What foods are good for underactive thyroid?
Hypothyroidism also called underactive thyroid, is when your thyroid gland doesn’t make enough thyroid hormones to meet your body’s needs. Your thyroid is a small, butterfly-shaped gland in the front of your neck. Your thyroid makes thyroid hormones that control the way your body uses energy. Thyroid hormones affect nearly every organ in your body and control many of your body’s most important functions. For example, they affect your breathing, heart rate, body weight, digestion, and moods. Without enough thyroid hormones, many of your body’s functions slow down. Hypothyroidism can contribute to high cholesterol. In rare cases, untreated underactive thyroid can cause myxedema coma. This is a condition in which your body’s functions slow down to the point that it becomes life-threatening.
During pregnancy, hypothyroidism can cause complications, such as premature birth, high blood pressure in pregnancy, and miscarriage. It can also slow the baby’s growth and development. However, thyroid hormone replacement medicines (levothyroxine) can help prevent problems and are safe to take during pregnancy. Many women taking thyroid hormone medicine (levothyroxine) need a higher dose during pregnancy, so contact your doctor right away if you find out you’re pregnant.
Hypothyroidism has several causes. They include:
- Hashimoto’s disease is also known as Hashimoto’s thyroiditis, chronic lymphocytic thyroiditis or autoimmune thyroiditis, an autoimmune disorder where your immune system attacks your thyroid. This is the most common cause of hypothyroidism in the United States, which affects about 5 in 100 Americans 1. After age six, Hashimoto’s thyroiditis is the most common cause of hypothyroidism in the United States and in those areas of the world where iodine intake is adequate 2. The incidence is estimated to be 0.8 per 1000 per year in men and 3.5 per 1000 per year in women. Twin studies have shown an increased concordance of autoimmune thyroiditis in monozygotic twins as compared with dizygotic twins. Danish studies have demonstrated concordance rates of 55% in monozygotic twins, compared with only 3% in dizygotic twins 3. This data suggests that 79% of predisposition is due to genetic factors, allotting 21% for environmental and sex hormone influences.
- Thyroiditis, inflammation of the thyroid. Thyroiditis causes stored thyroid hormone to leak out of your thyroid gland. At first, the leakage increases your blood’s hormone levels, leading to thyrotoxicosis, a condition in which thyroid hormone levels are too high. The thyrotoxicosis may last for many months. After that, your thyroid may become underactive and, over time, the condition may become permanent, requiring thyroid hormone replacement.
- Three types of thyroiditis can cause thyrotoxicosis followed by hypothyroidism 4:
- Subacute thyroiditis involves a painfully inflamed and enlarged thyroid.
- Postpartum thyroiditis develops after a woman gives birth.
- Silent thyroiditis is painless, even though your thyroid may be enlarged. Experts think it is probably an autoimmune condition.
- Three types of thyroiditis can cause thyrotoxicosis followed by hypothyroidism 4:
- Congenital hypothyroidism, is hypothyroidism that is present at birth. Some babies are born with a thyroid that is not fully developed or does not work properly. If untreated, congenital hypothyroidism can lead to intellectual disability and growth failure—when a baby doesn’t grow as expected. Early treatment can prevent these problems. That’s why most newborns in the United States are tested for hypothyroidism.
- Surgical removal of part or all of the thyroid. When surgeons remove part of the thyroid, the remaining part may produce normal amounts of thyroid hormone. But some people who have this surgery may develop hypothyroidism. Removing the entire thyroid always results in hypothyroidism.
- Surgeons may remove part or all of the thyroid as a treatment for:
- hyperthyroidism
- a large goiter
- thyroid nodules, which are noncancerous tumors or lumps in the thyroid that can produce too much thyroid hormone
- small thyroid cancers
- Surgeons may remove part or all of the thyroid as a treatment for:
- Radiation treatment of the thyroid. Radioactive iodine, a common treatment for hyperthyroidism (overactive thyroid), gradually destroys thyroid cells. If you receive radioactive iodine treatment, you probably will eventually develop hypothyroidism. Doctors also treat people who have head or neck cancers with external radiation therapy, which can also damage the thyroid if it is included in the treatment.
- Certain medicines (e.g., lithium, dopamine, glucocorticoids). Several recently developed cancer medicines, in particular, can either affect the thyroid directly or affect it indirectly by damaging the pituitary gland.
- In rare cases, a pituitary disease, pregnancy or too much or too little iodine in your diet
- Pituitary disorder. A relatively rare cause of hypothyroidism is the failure of the pituitary gland to produce enough thyroid-stimulating hormone (TSH) — usually because of a benign tumor of the pituitary gland.
- Iodine deficiency–most common worldwide. If a person’s iodine intake falls below approximately 10–20 micrograms (mcg)/day, hypothyroidism occurs 5. Iodine is a trace mineral found primarily in seafood, seaweed, plants grown in iodine-rich soil and iodized salt. Iodine is essential for the production of thyroid hormones. Too little iodine can lead to hypothyroidism, and too much iodine can worsen hypothyroidism in people who already have the condition. In some parts of the world, iodine deficiency is common, but the addition of iodine to table salt has virtually eliminated this problem in the United States.
- Pregnancy. Some women develop hypothyroidism during or after pregnancy (postpartum hypothyroidism), often because they produce antibodies to their own thyroid gland. Left untreated, hypothyroidism increases the risk of miscarriage, premature delivery and preeclampsia — a condition that causes a significant rise in a woman’s blood pressure during the last three months of pregnancy. It can also seriously affect the developing fetus.
You are at higher risk for hypothyroidism if you:
- Are a woman
- Are older than age 60. The prevalence of thyroid disease, in general, increases with age.
- Have had a thyroid problem before, such as a goiter (enlarged thyroid)
- Have had surgery to correct a thyroid problem
- Have received radiation treatment to the thyroid, neck, or chest
- Have a family history of thyroid disease
- Were pregnant or had a baby in the past 6 months
- Have Turner syndrome, a genetic disorder that affects females
- Have pernicious anemia, in which the body cannot make enough healthy red blood cells because it does not have enough vitamin B12
- Have Sjogren’s syndrome, a disease that causes dry eyes and mouth
- Have Type 1 diabetes
- Have rheumatoid arthritis, an autoimmune disease that affects the joints
- Have lupus, a chronic autoimmune disease
The symptoms of hypothyroidism can vary from person to person and may include:
- Fatigue
- Weight gain
- A puffy face
- Trouble tolerating cold
- Joint and muscle pain
- Constipation
- Dry skin
- Dry, thinning hair
- Decreased sweating
- Heavy or irregular menstrual periods
- Fertility problems in women
- Depression
- Slowed heart rate
- Reduced exercise tolerance
- Increased sensitivity to cold
- Goiter, an enlarged thyroid that may cause your neck to look swollen. Sometimes it can cause trouble with breathing or swallowing.
Because hypothyroidism develops slowly, many people don’t notice symptoms of the disease for months or even years.
Hypothyroidism can contribute to high cholesterol. If you have high cholesterol, you should get tested for hypothyroidism. Rarely, severe untreated hypothyroidism may lead to myxedema coma, an extreme form of hypothyroidism in which the body’s functions slow to a life-threatening point. Myxedema coma requires immediate medical treatment.
The mainstay of treatment for hypothyroidism is thyroid hormone replacement 6. The drug of choice is levothyroxine (LT4), which is identical to the natural thyroid hormone thyroxine (T4) and is administered orally. Levothyroxine was prescribed in pill form for many years, and is now also available as a liquid and in a soft gel capsule 7. These newer formulas may be helpful to people with digestive problems that affect how the thyroid hormone pill is absorbed. Absorption of levothyroxine occurs in the jejunum and ileum 8. An acidic pH in the stomach, as occurs during fasting conditions, appears to be important for subsequent intestinal absorption. The absorption of an orally administered dose of levothyroxine is about 70%–80% under optimum fasting conditions 9.
Levothyroxine has a half-life of 7 days and can be given daily. Some foods and supplements can affect how well your body absorbs levothyroxine. It should not be given with iron or calcium supplements, aluminum hydroxide, and proton pump inhibitors to avoid suboptimal absorption. Examples include grapefruit juice, espresso coffee, soy, and multivitamins that contain iron or calcium 10. Taking the medicine on an empty stomach can prevent this from happening. Levothyroxine is best taken early in the morning on an empty stomach for optimum absorption. Your doctor may ask you to take the levothyroxine in the morning, 30 to 60 minutes before you eat your first meal.
The standard levothyroxine dose is 1.6 – 1.8 microgram (mcg) per kg body weight per day, but it can vary from one patient to another 11. Patients less than 50 years old should be commenced on standard full dose; however, lower doses should be used in patients with cardiovascular diseases and the elderly. In patients older than 50 years, the recommended starting dose is 25 mcg/day with reevaluation in six to eight weeks. In contrast, in pregnancy, the dose of thyroxine needs to be increased by 30%, and in patients with the short-bowel syndrome, increased doses of levothyroxine are needed to maintain a euthyroid (normal) state.
Your doctor will give you a blood test about 6 to 8 weeks after you begin taking levothyroxine and adjust your dose if needed. Each time you change your dose, you’ll have another blood test. Once you’ve reached a dose that’s working for you, your doctor will likely repeat the blood test in 6 months and then once a year.
Never stop taking your medicine or take a higher dose without talking with your doctor first. Taking too much thyroid hormone medicine can cause serious problems, such as atrial fibrillation or osteoporosis 12.
Your hypothyroidism can be well-controlled with thyroid hormone medicine, as long as you take the medicine as instructed by your doctor and have regular follow-up blood tests.
There is less evidence to support an autoimmune or anti-inflammatory diet. The theory behind the inflammation has to do with the leaky gut syndrome, where there is an insult to the gut mucosa, which allows penetrance of proteins that do not typically enter the bloodstream via transporters in the gut mucosa. It is theorized that a response similar to molecular mimicry occurs, and antibodies are produced against the antigens. Unfortunately, the antigen may be very structurally similar to thyroid peroxidase, leading to antibody formation against this enzyme. The concept of an autoimmune diet is based on healing the gut and decreasing the severity of the autoimmune response. More research is required on this topic before it becomes a part of the hypothyroidism treatment guidelines.
The thyroid uses iodine, a mineral in some foods, to make thyroid hormones. However, if you have Hashimoto’s disease or other types of autoimmune thyroid disorders, you may be sensitive to harmful side effects from iodine. Eating foods that have large amounts of iodine—such as kelp, dulse, or other kinds of seaweed, and certain iodine-rich medicines—may cause hypothyroidism or make it worse 13. Taking iodine supplements can have the same effect.
However, if you are pregnant, you need to take enough iodine because the baby gets iodine from your diet. Too much iodine can cause problems as well, such as a goiter in the baby. If you are pregnant, talk with your doctor about how much iodine you need 13.
