicity reputedly linked to kava ingestion are available for review from various databases. Of these adverse events, four probably are linked to kavalactones taken alone and another 23 are potentially linked to kava intake, but also involve the concomitant ingestion of other compounds with potential hepatotoxicity.
Kava affects everyone differently, based on:
- Size, weight and health
- Whether the person is used to taking it
- Whether other drugs are taken around the same time
- The amount taken
- The strength of the drug
If a large amount of kava is taken the following effects may also be experienced 55:
- Drowsiness
- Nausea
- Loss of muscle control
- Mild fever
- Pupil dilation and red eyes
Kava abuse by Australian Aborigines suggest links to hematuria (blood in your urine), infectious diseases, neurological abnormalities, pulmonary hypotension, nephrosis, visual disturbances, ischemic heart disease, thrombosis, and sudden heart attacks 56.
At levels 100 times the therapeutic dose (roughly 13 liters kava beverage a day or 300-400 mg rhizome per week) caused anorexia, ataxia, dyspnea, hair loss, red eyes, skin rash, visual problems, and yellow skin 56.
Stop using kava and call your healthcare provider at once if you have:
liver problems–nausea, upper stomach pain, itching, tired feeling, loss of appetite, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes).
Long-term use of kava may cause serious health problems, including:
- dry, scaly, flaky skin;
- yellowed skin, hair, fingernails, or toenails;
- red eyes, puffy face;
- decreased ability to absorb protein;
- weight loss;
- lung problems;
- blood in your urine; or
- blood cell disorders that can make it easier for you to bleed or get sick.
This is not a complete list of side effects and others may occur.
Long-term effects
Regular use of large amounts of kava may eventually cause 55:
- Mood swings
- Apathy
- Dry, scaly skin. This disorder, called kava dermopathy, occurs only with prolonged use of large amounts of kava and is reversible on reduced intake or cessation 57.
- Malnutrition and severe weight loss
- Getting infections more easily
- Shortness of breath
- Chest pains
- Needing to use more to get the same effect
- Financial, work and social problems
People with a family history of mental illness or who are experiencing mental health problems such as depression and schizophrenia, may find excessive use of kava makes the symptoms of these conditions more severe 55.
Withdrawal
There is no evidence that people who regularly use kava become dependent on the drug, so if you stop taking it, you are unlikely to experience withdrawal symptoms. However, if you have health problems seek medical advice 58.
Kava Overdoese
In a case report of a kava overdose, a 37-year-old man presented to the emergency department with leg weakness, severe vertigo, slurred speech, and the inability to stand on multiple attempts. After 4 hours, his ataxia resolved and his mental status and slurring of speech improved. Thus, overdosage of kava may acutely cause mental status changes and vertigo 59.
References- National Centre for Complementary and Integrative Health. (2016). Kava. https://nccih.nih.gov/health/kava
- Kelly AB (2006) Alcohol problems and psychological health in a remote Indigenous Australian community: a preliminary quantitative study Australian Journal of Rural Health; 14(2): 86-87
- Gounder R; Pac Health Dialog 13 (2): 131-5, 2006 https://www.ncbi.nlm.nih.gov/pubmed/18181402
- Strahl S, Ehret V, Dahm HH, Maier KP. Necrotizing hepatitis after taking herbal remedies. Dtsch Med Wochenschr 1998;123:1410–4.
- Russmann S, Lauterburg BH, Helbling A. Kava hepatotoxicity. Ann Intern Med 2001;135:68–9.
- Clough AR, Currie BJ, Yunupingu MW, Conigrave KM (2006) Action is required to reduce kava supply in Arnhem Land…again! [letter] Medical Journal of Australia; 184(2):91-92
- Urquhart, B., & Thomson, N. (2009). Review of the misuse of kava among Indigenous Australians. Australian Indigenous Health Bulletin, 9(3), 1-14. http://healthbulletin.org.au/articles/review-of-the-misuse-of-kava-among-indigenous-people/
- Lee, K., Freeburn, B., Ella, S., Miller, W., Perry, J., & Conigrave, K. (2012). Handbook for Aboriginal Alcohol and Drug Work.
- Territory Health Services (2002) The public health bush book 2nd ed. [Darwin]: Territory Health Services
- Cairney S, Clough AR, Maruff P, Collie A, Currie BJ, Currie J (2003) Saccade and cognitive function in chronic kava users Neuropsychopharmacology; 28: 389-396
- Hepatic Toxicity Possibly Associated with Kava-Containing Products — United States, Germany, and Switzerland, 1999–2002. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5147a1.htm
- Brauer RB, Pfab R, Becker K, Berger H, Stangl M. Fulminantes leberversagen nach einnahme des pflazlichen heilmittels kava-kava. Z Gastroenterol 2001;39:491.