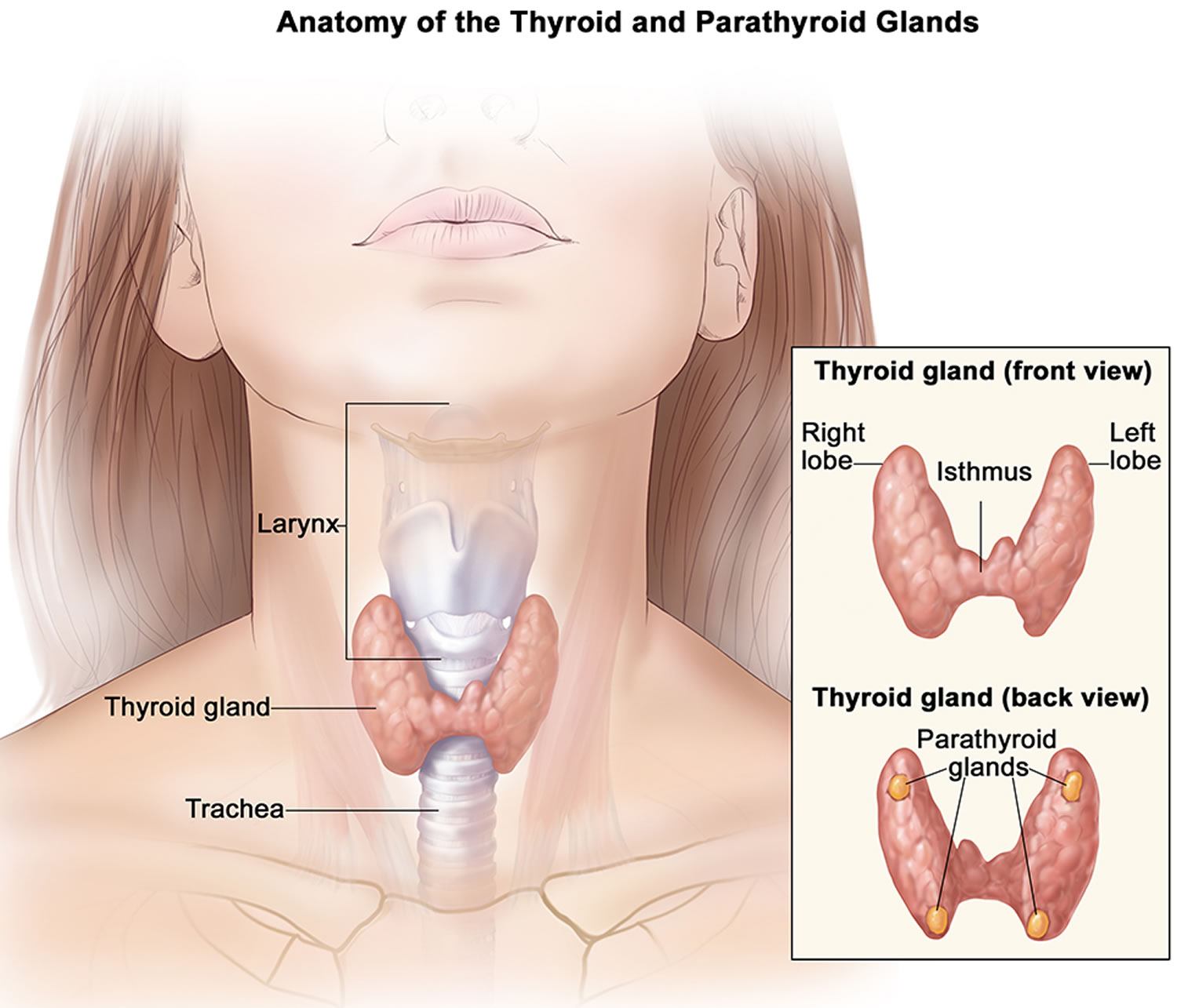
Thyroid gland
The thyroid gland is the largest adult gland to have a purely endocrine function, weighing about 25-30 g. The thyroid gland is a small butterfly shaped gland with 2 lobes, the right lobe and the left lobe joined by a narrow piece of the thyroid gland called the isthmus, that is located in front of your neck near the base of your throat, beneath the larynx (voice box or Adam’s apple). About 50% of thyroid glands have a small third lobe, called the pyramidal lobe. It extends superiorly from the isthmus. The thyroid gland makes and releases hormones. You can’t usually feel a thyroid gland that is normal.
The thyroid gland has 2 main types of cells:
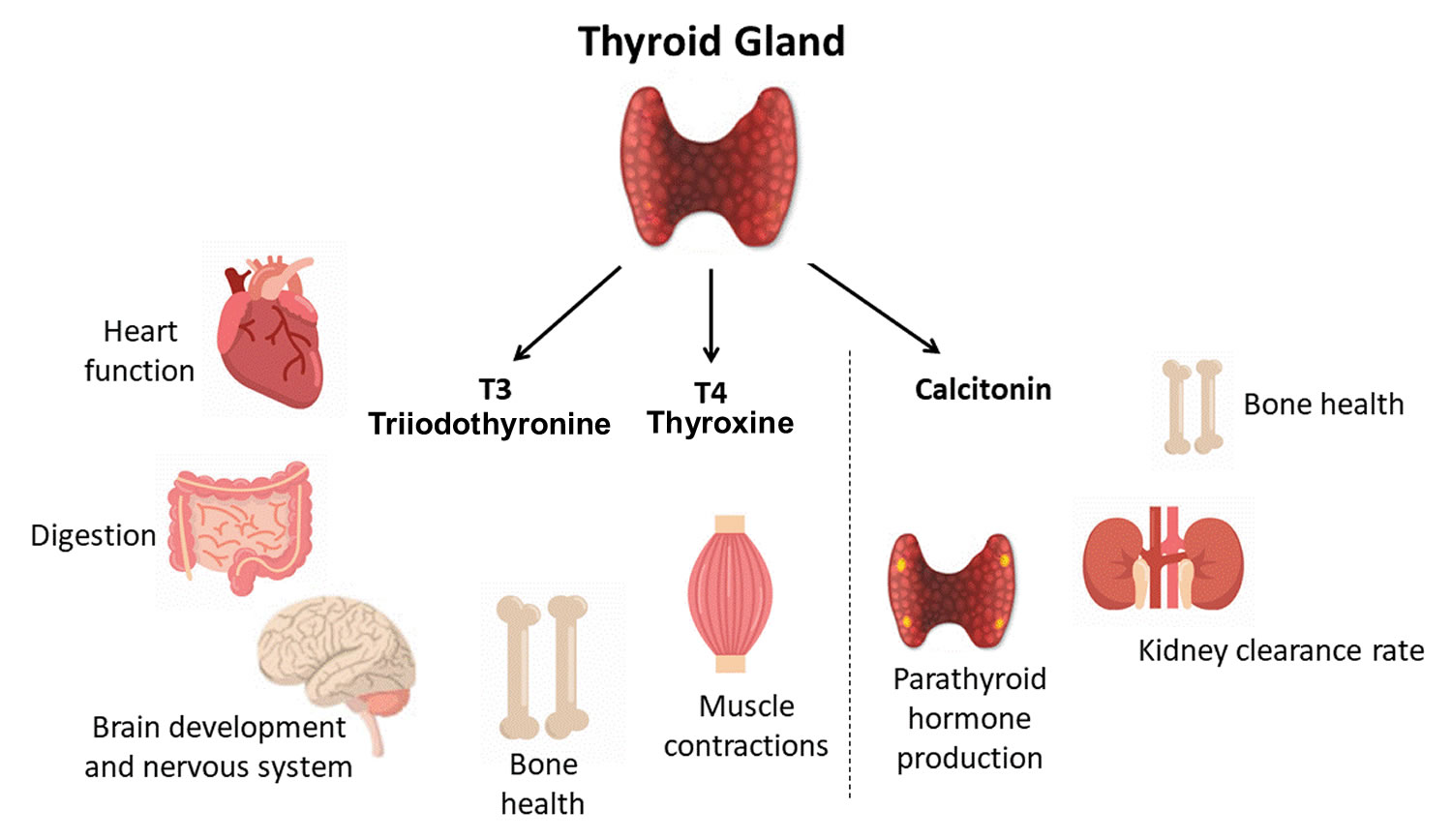
- Follicular cells use iodine from the blood to make thyroid hormones, which help regulate a person’s metabolism. Having too much thyroid hormone (hyperthyroidism) can cause a fast or irregular heartbeat, trouble sleeping, nervousness, hunger, weight loss, and a feeling of being too warm. Having too little thyroid hormone (hypothyroidism) causes a person to slow down, feel tired, and gain weight. The amount of thyroid hormone released by the thyroid gland is regulated by the pituitary gland at the base of the brain, which makes a substance called thyroid-stimulating hormone (TSH) (see Figure 3).
- C cells also called parafollicular cells at the periphery of the follicles that make calcitonin, a hormone that helps control how your body uses calcium. The parafollicular cells (C cells) respond to rising levels of blood calcium by secreting the hormone calcitonin. Calcitonin antagonizes (blocks) parathyroid hormone (PTH) and stimulates osteoblast activity, thus promoting calcium deposition and bone formation. It is important mainly in children, having relatively little effect in adults.
Other, less common cells in the thyroid gland include immune system cells (lymphocytes) and supportive (stromal) cells.
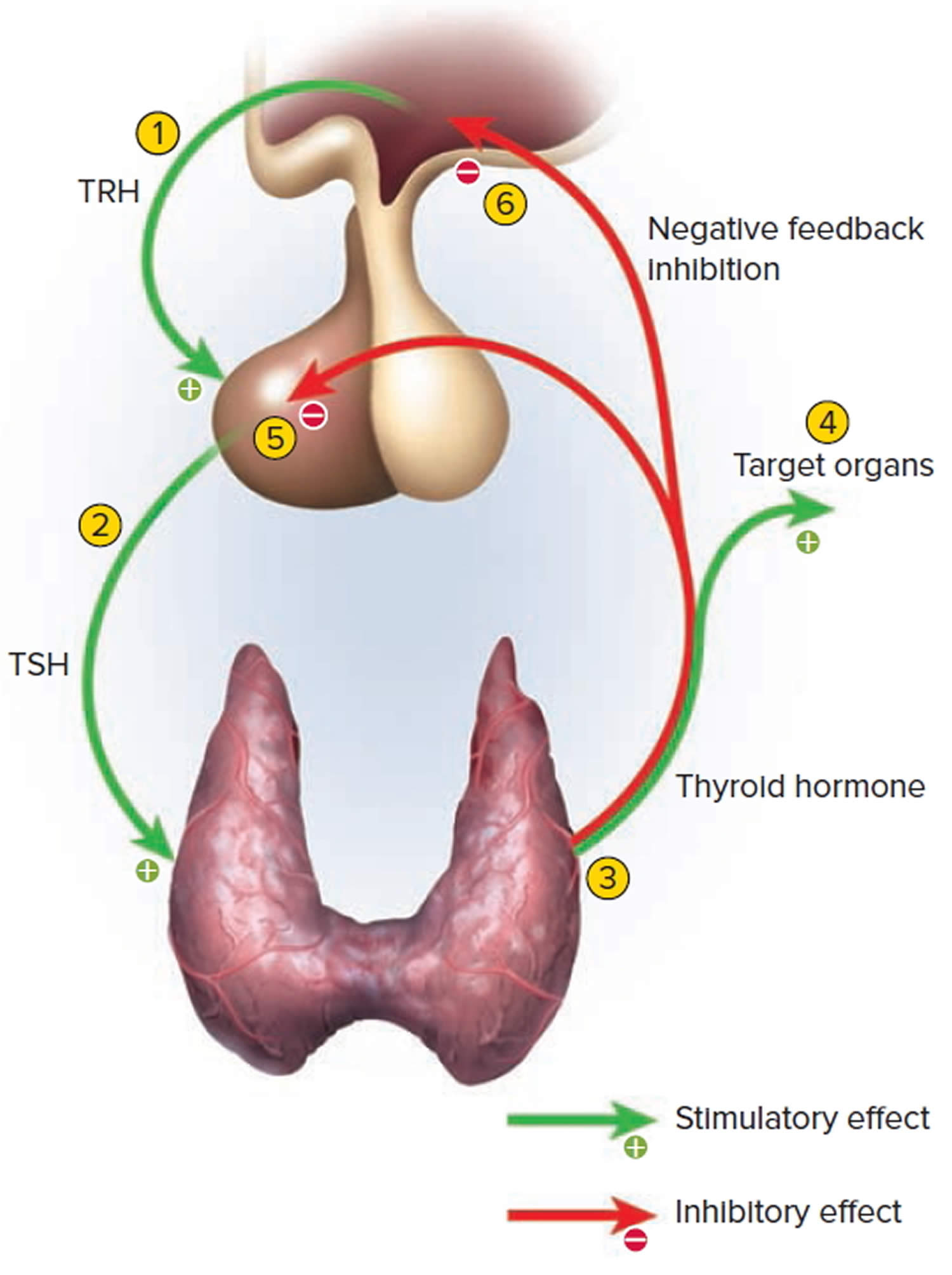
Thyroid hormone is secreted or inhibited in response to fluctuations in metabolic rate. The brain monitors the body’s metabolic rate and stimulates thyroid hormone secretion through the action of thyrotropin-releasing hormone (TRH) and thyroid stimulating hormone (TSH) as depicted in figure 3.
The primary effect of thyroid hormone (TH) is to increase one’s metabolic rate. As a result, it raises oxygen consumption and has a calorigenic effect—it increases heat production. To ensure an adequate blood and oxygen supply to meet this increased metabolic demand, thyroid hormone also raises the breathing (respiratory) rate, heart rate, and strength of the heartbeat. It stimulates the appetite and accelerates the breakdown of carbohydrates, fats, and protein for fuel. Thyroid hormone also promotes alertness and quicker reflexes; growth hormone secretion; growth of the bones, skin, hair, nails, and teeth; and development of the fetal nervous system.
Figure 1. Thyroid gland and parathyroid gland
Footnotes: Anatomy of the thyroid and parathyroid glands. The thyroid gland lies at the base of the throat near the trachea. It is shaped like a butterfly, with the right lobe and left lobe connected by a thin piece of tissue called the isthmus. The parathyroid glands are four pea-sized organs found in the neck near the thyroid. The thyroid and parathyroid glands make hormones.
What does the thyroid gland do?
Formation, storage, and release of thyroid hormones
The thyroid gland is the only endocrine gland that stores its secretory product in large quantities—normally about a 100-day supply. Synthesis and secretion of triiodothyronine (T3) and thyroxine or tetraiodothyronine (T4) occurs as follows:
- Iodide trapping. Thyroid follicular cells trap iodide ions (I −) by actively transporting them from the blood into the cytosol. As a result, the thyroid gland normally contains most of the iodide in the body.
- Synthesis of thyroglobulin. While the follicular cells are trapping I −, they are also synthesizing thyroglobulin (TGB), a large glycoprotein that is produced in the rough endoplasmic reticulum, modified in the Golgi complex, and packaged into secretory vesicles. The vesicles then undergo exocytosis, which releases thyroglobulin into the lumen of the follicle.
- Oxidation of iodide. Some of the amino acids in thyroglobulin are tyrosines that will become iodinated. However, negatively charged iodide (I −) ions cannot bind to tyrosine until they undergo oxidation (removal of electrons) to iodine: I −→ I. As the iodide ions are being oxidized, they pass through the membrane into the lumen of the follicle.
- Iodination of tyrosine. As iodine atoms (I) form, they react with tyrosines that are part of thyroglobulin molecules. Binding of one iodine atom yields monoiodotyrosine (T1), and a second iodination produces diiodotyrosine (T2). The thyroglobulin with attached iodine atoms, a sticky material that accumulates and is stored in the lumen of the thyroid follicle, is termed colloid.
- Coupling of monoiodotyrosine (T1) and diiodotyrosine (T2). During the last step in the synthesis of thyroid hormone, two diiodotyrosine (T2) molecules join to form thyroxine (T4) or one T1 and one T2 join to form triiodothyronine (T3).
- Pinocytosis and digestion of colloid. Droplets of colloid reenter follicular cells by pinocytosis and merge with lysosomes. Digestive enzymes in the lysosomes break down thyroglobulin, cleaving off molecules of triiodothyronine (T3) and thyroxine (T4).
- Secretion of thyroid hormones. Because T3 and T4 are lipid soluble, they diffuse through the plasma membrane into interstitial fluid and then into the blood. T4 normally is secreted in greater quantity than T3, but T3 is several times more potent. Moreover, after T4 enters a body cell, most of it is converted to T3 by removal of one iodine.
- Transport thyroid hormones in the blood. More than 99% of both the T3 and the T4 combine with transport proteins in the blood, mainly thyroxine binding globulin (TBG).
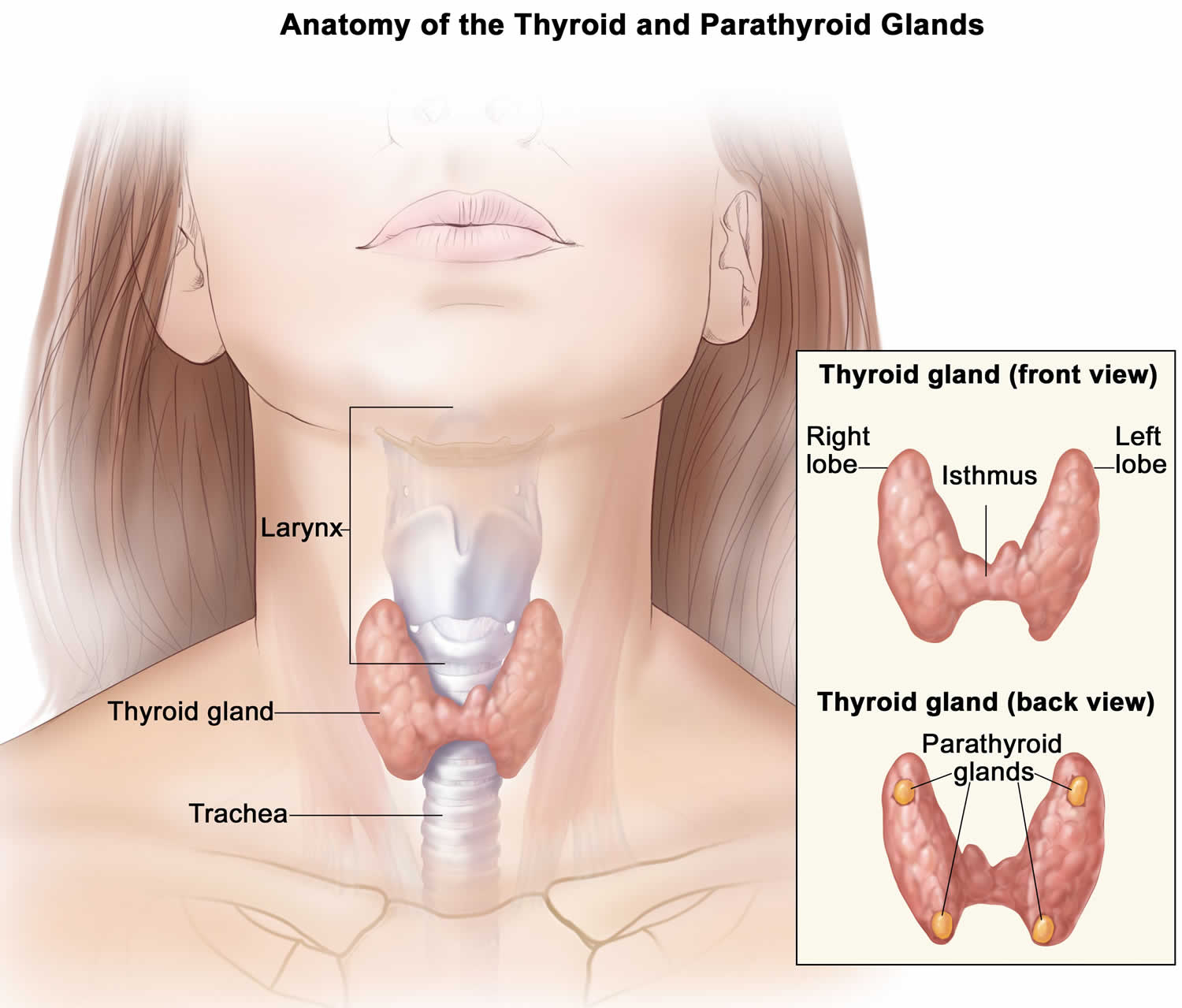
Figure 2. Thyroid hormones
Actions of thyroid hormones
Because most body cells have receptors for thyroid hormones, triiodothyronine (T3) and thyroxine (T4) affect tissues throughout the body. Thyroid hormones act on their target cells mainly by inducing gene transcription and protein synthesis. The newly formed proteins in turn carry out the cellular response.
Functions of thyroid hormones include the following:
- Increase basal metabolic rate. Thyroid hormones raise the basal metabolic rate (BMR), the rate of energy expenditure under standard or basal conditions (awake, at rest, and fasting). When basal metabolic rate increases, cellular metabolism of carbohydrates, lipids, and proteins increases. Thyroid hormones increase BMR in several ways: (1) They stimulate synthesis of additional Na+/K+ ATPases, which use large amounts of ATP to continually eject sodium ions (Na+) from cytosol into extracellular fluid and potassium ions (K+) from extracellular fluid into cytosol; (2) they increase the concentrations of enzymes involved in cellular respiration, which increases the breakdown of organic fuels and ATP production; and (3) they increase the number and activity of mitochondria in cells, which also increases ATP production. As cells produce and use more ATP, basal metabolic rate increases, more heat is given off and body temperature rises, a phenomenon called the calorigenic effect. In this way, thyroid hormones play an important role in the maintenance of normal body temperature. Normal mammals can survive in freezing temperatures, but those whose thyroid glands have been removed cannot.
- Enhance actions of catechlolamines. Thyroid hormones have permissive effects on the catecholamines (epinephrine and norepinephrine) because they up-regulate β-adrenergic receptors. Catecholamines bind to β-adrenergic receptors, promoting sympathetic responses. Therefore, symptoms of excess levels of thyroid hormone include increased heart rate, more forceful heartbeats, and increased blood pressure.
- Regulate development and growth of nervous tissue and bones. Thyroid hormones are necessary for the development of the nervous system: They promote synapse formation, myelin production, and growth of dendrites. Thyroid hormones are also required for growth of the skeletal system: They promote formation of ossification centers in developing bones, synthesis of many bone proteins, and secretion of growth hormone (GH) and insulin-like growth factors (IGFs). Deficiency of thyroid hormones during fetal development, infancy, or childhood causes severe mental retardation and stunted bone growth.