- Escher M, Desmeules J, Giostra E, et al. Hepatitis associated with kava, a herbal remedy for anxiety. BMJ 2001;322:139.
- Kraft M, Spahn TW, Menzel J, et al. Fulminant liver failure after administration of the herbal antidepressant kava-kava. Dtsch Med Wochenschr 2001;126:970–2.
- Saß M, Schnabel S, Kröger J, Liebe S, Schareck WD. Acute liver failure from kava-kava—a rare indication for liver transplantation. Z Gastroenterol 2001;39:491.
- Clough AR, Bailie R, Burns CB, Guyula T, Wunungmurra R, Wanybarrnga SR (2002) Validity and utility of community health workers’ estimation of kava use Australian and New Zealand Journal of Public Health; 26: 52-57
- Cairney SJ, Maruff P, Clough AR (2002) The neurobehavioural effects of kava Australian and New Zealand Journal of Psychiatry; 36: 657-662
- Lye G (2001) Information about the National Code of Kava management [fact sheet]Darwin: Northern Territory Government
- Clough A, Cairney S, Maruff P, Burns C, Currie B (2001) Possible toxicity and withdrawal seizures in Aboriginal kava drinkers in Arnhem Land (Australia) South Pacific Journal of Psychology; 13(1): 27-34
- Kava hepatotoxicity: comparison of aqueous, ethanolic, acetonic kava extracts and kava-herbs mixtures. J Ethnopharmacol. 2009 Jun 25;123(3):378-84. doi: 10.1016/j.jep.2009.03.038. Epub 2009 Apr 5. https://www.sciencedirect.com/science/article/pii/S0378874109001949
- Xia Q, Chiang H-M, Zhou Y-T, et al. Phototoxicity of Kava — Formation of Reactive Oxygen Species Leading to Lipid Peroxidation and DNA Damage. The American journal of Chinese medicine. 2012;40(6):1271-1288. doi:10.1142/S0192415X12500942. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5743056
- Clough AR, Burns CB, Mununggurr N (2000) Kava in Arnhem Land: a review of consumption and its social correlates Drug and Alcohol Review; 19(3): 319-328
- Unwin E, Thomson N, Gracey M (1994) The impact of tobacco smoking and alcohol consumption on Aboriginal mortality and hospitalisation in Western Australia: 1983-1991 Perth: Health Department of Western Australia
- Kava Code of Management Advisory Group (2003) National Code of Kava ManagementDarwin: Northern Territory Government
- Kava fact sheet. https://www.tga.gov.au/community-qa/kava-fact-sheet
- Fetrow CW, Avila JR. Professional’s Handbook of Complementary & Alternative Medicines . 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004:472-477.
- Freeman LW. Mosby’s Complementary & Alternative Medicine: A Research-Based Approach. 3rd ed. St. Louis, MO: Mosby Elsevier; 2009:431-434.
- Geier FP, Konstantinowicz T. Kava treatment in patients with anxiety. Phytother Res . 2004;18(4):297-300.
- Singh YN, Singh NN. Therapeutic potential of kava in the treatment of anxiety disorders. CNS Drugs . 2002;16(11):731-743.
- Prescott J, Jamieson D, Emdur N, Duffield P. Acute effects of kava on measures of cognitive performance, physiological function and mood. Drug Alcohol Rev . 1993;12(1):49-57.
- Münte TF, Heinze HJ, Matzke M, Steitz J. Effects of oxazepam and an extract of kava roots ( Piper methysticum ) on event-related potentials in a word recognition task. Neuropsychobiology . 1993;27(1):46-53.
- Heinze HJ, Munthe TF, Steitz J, Matzke M. Pharmacopsychological effects of oxazepam and kava extract in a visual search paradigm assessed with event-related potentials. Pharmacopsychiatry . 1994;27(6):224-230.
- Saletu B, Grünberger J, Linzmayer L, Anderer P. EEG-brain mapping, psychometric and psychophysiological studies on central effects of kavain—a kava plant derivative. Human Psychopharmacol . 1989;4(3):169-190.
- Russell PN, Bakker D, Singh NN. The effects of kava on alerting and speed of access of information from long-term memory. Bull Psychon Soc . 1987;25(4):236-237.
- Garner LF, Klinger JD. Some visual effects caused by the beverage kava. J Ethnopharmacol . 1985;13(3):307-311.
- Schulz V, Hübner WD, Ploch M. Clinical trials with phyto-psychopharmacological agents. Phytomedicine . 1997;4(4):379-387.