Control of thyroid hormone secretion
Thyrotropin-releasing hormone (TRH) from the hypothalamus and thyroid-stimulating hormone (TSH) from the anterior pituitary stimulate secretion of thyroid hormones, as shown in Figure 5:
- Low blood levels of T3 and T4 or low metabolic rate stimulate the hypothalamus to secrete thyrotropin-releasing hormone (TRH).
- Thyrotropin-releasing hormone (TRH) enters the hypothalamic–hypophyseal portal system and flows to the anterior pituitary, where it stimulates thyrotrophs to secrete thyroid stimulating hormone (TSH).
- Thyroid stimulating hormone (TSH) stimulates virtually all aspects of thyroid follicular cell activity, including iodide trapping, hormone synthesis and secretion, and growth of the follicular cells.
- The thyroid follicular cells release T3 and T4 into the blood until the metabolic rate returns to normal.
- An elevated level of T3 inhibits release of TRH and TSH (negative feedback inhibition).
Conditions that increase ATP demand—a cold environment, hypoglycemia, high altitude, and pregnancy—increase the secretion of the thyroid hormones.
Figure 3. Control of thyroid hormone secretion
Footnote: Negative Feedback Inhibition of the Anterior Pituitary Gland by the Thyroid Gland
How much iodine do I need?
The amount of iodine you need each day depends on your age. Average daily recommended amounts are listed below in micrograms (mcg).
Table 1 lists the current Recommended Dietary Allowances (RDA – the average daily level of intake sufficient to meet the nutrient requirements of nearly all [97%–98%] healthy individuals; often used to plan nutritionally adequate diets for individuals) for iodine 14. For infants from birth to 12 months, the Food and Nutrition Board at the Institute of Medicine of the National Academies established an Adequate Intake (AI) for iodine that is equivalent to the mean intake of iodine in healthy, breastfed infants in the United States.
The World Health Organization (WHO), United Nations Children’s Fund (UNICEF), and the International Council for the Control of Iodine Deficiency Disorders (ICCIDD) recommend a slightly higher iodine intake for pregnant women of 250 mcg per day 15, 16.
Table 1. Recommended Dietary Allowances (RDAs) for Iodine
| Age | Male | Female | Pregnancy | Lactation |
| Birth to 6 months | 110 mcg* | 110 mcg* | ||
| 7–12 months | 130 mcg* | 130 mcg* | ||
| 1–3 years | 90 mcg | 90 mcg | ||
| 4–8 years | 90 mcg | 90 mcg | ||
| 9–13 years | 120 mcg | 120 mcg | ||
| 14–18 years | 150 mcg | 150 mcg | 220 mcg | 290 mcg |
| 19+ years | 150 mcg | 150 mcg | 220 mcg | 290 mcg |
Footnote: * Adequate Intake (AI)
What foods are good source for iodine?
Seaweed (such as kelp, nori, kombu, and wakame) is one of the best food sources of iodine 5. Other good sources include fish and other seafood, as well as eggs (see Table 2). Iodine is also present in human breast milk 14 and infant formulas 17. The U.S. Department of Agriculture (USDA) lists the iodine content of numerous foods and beverages 17.
Dairy products contain iodine. However, the amount of iodine in dairy products varies by whether the cows received iodine feed supplements and whether iodophor sanitizing agents were used to clean the cows and milk-processing equipment 18. For example, an analysis of 44 samples of nonfat milk found a range of 38 to 159 mcg per cup (with an average of 85 mcg/cup used for Table 2) 17. Plant-based beverages used as milk substitutes, such as soy and almond beverages, contain relatively small amounts of iodine.
Most commercially prepared bread contains very little iodine unless the manufacturer has used potassium iodate or calcium iodate as a dough conditioner 19. Manufacturers list dough conditioners as an ingredient on product labels but are not required to include iodine on the Nutrition Facts label 20, even though these conditioners provide a substantial amount of iodine. According to 2019 data from the USDA Branded Food Products Database, approximately 20% of ingredient labels for white bread, whole-wheat bread, hamburger buns, and hot dog buns listed iodate. Pasta is not a source of iodine unless it is prepared in water containing iodized salt because it absorbs some of the iodine 21.
Most fruits and vegetables are poor sources of iodine, and the amounts they contain are affected by the iodine content of the soil, fertilizer use, and irrigation practices 19. This variability affects the iodine content of meat and animal products because of its impact on the iodine content of foods that the animals consume 22. The iodine amounts in different seaweed species also vary greatly. For example, commercially available seaweeds in whole or sheet form have iodine concentrations ranging from 16 mcg/g to 2,984 mcg/g 23. For these reasons, the values for the foods listed in Table 2 are approximate but can be used as a guide for estimating iodine intakes.
Table 2. Iodine Content of Selected Foods
| Food | Micrograms (mcg) per serving | Percent DV* |
| Seaweed, nori, dried, 10 g | 232 | 155 |
| Bread, whole-wheat, made with iodate dough conditioner, 1 slice | 198 | 132 |
| Bread, white, enriched, made with iodate dough conditioner, 1 slice | 185 | 123 |
| Cod, baked, 3 ounces | 158 | 106 |
| Yogurt, Greek, plain, nonfat, 1 cup | 116 | 77 |
| Oysters, cooked, 3 ounces | 93 | 62 |
| Milk, nonfat, 1 cup | 85 | 57 |
| Iodized table salt, 1.5 g (approx. ¼ teaspoon) | 76 | 51 |
| Fish sticks, cooked, 3 ounces | 58 | 39 |
| Pasta, enriched, boiled in water with iodized salt, 1 cup | 36 | 24 |
| Egg, hard boiled, 1 large | 26 | 17 |
| Ice cream, chocolate, ½ cup | 21 | 14 |
| Liver, beef, cooked, 3 ounces | 14 | 9 |
| Cheese, cheddar, 1 ounce | 14 | 9 |
| Shrimp, cooked, 3 ounces | 13 | 9 |
| Tuna, canned in water, drained, 3 ounces | 7 | 5 |
| Soy beverage, 1 cup | 7 | 5 |
| Fruit cocktail in light syrup, canned, ½ cup | 6 | 4 |
| Beef, chuck, roasted, 3 ounces | 3 | 2 |
| Chicken breast, roasted, 3 ounces | 2 | 1 |
| Almond beverage, 1 cup | 2 | 1 |
| Apple juice, 1 cup | 1 | 1 |
| Bread, whole-wheat, made without iodate dough conditioner, 1 slice | 1 | 1 |
| Bread, white, enriched, made without iodate dough conditioner, 1 slice | 1 | 1 |
| Raisin bran cereal, 1 cup | 1 | 1 |
| Rice, brown, cooked, ½ cup | 1 | 1 |
| Corn, canned, ½ cup | 1 | 1 |
| Sea salt, non-iodized, 1.5 g (approx. ¼ teaspoon) | <1 | <1 |
| Broccoli, boiled, ½ cup | 0 | 0 |
| Banana, 1 medium | 0 | 0 |
| Lima beans, mature, boiled, ½ cup | 0 | 0 |
| Green peas, frozen, boiled, ½ cup | 0 | 0 |
| Pasta, enriched, boiled in water without iodized salt, 1 cup | 0 | 0 |
Footnotes: *DV = Daily Value. The U.S. Food and Drug Administration (FDA) developed DVs to help consumers compare the nutrient contents of foods and dietary supplements within the context of a total diet. The DV for iodine is 150 mcg for adults and children aged 4 years and older [12]. FDA does not require food labels to list iodine content unless iodine has been added to the food. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
[Source 17 ]What are complications of untreated hypothyroidism?
Untreated hypothyroidism can lead to a number of health problems:
- Goiter. Constant stimulation of your thyroid to release more hormones may cause the gland to become larger — a condition known as a goiter. Although generally not uncomfortable, a large goiter can affect your appearance and may interfere with swallowing or breathing.
- Heart problems. Hypothyroidism may also be associated with an increased risk of heart disease and heart failure, primarily because high levels of low-density lipoprotein (LDL) cholesterol — the “bad” cholesterol — can occur in people with an underactive thyroid.
- Mental health issues. Depression may occur early in hypothyroidism and may become more severe over time. Hypothyroidism can also cause slowed mental functioning.
- Peripheral neuropathy. Long-term uncontrolled hypothyroidism can cause damage to your peripheral nerves. These are the nerves that carry information from your brain and spinal cord to the rest of your body — for example, your arms and legs. Peripheral neuropathy may cause pain, numbness and tingling in affected areas.
- Myxedema. This rare, life-threatening condition is the result of long-term, undiagnosed hypothyroidism. Its signs and symptoms include intense cold intolerance and drowsiness followed by profound lethargy and unconsciousness. A myxedema coma may be triggered by sedatives, infection or other stress on your body. If you have signs or symptoms of myxedema, you need immediate emergency medical treatment.
- Infertility. Low levels of thyroid hormone can interfere with ovulation, which impairs fertility. In addition, some of the causes of hypothyroidism — such as autoimmune disorder — can also impair fertility.
- Birth defects. Babies born to women with untreated thyroid disease may have a higher risk of birth defects compared to babies born to healthy mothers. These children are also more prone to serious intellectual and developmental problems. Infants with untreated hypothyroidism present at birth are at risk of serious problems with both physical and mental development. But if this condition is diagnosed within the first few months of life, the chances of normal development are excellent.
How is hypothyroidism diagnosed?
Your doctor will take your medical history and perform a physical exam. A hypothyroidism diagnosis can’t be based on symptoms alone because many of its symptoms are the same as those of other diseases 24. That’s why your doctor may use several thyroid blood tests and imaging tests to confirm the diagnosis and find its cause.
Because hypothyroidism can cause fertility problems, women who have trouble getting pregnant often get tested for thyroid problems.
The correct diagnosis of hypothyroidism depends on the following 25:
- Symptoms. Hypothyroidism doesn’t have any characteristic symptoms. There are no symptoms that people with hypothyroidism always have and many symptoms of hypothyroidism can occur in people with other diseases. One way to help figure out whether your symptoms are due to hypothyroidism is to think about whether you’ve always had the symptom (hypothyroidism is less likely) or whether the symptom is a change from the way you used to feel (hypothyroidism is more likely).
- Medical and family history. You should tell your doctor:
- about changes in your health that suggest that your body is slowing down;
- if you’ve ever had thyroid surgery;
- if you’ve ever had radiation to your neck to treat cancer;
- if you’re taking any of the medicines that can cause hypothyroidism— amiodarone, lithium, interferon alpha, interleukin-2, and maybe thalidomide;
- whether any of your family members have thyroid disease..
- Physical exam. The doctor will check your thyroid gland and look for changes such as dry skin, swelling, slower reflexes, and a slower heart rate.
- Blood tests. There are two blood tests that are used in the diagnosis of hypothyroidism.
- TSH (thyroid-stimulating hormone) test. This is the most important and sensitive test for hypothyroidism. It measures how much of the thyroid hormone thyroxine (T4) the thyroid gland is being asked to make. An abnormally high TSH means hypothyroidism: the thyroid gland is being asked to make more T4 because there isn’t enough T4 in the blood.
- T4 (thyroxine) tests. Most of the T4 in the blood is attached to a protein called thyroxine-binding globulin. The “bound” T4 can’t get into body cells. Only about 1%–2% of T4 in the blood is unattached (“free”) and can get into cells. The free T4 and the free T4 index are both simple blood tests that measure how much unattached T4 is in the blood and available to get into cells.
How is hypothyroidism treated?
Hypothyroidism is treated with a synthetic thyroid hormone called levothyroxine, taken as a pill. Levothyroxine restores adequate thyroid hormone levels, reversing the signs and symptoms of hypothyroidism. Levothyroxine is a synthetic (laboratory-made) form of T4 that is identical to the T4 the thyroid naturally makes. You’ll likely start to feel better soon after you start treatment. The medication gradually lowers cholesterol levels elevated by the disease and may reverse any weight gain. Levothyroxine comes in brand-name and generic versions. Changing the manufacturer of the medication could alter the amount of medicine your body gets; so preferably, try to consistently take the same dose, made by the same company at all times. Often, this might be resolved by using a branded levothyroxine product.
Most people need thyroid hormone replacement with levothyroxine for life. If the brand or dosage needs to be changed, you should have blood tests for TSH done again. Your dose will be adjusted based on your TSH tests. Your doctor is likely to check your TSH level every year. Over time, doses of thyroid hormone that are too high can lead to bone loss, abnormal heart function, and abnormal heart rhythms. Doses that are too low may not relieve your symptoms. Dose adjustment may be necessary over your lifetime, including during pregnancy. You can discuss dose changes during your regular check-ups with your doctor.
The only dangers of levothyroxine are caused by taking too little or too much. If you take too little levothyroxine, your hypothyroidism will continue. If you take too much levothyroxine, you’ll develop the symptoms of hyperthyroidism—an overactive thyroid gland. The most common symptoms of too much thyroid hormone are fatigue but inability to sleep, greater appetite, nervousness, shakiness, feeling hot when other people are cold, and trouble exercising because of weak muscles, shortness of breath , and a racing, skipping heart. Patients who have hyperthyroid symptoms at any time during thyroxine replacement therapy should have their TSH tested. If it is low, indicating too much thyroid hormone, their dose needs to be lowered.
Determining proper levothyroxine dosage may take time
To determine the right dosage of levothyroxine initially, your doctor generally checks your level of TSH after six to eight weeks. After that, blood levels are generally checked six months later. Excessive amounts of the hormone can cause side effects, such as:
- Increased appetite
- Insomnia
- Heart palpitations
- Shakiness
If you have coronary artery disease or severe hypothyroidism, your doctor may start treatment with a smaller amount of medication and gradually increase the dosage. Progressive hormone replacement allows your heart to adjust to the increase in metabolism.
Levothyroxine causes virtually no side effects when used in the appropriate dose and is relatively inexpensive. If you change brands, let your doctor know to ensure you’re still receiving the right dosage.
Also, don’t skip doses or stop taking the drug because you’re feeling better. If you do, the symptoms of hypothyroidism will gradually return.
Proper absorption of levothyroxine
Certain medications, supplements and even some foods may affect your ability to absorb levothyroxine. Talk to your doctor if you eat large amounts of soy products or a high-fiber diet or you take other medications, such as:
- Iron supplements or multivitamins that contain iron
- Aluminum hydroxide, which is found in some antacids
- Calcium supplements
Levothyroxine is best taken on an empty stomach at the same time every day. Ideally, you’ll take the hormone in the morning and wait an hour before eating or taking other medications. If you take it at bedtime, wait four hours after your last meal or snack.
If you miss a dose of levothyroxine, take two pills the next day.
Subclinical hypothyroidism
If you have subclinical hypothyroidism, discuss treatment with your doctor. For a relatively mild increase in TSH, you probably won’t benefit from thyroid hormone therapy, and treatment could even be harmful. On the other hand, for a higher TSH level, thyroid hormones may improve your cholesterol level, the pumping ability of your heart and your energy level.
Follow-up
You’ll need to have your TSH checked 6 to 10 weeks after a thyroxine dose change. You may need tests more often if you’re pregnant or you’re taking a medicine that interferes with your body’s ability to use thyroxine. The goal of treatment is to get and keep your TSH in the normal range. Babies with hypothyroidism must get all their daily treatments and have their TSH levels checked as they grow, to prevent mental retardation and stunted growth. Once you’ve settled into a levothyroxine dose, you can return for TSH tests about once a year.
You need to see your doctor sooner if any of the following apply to you:
- Your symptoms return or get worse.
- You want to change your levothyroxine dose or brand, or change taking your pills with or without food.
- You gain or lose a lot of weight (as little as a 10-pound difference for those who weren’t overweight to begin with).
- You start or stop taking a drug that can interfere with absorbing thyroxine (such as certain antacids, calcium supplements and iron tablets), or you change your dose of such a drug. Medications containing estrogen also impact thyroxine doses, so any change in such a medication should prompt a re-evaluation of your thyroxine dose.
- You start or stop taking certain medicines to control seizures such as phenytoin or tegretol, as such medicines increase the rate at which thyroxine is metabolized in your body, and your dose of thyroxine may need to be adjusted.
- You’re not taking all your thyroxine pills. Tell your doctor honestly how many pills you’ve missed.
- You want to try stopping thyroxine treatment. If ever you think you’re doing well enough not to need thyroxine treatment any longer, try it only under your doctor’s close supervision. Rather than stopping your pills completely, you might ask your doctor to try lowering your dose. If your TSH goes up, you’ll know that you need to continue treatment.
What is Hashimoto’s disease?
Hashimoto disease also known as Hashimoto’s thyroiditis, chronic lymphocytic thyroiditis or autoimmune thyroiditis, is an autoimmune disease where your body’s immune system attacks your thyroid gland, preventing it from producing enough thyroid hormones (tri-iodothyronine [T3] and thyroxine [T4]). Low thyroid hormone levels may cause hypothyroidism with a range of symptoms, such as tiredness or fatigue, weight gain, intolerance to cold temperatures, dry skin or dry thinning hair, slowed heart rate, heavy or irregular menstrual periods or fertility problems. Rarely, early in the course of the disease, thyroid gland damage may lead to the release of too much thyroid hormone into your blood, causing symptoms of hyperthyroidism 26. Too much thyroid hormone (hyperthyroidism) can cause weight loss, despite an increased appetite. You might also feel anxious and find it difficult to relax.
Your thyroid gland is a butterfly-shaped gland with 2 lobes (the right lobe and the left lobe — joined by a narrow piece of the thyroid gland called the isthmus) that is located in front of your neck near the base of your throat, beneath the larynx (voice box or Adam’s apple) (Figure 1). In most people, the thyroid gland cannot be seen or felt. Your thyroid gland produces thyroid hormones, tri-iodothyronine (T3) and thyroxine (T4) (the main hormones that your thyroid gland makes) and calcitonin. The thyroid hormones, T3 (tri-iodothyronine) and T4 (thyroxine) influence important body processes such as body temperature, energy levels, growth, your digestion, muscles and heart. Thyroid hormones are important for how your body uses energy, your metabolism, so thyroid hormones affect nearly every organ in your body even the way your heart beats. You might put on weight and feel very tired and lacking in energy if your thyroid gland doesn’t make enough T3 (tri-iodothyronine) and T4 (thyroxine).
Calcitonin is another hormone produced by the thyroid gland. Calcitonin helps to control the amount of calcium circulating in your blood. Calcitonin works with a hormone called parathyroid hormone (PTH) to do this. Parathyroid hormone is made by parathyroid glands. These sit behind and are attached to the thyroid gland (see Figure 1).
In people with Hashimoto’s disease:
- the immune system makes antibodies that attack the thyroid gland (autoimmune disorder). Usually in Hashimoto’s disease, the immune system produces an antibody to thyroid peroxidase (TPO), a protein that plays an important part in thyroid hormone production. Most people with Hashimoto’s disease will have TPO (thyroid peroxidase) antibodies in their blood. Lab tests for other antibodies associated with Hashimoto’s disease may need to be done.
- large numbers of white blood cells, which are part of the immune system, build up in the thyroid gland
- the thyroid gland becomes damaged and can’t make enough thyroid hormones
Hashimoto’s disease is an autoimmune disorder affecting the thyroid gland. In Hashimoto’s thyroiditis, the immune-system cells lead to the death of the thyroid’s hormone-producing cells. Hashimoto’s disease usually results in a decline in thyroid hormones production (hypothyroidism). The symptoms of hypothyroidism might be mild, or they might be severe. They include:
- fatigue
- being unable to stand the cold
- weight gain
- constipation
- muscle pain
- dry skin, thin hair and / or brittle nails
- low sex drive (libido)
Hashimoto’s disease can also cause cognitive symptoms including:
- depression or low mood
- an inability to concentrate
- poor memory
In some cases, your thyroid gland may become noticeably larger (called a goiter) or it may shrink. Lumps or nodules may also develop in your thyroid gland.
Although Hashimoto’s disease can affect people of all ages, it’s most common in women in their 30s and 40s 27. The female-to-male ratio is at least 10:1 26. If someone in your family has had thyroid disease, you may have an increased risk for Hashimoto’s disease. No one is sure why people get Hashimoto’s disease.
If you have symptoms of hypothyroidism, see your doctor. Your doctor will examine you and may run blood tests, including testing your thyroid hormone levels.
If left untreated, hypothyroidism can lead to problems including goiter (an increase in the size of the thyroid gland), heart problems or mental health problems. Occasionally, it can lead to a potentially life-threatening disorder called myxedema coma.
While there is no cure for Hashimoto’s disease, hypothyroidism can be treated. The primary treatment of Hashimoto’s disease is thyroid hormone replacement. Most people with Hashimoto’s disease take a synthetic thyroid hormone medication called levothyroxine (Levoxyl, Synthroid, others) to treat hypothyroidism. The synthetic thyroid hormone works like the T4 hormone naturally produced by the thyroid. Your hypothyroidism can be well-controlled with thyroid hormone medicine, as long as you take the medicine as instructed by your doctor and have regular follow-up blood tests.
If you have mild hypothyroidism, you may not need to have treatment but get regular thyroid stimulating hormone (TSH) tests to monitor thyroid hormone levels.
How common is Hashimoto’s disease?
The number of people who have Hashimoto’s disease in the United States is unknown. However, Hashimoto’s disease is the most common cause of hypothyroidism the United States, which affects about 5 in 100 Americans 28.
Hashimoto is also the most common cause of hypothyroidism in those areas of the world where iodine intake is adequate. The incidence is estimated to be 0.8 per 1000 per year in men and 3.5 per 1000 per year in women 26. The prevalence of thyroid disease, in general, increases with age.
How does eating, diet, and nutrition affect Hashimoto’s disease?
The thyroid gland uses iodine, a mineral in some foods, to make thyroid hormones. However, if you have Hashimoto’s disease or other types of autoimmune thyroid disorders, you may be sensitive to harmful side effects from iodine. Eating foods that have large amounts of iodine—such as kelp, dulse, or other kinds of seaweed, and certain iodine-rich medicines—may cause hypothyroidism or make it worse. Taking iodine supplements can have the same effect.
Talk with members of your health care team about:
- what foods and beverages to limit or avoid
- whether you take iodine supplements
- any cough syrups you take that may contain iodine
However, if you are pregnant, you need to take enough iodine because the baby gets iodine from your diet. Too much iodine can cause problems as well, such as a goiter in the baby. If you are pregnant, talk with your doctor about how much iodine you need.