- Lindenberg D, Pitule-Schödel H. D,L-kavain in comparison with oxazepam in anxiety disorders, a double-blind study of clinical effectiveness [in German]. Fortschr Med . 1990;108(2):49-50, 53-54.
- Kinzler E, Krömer J, Lehmann E. Effect of a special kava extract in patients with anxiety-, tension-, and excitation states of non-psychotic genesis. Double blind study with placebos over 4 weeks [in German]. Arzneimittelforschung . 1991;41(6):584-588.
- Volz HP, Kieser M. Kava-kava extract WS 1490 versus placebo in anxiety disorders—a randomized placebo-controlled 25-week outpatient trial. Pharmacopsychiatry . 1997;30(1):1-5.
- Lehmann E, Kinzler E, Friedmann J. Efficacy of a special kava extract ( Piper methysticum ) in patients with states of anxiety, tension and excitedness of non-mental origin—a double-blind placebo controlled study of four weeks treatment. Phytomedicine . 1996;3(2):113-119.
- Singh NN, Ellis CR, Singh YN. A double-blind, placebo controlled study of the effects of kava ( Kavatrol ) on daily stress and anxiety in adults. Altern Ther . 1998;4:97.
- De Leo V, la Marca A, Morgante G, Lanzetta D, Florio P, Petraglia F. Evaluation of combining kava extract with hormone replacement therapy in the treatment of postmenopausal anxiety. Maturitas . 2001;39(2):185-188.
- Emser W, Bartylla K. Improvement in quality of sleep: effect of kava extract WS 1490 on the sleep patterns in healthy people. TW Neurol Psychiatr . 1991;5:636-642.
- Watkins LL, Connor KM, Davidson JR. Effect of kava extract on vagal cardiac control in generalized anxiety disorder: preliminary findings. J Psychopharmacol . 2001;15(4):283-286.
- Lehrl S. Clinical efficacy of kava extract WS 1490 in sleep disturbances associated with anxiety disorders. Results of a multicenter, randomized, placebo-controlled, double-blind clinical trial [published correction appears in J Affect Disord . 2004;83(2-3):287]. J Affect Disorders . 2004;78(2):101-110.
- Malsch U, Kieser M. Efficacy of kava-kava in the treatment of non-psychotic anxiety, following pretreatment with benzodiazepines. Psychopharmacology (Berl) . 2001;157(3):277-283.
- Pittler MH, Ernst E. Kava extract for treating anxiety. Cochrane Database Syst Rev . 2003;(1):CD003383.
- Jacobs BP, Bent S, Tice JA, Blackwell T, Cummings SR. An internet-based randomized, placebo-controlled trial of kava and valerian for anxiety and insomnia. Medicine (Baltimore) . 2005;84(4):197-207.
- Connor KM, Payne V, Davidson JR. Kava in generalized anxiety disorder: three placebo-controlled trials. Int Clin Psychopharmacol . 2006;21(5):249-253.
- Huntley AL, Ernst E. A systematic review of herbal medicinal products for the treatment of menopausal symptoms. Menopause . 2003;10(5):465-476.
- Warnecke G. Psychosomatic dysfunctions in the female climacteric. Clinical effectiveness and tolerance of kava extract WS 1490 [in German]. Fortschr Med . 1991;109(4):119-122.
- Warnecke G, Pfaender H, Gerster G, Gracza E. Wirksamheit von kawa-kawa-extrakt beim klimakterischen syndrom. Z Phytother . 1990;11:81-86.
- Cagnacci A, Arangion S, Renzi A, Zanni AL, Malmusi S, Volpe A. Kava-kava administration reduces anxiety in perimenopausal women. Maturitas . 2003;44(2):103-109.
- Kava kava: examining new reports of toxicity. Toxicology Letters Volume 150, Issue 1, 15 April 2004, Pages 85-96. https://www.sciencedirect.com/science/article/pii/S0378427404000402
- Lee, K., Freeburn, B., Ella, S., Miller, W., Perry, J., & Conigrave, K. (2012). Handbook for Aboriginal Alcohol and Drug Work
- Duke JA et al; Handbook of Medicinal Hebs 2 nd ed, p. 438, 2002
- Therapeutic potential of kava in the treatment of anxiety disorders. CNS Drugs. 2002;16(11):731-43. https://www.ncbi.nlm.nih.gov/pubmed/12383029
- Territory Health Services, Public Health Strategy Unit. (2005). The Public Health Bush Book (3rd ed.). Darwin: Territory Health Services.
- Perez J, Holmes JF. Altered mental status and ataxia secondary to acute kava ingestion. J Emerg Med . 2005;28(1):49-51.