Researchers are looking at other ways in which diet and supplements such as vitamin D and selenium may affect Hashimoto’s disease 29. However, no specific guidance is currently available 26.
Hashimoto’s disease and gluten
There is insufficient evidence to support a gluten-free diet for all Hashimoto’s disease patients 30. Few studies have been conducted on the usage of a gluten-free diet in patients with Hashimoto’s disease 31, 32. Some research suggested a relationship between gluten consumption and the development or progression of Hashimoto’s disease. A pilot study of normal thyroid function (euthyroid) women with Hashimoto’s disease showed that gluten-free diet reduced thyroid antibody titers 31. Another study by Velija et al. 32 tested the response of subclinical hypothyroidism patients with Hashimoto’s disease treated with a gluten-free diet and selenium supplementation in restoring a normal thyroid function. After six months, normal thyroid function was restored in more patients who received selenium and had a gluten-free diet compared to the control group who supplemented selenium without any dietary intervention 32. Moreover, the reduction in serum anti-thyroid peroxidase (anti-TPO) antibody levels in the study group was significantly greater than in the control group. The results of that study suggested that the gluten-free diet together with selenium supplementation is more effective compared to only Se supplementation in Hashimoto’s disease women with subclinical hypothyroidism 32. Another study showed no reduction in thyroid autoimmunity after following a gluten-free diet 33. Pobłocki et al. 33 conducted a randomized study with euthyroid women with Hashimoto’s disease receiving levothyroxine. The control group’s diet contained gluten, and the study group was on a gluten-free diet for 12 months. During follow-up, there was a significant reduction in thyroid stimulating hormone (TSH) levels in the study group 33. Only a few studies suggest that gluten elimination may be helpful for some Hashimoto’s disease patients. It should be noted that gluten-free diet is very restrictive and difficult to follow and contributes to the risk of nutritional deficiencies. The studies conducted so far do not confirm that patients with Hashimoto’s disease should be on a gluten-free diet, therefore it is not recommended 34.
Hashimoto’s disease and anti-inflammatory diet
An anti-inflammatory diet rich in vitamins, minerals and polyphenols is recommended as diet therapy for Hashimoto’s disease 35, 36, 34. The theory behind the inflammation has to do with the leaky gut syndrome, where there is an insult to the gut mucosa, which allows the penetrance of proteins that do not typically enter the bloodstream via transporters in the gut mucosa. It is theorized that a response similar to molecular mimicry occurs, and antibodies are produced against the antigens. Unfortunately, the antigen may be very structurally similar to thyroid peroxidase, leading to antibody formation against this enzyme. The concept of an autoimmune diet is based on healing the gut and decreasing the severity of the autoimmune response.
Natural antioxidants like vitamin A, vitamin C and vitamin E are found in products of plant origin, including a wide variety of vegetables and fruits. Sources of vitamin C include broccoli, peppers, black currant, strawberries, lemons, spinach, kiwifruit, oranges, grapefruit, limes, tomatoes, raspberries, asparagus, pineapples, fennel and parsley. The best source of vitamin E is avocado, nuts, seeds, egg, milk and whole grains. In addition, vitamin A is present in foods such as liver, carrot, broccoli, butter, pumpkin, cheese, egg, mango and milk 37. According to the current findings, the Mediterranean diet may show the most benefits for Hashimoto’s disease patients with its antioxidant properties 38.
One study by Ostrowska et al. 39 assessed the effectiveness of two “reducing diets” and their effect on thyroid parameters in female obese patients with Hashimoto’s disease. All women who received levothyroxine, selenium and zinc were randomly assigned to the study group following individually balanced elimination/reducing diets, in accordance with the previously performer food sensitivity tests, and the control group following reducing diets with the same caloric content, but without product elimination. The anthropometric and thyroid parameters have changed in both groups during the nutritional intervention. This research showed that weight reduction may improve thyroid function in patients suffering from obesity and Hashimoto’s disease 39. Moreover, an individually selected elimination reducing diet was more effective than classic reducing diets with the same energy intake and macronutrient content and can lead to better therapeutic outcomes, which may cause an anti-inflammatory effect 39.
One case report 40 showed a novel approach that led to the improvement of symptoms and a reduction of thyroid antibodies in a 23-year-old woman with Hashimoto’s disease. The woman presented with symptoms of fatigue, hair loss, energy and mood disturbance, problems with insomnia and daytime napping. The thyroid antibodies were strongly positive, with a normal TSH level. Integrative treatment was started, which involved nutritional changes and micronutrient supplementation 40. This supplementation supported the methylation cycle, anti-oxidant capacity and stress management, and included vitamin C, vitamin B1, vitamin B2, vitamin B5, vitamin B6, Pyridoxal-5 Phosphate, zinc picolonate, L-5 methyltetrahydrofolate, magnesium glycinate, selenomethionine, N- Acetyl Cysteine and methylcobalamin (vitamin B12). The patient followed a paleo-style diet without grains and dairy products and increased consumption of bone broth and fermented foods as well as organic animal protein as tolerated. In addition, daily meditation and mindfulness techniques were recommended, and gentle exercise three times a week was added. After 15 months of treatment, there was a reduction in antithyroid antibodies and a significant relief of symptoms. This case demonstrated the potential benefits of an integrative approach to autoimmunity and oxidative stress in Hashimoto’s disease 40.
In a pilot study by Abbott et al. 41, women participated in a 10-week online health coaching program focused on implementing an “autoimmune protocol diet”. They applied a modified paleolithic diet. In the referred study, there were no significant changes in thyroid function markers, as well as serum antithyroid antibody concentrations, although the number of immune cells and an inflammatory processes marker (high sensitivity CRP) were decreased. These results suggest that an “autoimmune protocol” may decrease inflammation and modulate the immune system. Moreover, the therapy improves health-related quality of life (measured by 36-Item Short-Form Health Survey) and reduces symptoms of the diseases (measured by the Medical Symptoms Questionnaire) 41. A case study with a 49-year-old obese Hashimoto’s disease woman indicated that a modified autoimmune paleo low-calorie diet might improve TSH, anti-TPO antibody, body composition and lipid profile 42.
What causes Hashimoto’s disease?
Hashimoto’s disease is an autoimmune disorder. The immune system creates antibodies that attack thyroid cells as if they were bacteria, viruses or some other foreign body. The immune system wrongly enlists disease-fighting agents that damage cells and lead to cell death. What causes the immune system to attack thyroid cells is not clear. Multiple factors from the external environment and the genetic background contribute to the pathogenesis of Hashimoto’s disease 30. These genetic, environmental, and existential factors provoke the immune system to produce antibodies to thyroid antigens 43, 44, 45, 46, 47, 48, 49, 50. The most important factors associated with Hashimoto’s thyroiditis are summarized in Table 3 below.
The onset of Hashimoto’s disease may be related to 51, 52, 53, 54:
- Genetic factors. Twin studies have shown an increased concordance of autoimmune thyroiditis in monozygotic twins as compared with dizygotic twins. Danish studies have demonstrated concordance rates of 55% in monozygotic twins, compared with only 3% in dizygotic twins 3. This data suggests that 79% of predisposition is due to genetic factors, allotting 21% for environmental and sex hormone influences.
- Environmental triggers, such as infection, stress or radiation exposure
- Interactions between environmental and genetic factors.
Hypothyroidism can also be caused by:
- some medicines used to treat bipolar disorder or other mental health problems
- iodine-containing medicines used to treat abnormal heart rhythm
- exposure to toxins, such as nuclear radiation
- viruses, such as hepatitis C
Several genes have been involved in Hashimoto’s disease pathogenesis, including genes of the immune response (coded in the Human Leukocyte Antigen (HLA) complex) and thyroid function 30. Other immunoregulatory genes are involved in the development of Hashimoto’s disease, including the single nucleotide polymorphisms (SNPs) in cytotoxic T lymphocyte-associated antigen 4 (CTLA-4), protein tyrosine phosphatase non-receptor type 22 (PTPN22), and CD40 55, 43, 48, 56.
Among the environmental factors are inadequate or excessive iodine intake, infections, or the intake of certain medications 43, 48, 47, 49, 36. Several of the currently used anticancer drugs, such as interferon-alpha, may cause autoimmune thyroid dysfunction 57, 50. The role of smoking and alcohol consumption in the etiopathogenesis of Hashimoto’s disease is still not clear 30. The data suggest that moderate alcohol consumption may protect against Hashimoto’s disease and the development of overt hypothyroidism 50, 58, 59. Furthermore, some studies indicate that smoking decreases the levels of thyroid autoantibodies and the risk of hypothyroidism. However, the mechanism for these protective effects of smoking and drinking remains unclear and must be clarified with future studies 50, 58, 59. In recent years, the influence of stress on the development and course of Hashimoto’s disease has also been investigated. Some studies suggest that stress is involved in the pathogenesis of Hashimoto’s disease, while other evidence indicates that it has no effect 50, 60. A randomized controlled trial by Markomanolaki et al. 61 showed that managing stress is also important in treating Hashimoto’s disease patients. After eight weeks of stress management intervention, patients demonstrated a reduction in antithyroglobulin (anti-Tg) titers, decreased levels of stress, depression, anxiety and improved lifestyle 61. Additionally, the adequate levels of vitamin D and selenium may help prevent or delay the onset of Hashimoto’s disease 47, 49, 62, 63. Moreover, the risk of Hashimoto’s disease is increased in other autoimmune diseases 64, 50.
Most Hashimoto’s disease patients develop antibodies to a variety of thyroid antigens, the most common of which is anti-thyroid peroxidase (anti-TPO). Many also form antithyroglobulin (anti-Tg) and TSH receptor-blocking antibodies (TBII) 26. These antibodies attack the thyroid tissue, eventually leading to inadequate production of thyroid hormone. There is a small subset of the population, no more than 10-15% with the clinically evident disease, that are serum antibody-negative 26.
Table 3. Genetic, environmental and existential factors associated with Hashimoto’s thyroiditis
| Genetic Factors | Environmental Factors | Existential Factors |
|---|---|---|
| Histocompatibility genes (HLA class I and II) | Iodine | Sex |
| Immunoregulatory genes (SNPs in HLA, CTLA-4, PTPN22, CD40 genes) | Medications (e.g., interferon-α, lithium, amiodarone) | Associated diseases (e.g., type 1 diabetes mellitus, pernicious anaemia, coeliac disease, myasthenia gravis) |
| Thyroid-specific genes | Infections (e.g., hepatitis C virus) | Age |
| Genes associated with thyroid peroxidase antibody synthesis | Smoking | Pregnancy |
| Selenium | Down’s syndrome | |
| Vitamin D | Microbiome composition | |
| Alcohol | Familial aggregation | |
| Radiation Exposure |
Risk factors for Hashimoto’s disease
The following factors are associated with an increased risk of Hashimoto’s disease 29:
- Sex. Women are much more likely to get Hashimoto’s disease.
- Age. Hashimoto’s disease can occur at any age but more commonly occurs during middle age.
- Other autoimmune disease. Having another autoimmune disease — such as rheumatoid arthritis, type 1 diabetes or lupus — increases your risk of developing Hashimoto’s disease.
- Genetics and family history. You’re at higher risk for Hashimoto’s disease if others in your family have thyroid disorders or other autoimmune diseases.
- Pregnancy. Typical changes in immune function during pregnancy may be a factor in Hashimoto’s disease that begins after pregnancy.
- Excessive iodine intake. Too much iodine in the diet may function as a trigger among people already at risk for Hashimoto’s disease.
- Radiation exposure. People exposed to excessive levels of environmental radiation are more prone to Hashimoto’s disease.
Hashimoto’s disease pathophysiology
The exact mechanisms underlying Hashimoto’s disease pathogenesis are not fully understood 30. The development of Hashimoto’s disease is thought to be of autoimmune origin with lymphocyte infiltration of T and B cells, especially of CD4+ Th1 and the production of antithyroid antibodies 48, 65, 66, 43, 50. This leads to chronic inflammation and thyroid fibrosis and gradual atrophy of the thyroid tissue 66, 43, 65.
The current diagnosis is based on clinical symptoms correlating with laboratory results of elevated thyroid stimulating hormone (TSH) with normal to low thyroxine (T4) levels. It is interesting to note, however, that there is little evidence demonstrating the role of antithyroid peroxidase (anti-TPO) antibody in the pathogenesis of autoimmune thyroid disease 26. Anti-TPO antibodies can fix complement and, in test tube (in vitro), have been shown to bind and kill thyroid cells (thyrocytes). However, to date, there has been no correlation noted in human studies between the severity of disease and the level of anti-TPO antibody concentration in serum 26. Scientists do, however, know that positive serum anti-TPO antibody concentration is correlated with the active phase of Hashimoto’s disease 67. Other theories implicated immune complexes, containing thyroid directed antibodies, as culprits of thyroid destruction.
Hashimoto’s disease prevention
At the present time there is no known way to prevent Hashimoto’s disease.
Hashimoto’s disease signs and symptoms
Signs and symptoms of Hashimoto’s disease vary widely and are not specific to the disorder. Hashimoto’s disease progresses slowly over the years. Many people with Hashimoto’s disease may not notice signs or symptoms of the disease at first. An ordinary blood test may just show a thyroid hormone imbalance. Because the thyroid gland may grow and get larger, you may have a feeling of fullness or tightness in your throat, though it is usually not painful. You may have trouble swallowing food or liquids. You might have a swelling (a bump) in the front of your neck, the enlarged thyroid is called a goiter. After many years, or even decades, damage to the thyroid may cause the gland to shrink and the goiter to disappear.
Some people with Hashimoto’s disease have symptoms such as tiredness, forgetfulness, depression, coarse dry skin, slow heartbeat, weight gain, constipation and intolerance to cold. A blood test can tell if your thyroid gland is underactive. Other blood tests can be done to look for Hashimoto’s disease.
Eventually, the decline in thyroid hormone production can result in hypothyroidism with any of the following:
- Fatigue and sluggishness
- Increased sensitivity to cold
- Increased sleepiness
- Dry skin
- Constipation
- Muscle weakness
- Muscle aches, tenderness and stiffness
- Joint pain and stiffness
- Irregular or excessive menstrual bleeding
- Depression
- Problems with memory or concentration
- Swelling of the thyroid (goiter)
- A puffy face
- Brittle nails
- Hair loss
- Enlargement of the tongue
Because these symptoms could result from any number of disorders, it’s important to see your doctor as soon as possible for a timely and accurate diagnosis.
Hashimoto’s disease complications
Thyroid hormones are essential for the healthy function of many body systems. Therefore, when Hashimoto’s disease and hypothyroidism are left untreated, many complications can occur. These include:
- Goiter. A goiter is enlargement of the thyroid. As thyroid hormone production declines due to Hashimoto’s disease, the thyroid receives signals from the pituitary gland to make more. This cycle may result in a goiter. It’s generally not uncomfortable, but a large goiter can affect your appearance and may interfere with swallowing or breathing.
- Heart problems. Hypothyroidism can result in poor heart function, an enlarged heart and irregular heartbeats. It can also result in high levels of low-density lipoprotein (LDL) cholesterol — the “bad” cholesterol — that is a risk factor for cardiovascular disease and heart failure.
- Mental health issues. Depression or other mental health disorders may occur early in Hashimoto’s disease and may become more severe over time.
- Sexual and reproductive dysfunction. In women, hypothyroidism can result in a reduced sexual desire (libido), an inability to ovulate, and irregular and excessive menstrual bleeding. Men with hypothyroidism may have a reduced libido, erectile dysfunction and a lowered sperm count.
- Poor pregnancy outcomes. Hypothyroidism during pregnancy may increase the risk of a miscarriage or preterm birth. Babies born to women with untreated hypothyroidism are at risk for decreased intellectual abilities, autism, speech delays and other developmental disorders.
- Myxedema coma. This rare, life-threatening condition can develop due to long-term, severe, untreated hypothyroidism. Its signs and symptoms include drowsiness followed by profound lethargy and unconsciousness. A myxedema coma may be triggered by exposure to cold, sedatives, infection or other stress on your body. Myxedema requires immediate emergency medical treatment.
How is the diagnosis of Hashimoto’s disease made?
The diagnosis of Hashimoto’s thyroiditis may be made when patients present with symptoms of hypothyroidism, often accompanied by a goiter (an enlarged thyroid gland) on physical examination, and laboratory testing of hypothyroidism, which is an elevated thyroid stimulating hormone (TSH) with or without a low thyroid hormone (Free thyroxine [Free T4]) levels. Anti-thyroid peroxidase (anti-TPO) antibody, when measured, is usually elevated. The presence of anti-thyroid peroxidase (anti-TPO) and anti-thyroglobulin antibodies suggests Hashimoto thyroiditis, however, 10% of patients may be antibody negative. However, to date, there has been no correlation noted in human studies between the severity of disease and the level of anti-thyroid peroxidase (anti-TPO) antibody concentration in serum. However, scientists know that positive serum anti-TPO antibody concentration is correlated with the active phase of Hashimoto’s disease 67.
Occasionally, Hashimoto’s disease may be diagnosed early, especially in people with a strong family history of thyroid disease. Anti-thyroid peroxidase (anti-TPO) antibody may be positive, but thyroid hormone levels may be normal or there may only be isolated mild elevation of serum TSH is seen. Symptoms of hypothyroidism may be absent.
- Anemia is present in 30% to 40%.
- There can be decreased glomerular filtration rate (GFR), renal plasma flow, and renal free water clearance with resultant hyponatremia.
- Creatine kinase is frequently elevated.
- Prolactin levels may be elevated.
- Elevated total cholesterol, LDL, and triglyceride levels can occur.
A thyroid ultrasound assesses thyroid size, echotexture, and whether thyroid nodules are present; however, it is usually not necessary for diagnosing the conditioning the majority 68.
On pathologic examination, there is a diffuse, symmetric enlargement of the thyroid. The capsule is often intact with a prominent pyramidal lobe. When cut, the surface is similar to that of lymph nodes, with a pale brown to yellow color. Interlobular fibrosis may or may not be present. Atrophy may also occur and in some patients, the gland may become nodular or asymmetric. However, necrosis or calcification does not occur and would suggest a different diagnosis.
Antibody tests
More than one disease process can lead to hypothyroidism. To determine if Hashimoto’s disease is the cause of hypothyroidism, your doctor will order an antibody test.
The intended purpose of an antibody is to flag disease-causing foreign agents that need to be destroyed by other actors in the immune system. In an autoimmune disorder, the immune system produces rogue antibodies that target healthy cells or proteins in the body.
Usually in Hashimoto’s disease, the immune system produces an antibody to thyroid peroxidase (anti-TPO), a protein that plays an important part in thyroid hormone production. Most people with Hashimoto’s disease will have TPO antibodies (anti-TPO) in their blood. Lab tests for other antibodies associated with Hashimoto’s disease may also need to be done.
Thyroglobulin antibodies (Tg) can also be a sign of Hashimoto disease. Most people with Hashimoto disease have high levels of both thyroglobulin antibodies (anti-Tg) and TPO antibodies (anti-TPO).
Circulating antibody to thyroid peroxidase (anti-TPO) are found in about 90% of Hashimoto’s disease patients. Anti-thyroglobulin antibodies (anti-Tg) are less sensitive (positive in about 60–80% of patients) and less specific than antibody to thyroid peroxidase (anti-TPO) 66, 43, 69.
You probably won’t need other tests to confirm you have Hashimoto’s disease. However, if your doctor suspects Hashimoto’s disease but you don’t have antithyroid antibodies in your blood, you may have an ultrasound of your thyroid. The ultrasound images can show the size of your thyroid and other features of Hashimoto’s disease. The ultrasound also can rule out other causes of an enlarged thyroid, such as thyroid nodules—small lumps in the thyroid gland.
How is Hashimoto’s disease treated?
How your doctors treat Hashimoto’s disease usually depends on whether your thyroid is damaged enough to cause hypothyroidism. If you don’t have hypothyroidism or you have mild hypothyroidism, your doctor may choose to simply check your symptoms and do regular thyroid stimulating hormone (TSH) tests to monitor your thyroid hormone levels.
Most people with Hashimoto’s disease need take a synthetic thyroid hormone medication called levothyroxine (Levoxyl, Synthroid, others) to treat hypothyroidism. The synthetic thyroid hormone works like the thyroxine (T4) hormone naturally produced by your thyroid. Prescribed in pill form for many years, this medicine is now also available as a liquid and in a soft gel capsule 29. These newer formulas may be helpful to people with digestive problems that affect how the thyroid hormone pill is absorbed.
Some foods and supplements can affect how well your body absorbs levothyroxine. Examples include grapefruit juice, espresso coffee, soy, and multivitamins that contain iron or calcium 28, 70. Taking levothyroxine on an empty stomach can prevent this from happening. Your doctor may ask you to take the levothyroxine in the morning, 30 to 60 minutes before you eat your first meal.
Your doctor will give you a blood test about 6 to 8 weeks after you begin taking levothyroxine and adjust your dose if needed. Each time you change your dose, you’ll have another blood test. Once you’ve reached a dose that’s working for you, your doctor will likely repeat the blood test in 6 months and then once a year.
Never stop taking your levothyroxine or take a higher dose without talking with your doctor first. Taking too much thyroid hormone medicine can cause serious problems, such as atrial fibrillation or osteoporosis 53.
Thyroxine (T4) hormone replacement therapy
Hypothyroidism associated with Hashimoto’s disease is treated with a synthetic hormone called levothyroxine (Levoxyl, Synthroid, others). The recommended dose of levothyroxine is 1.6 to 1.8 mcg/kg/day 26. The synthetic hormone works like the thyroxine (T4) hormone naturally produced by the thyroid. The treatment goal is to restore and maintain adequate thyroxine (T4) hormone levels and improve symptoms of hypothyroidism. You will need this treatment for the rest of your life.
Monitoring the dosage
Your doctor will determine a dosage of levothyroxine that’s appropriate for your age, weight, current thyroid production, other medical conditions and other factors. Your doctor will retest your TSH (thyroid stimulating hormone) levels about 6 to 10 weeks later and adjust the dosage as necessary.
Once the best dosage is determined, you will continue to take the medication once a day. You’ll need follow-up tests once a year to monitor TSH (thyroid stimulating hormone) levels or any time after your doctor changes your dosage.
A levothyroxine pill is usually taken in the morning before you eat. Talk to your doctor if you have any questions about when or how to take the pill. Also, ask what to do if you accidentally skip a dose. If your health insurance requires you to switch to a generic drug or a different brand, talk to your doctor.
Precautions
Because levothyroxine acts like natural thyroxine (T4) in your body, there are generally no side effects as long as the treatment is resulting in “natural” levels of thyroxine (T4) for your body.
Too much thyroid hormone can worsen bone loss that causes weak, brittle bones (osteoporosis) or cause irregular heartbeats (arrhythmias) the most common being atrial fibrillation.
Effects of other substances
Certain medications, supplements and foods may affect your ability to absorb levothyroxine. It may be necessary to take levothyroxine at least four hours before these substances. Talk to your doctor about any of the following:
- Soy products
- High-fiber foods
- Iron supplements, including multivitamins that contain iron
- Cholestyramine (Prevalite), a medication used to lower blood cholesterol levels
- Aluminum hydroxide, which is found in some antacids
- Sucralfate, an ulcer medication
- Calcium supplements
Triiodothyronine (T3) hormone replacement therapy
Naturally produced thyroxine (T4) is converted into another thyroid hormone called triiodothyronine (T3). The thyroxine (T4) replacement hormone is also converted into triiodothyronine (T3), and for most people the thyroxine (T4) replacement therapy results in an adequate supply of triiodothyronine (T3) for the body.
For people who need better symptom control, a doctor also may prescribe a synthetic triiodothyronine (T3) (Cytomel) or a synthetic T4 and T3 combination. Side effects of triiodothyronine (T3) hormone replacement include rapid heartbeat, insomnia and anxiety. These treatments may be tested with a trial period of 3 to 6 months.
Alternative medicine
Products with triiodothyronine (T3) and thyroxine (T4) hormones derived from pigs or other animals are available as prescriptions or as dietary supplements, such as Armour Thyroid, in the United States. Concerns about these products include the following:
- The balance of thyroxine (T4) and triiodothyronine (T3) in animals isn’t the same as in humans.
- The exact amount of thyroxine (T4) and triiodothyronine (T3) in each batch of a natural extract product can vary, leading to unpredictable levels of these hormones in your blood.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association [published correction appears in Endocrine Practice. 2013;19(1):175]. Endocrine Practice. 2012;18(6):988–1028. doi: 10.4158/EP12280.GL
- Mincer DL, Jialal I. Hashimoto Thyroiditis. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459262
- Brix TH, Hegedüs L, Gardas A, Banga JP, Nielsen CH. Monozygotic twin pairs discordant for Hashimoto’s thyroiditis share a high proportion of thyroid peroxidase autoantibodies to the immunodominant region A. Further evidence for genetic transmission of epitopic “fingerprints”. Autoimmunity. 2011 May;44(3):188-94. doi: 10.3109/08916934.2010.518575
- Pearce EN, Farwell AP, Braverman LE. Thyroiditis. New England Journal of Medicine. 2003;348(26):2646–2655. doi: 10.1056/NEJMra021194. Erratum in: New England Journal of Medicine. 2003;349(6):620. https://www.nejm.org/doi/10.1056/NEJMra021194
- Zimmermann MB. Iodine deficiency. Endocr Rev. 2009 Jun;30(4):376-408. doi: 10.1210/er.2009-0011
- Jonklaas, J., Bianco, A. C., Bauer, A. J., Burman, K. D., Cappola, A. R., Celi, F. S., Cooper, D. S., Kim, B. W., Peeters, R. P., Rosenthal, M. S., Sawka, A. M., & American Thyroid Association Task Force on Thyroid Hormone Replacement (2014). Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association task force on thyroid hormone replacement. Thyroid : official journal of the American Thyroid Association, 24(12), 1670–1751. https://doi.org/10.1089/thy.2014.0028
- Ragusa F, Fallahi P, Elia G, et al. Hashimotos’ thyroiditis: epidemiology, pathogenesis, clinic, and therapy. Best Practice & Research Clinical Endocrinology & Metabolism. 2019;33(6):101367. doi: 10.1016/j.beem.2019.101367
- Hays MT. Localization of human thyroxine absorption. Thyroid. 1991 Summer;1(3):241-8. doi: 10.1089/thy.1991.1.241
- Fish LH, Schwartz HL, Cavanaugh J, Steffes MW, Bantle JP, Oppenheimer JH. Replacement dose, metabolism, and bioavailability of levothyroxine in the treatment of hypothyroidism. Role of triiodothyronine in pituitary feedback in humans. N Engl J Med. 1987 Mar 26;316(13):764-70. doi: 10.1056/NEJM198703263161302
- Burch HB. Drug effects on the thyroid. New England Journal of Medicine. 2019;381(8):749–761. doi: 10.1056/NEJMra1901214
- Jonklaas, J., Bianco, A. C., Bauer, A. J., Burman, K. D., Cappola, A. R., Celi, F. S., Cooper, D. S., Kim, B. W., Peeters, R. P., Rosenthal, M. S., Sawka, A. M., & American Thyroid Association Task Force on Thyroid Hormone Replacement (2014). Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid : official journal of the American Thyroid Association, 24(12), 1670–1751. https://doi.org/10.1089/thy.2014.0028
- Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017;390(10101):1550–1562. doi: 10.1016/S0140-6736(17)30703-1
- Hashimoto’s Disease. https://www.niddk.nih.gov/health-information/endocrine-diseases/hashimotos-disease
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press, 2001. https://www.nap.edu/read/10026/chapter/2
- World Health Organization. United Nations Children’s Fund & International Council for the Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. 3rd ed. Geneva, Switzerland: WHO, 2007. http://apps.who.int/iris/bitstream/handle/10665/43781/9789241595827_eng.pdf;jsessionid=2E9F56538AEFD33C83934FB34BD4E8C4
- WHO Secretariat, Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007 Dec;10(12A):1606-11. doi: 10.1017/S1368980007361004. Erratum in: Public Health Nutr. 2008 Mar;11(3):327.
- USDA, FDA, and ODS-NIH Database for the Iodine Content of Common Foods Release 1.0. 2020. https://www.ars.usda.gov/ARSUSERFILES/80400535/DATA/IODINE/IODINE_DATABASE_PDFVersion_2020.PDF
- Pennington JA, Young B. Iron, zinc, copper, manganese, selenium, and iodine in foods from the United States Total Diet Studyexternal link disclaimer. J Food Compost Anal. 1990 June;3(2):166-184. https://www.sciencedirect.com/science/article/abs/pii/088915759090022E
- Ershow AG, Skeaff SA, Merkel JM, Pehrsson PR. Development of Databases on Iodine in Foods and Dietary Supplements. Nutrients. 2018 Jan 17;10(1):100. doi: 10.3390/nu10010100
- Food Labeling: Revision of the Nutrition and Supplement Facts Labels. https://www.federalregister.gov/documents/2016/05/27/2016-11867/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels
- Patterson KY, Spungen JH, Roseland JM, Pehrsson PR, Ershow AG, Gahche JJ. USDA-FDA-ODS database for the iodine content of common foods (release one). Iodine database PDF. Methods and Application of Food Composition Laboratory, Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture, Beltsville MD. July 2020. https://www.ars.usda.gov/ARSUSERFILES/80400535/DATA/IODINE/IODINE_DATABASE.PDF
- Pennington JAT, Schoen SA, Salmon GD, Young B, Johnson RD, Marts RW. Composition of Core Foods of the U.S. Food Supply, 1982-1991. III. Copper, Manganese, Selenium, and Iodine. J Food Comp Anal. 1995;8(2):171-217. https://www.sciencedirect.com/science/article/abs/pii/S0889157585710149
- Teas J, Pino S, Critchley A, Braverman LE. Variability of iodine content in common commercially available edible seaweeds. Thyroid. 2004 Oct;14(10):836-41. doi: 10.1089/thy.2004.14.836
- Patil N, Rehman A, Jialal I. Hypothyroidism. [Updated 2021 Jan 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519536
- Hypothyroidism (Underactive). https://www.thyroid.org/hypothyroidism
- Mincer DL, Jialal I. Hashimoto Thyroiditis. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459262
- Hashimoto’s Disease: What It Is and How It’s Treated. https://www.aafp.org/pubs/afp/issues/2000/0215/p1054.html
- Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, Pessah-Pollack R, Singer PA, Woeber KA; American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012 Nov-Dec;18(6):988-1028. doi: 10.4158/EP12280.GL. Erratum in: Endocr Pract. 2013 Jan-Feb;19(1):175.
- Ragusa F, Fallahi P, Elia G, Gonnella D, Paparo SR, Giusti C, Churilov LP, Ferrari SM, Antonelli A. Hashimotos’ thyroiditis: Epidemiology, pathogenesis, clinic and therapy. Best Pract Res Clin Endocrinol Metab. 2019 Dec;33(6):101367. doi: 10.1016/j.beem.2019.101367
- Mikulska AA, Karaźniewicz-Łada M, Filipowicz D, Ruchała M, Główka FK. Metabolic Characteristics of Hashimoto’s Thyroiditis Patients and the Role of Microelements and Diet in the Disease Management-An Overview. Int J Mol Sci. 2022 Jun 13;23(12):6580. doi: 10.3390/ijms23126580
- Krysiak R., Szkróbka W., Okopień B. The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp. Clin. Endocrinol. Diabetes. 2019;127:417–422. doi: 10.1055/a-0653-7108
- Velija A.Z., Hadzovic-Dzuvo A., Al T.D. Endocrine Abstracts. Volume 70 Bioscientifica; Bristol, UK: 2020. The Effect of Selenium Supplementation and Gluten-Free Diet in Patients with Subclinical Hypothyroidism Affected by Autoimmune Thyroiditis.
- Pobłocki J., Pańka T., Szczuko M., Telesiński A., Syrenicz A. Whether a Gluten-Free Diet Should Be Recommended in Chronic Autoimmune Thyroiditis or Not?—A 12-Month Follow-Up. J. Clin. Med. 2021;10:3240. doi: 10.3390/jcm10153240
- Szczuko M., Syrenicz A., Szymkowiak K., Przybylska A., Szczuko U., Pobłocki J., Kulpa D. Doubtful Justification of the Gluten-Free Diet in the Course of Hashimoto’s Disease. Nutrients. 2022;14:1727. doi: 10.3390/nu14091727
- Kawicka A., Regulska-Ilow B., Regulska-Ilow B. Metabolic Disorders and Nutritional Status in Autoimmune Thyroid Diseases. Postepy Hig. Med. Doswiadczalnej Online. 2015;69:80–90. doi: 10.5604/17322693.1136383
- Ihnatowicz P., Drywień M., Wątor P., Wojsiat J. The Importance of Nutritional Factors and Dietary Management of Hashimoto’s Thyroiditis. Ann. Agric. Environ. Med. 2020;27:184–193. doi: 10.26444/aaem/112331
- Landete J.M. Dietary Intake of Natural Antioxidants: Vitamins and Polyphenols. Crit. Rev. Food Sci. Nutr. 2013;53:706–721. doi: 10.1080/10408398.2011.555018
- Ruggeri R.M., Giovinazzo S., Barbalace M.C., Cristani M., Alibrandi A., Vicchio T.M., Giuffrida G., Aguennouz M.H., Malaguti M., Angeloni C., et al. Influence of Dietary Habits on Oxidative Stress Markers in Hashimoto’s Thyroiditis. Thyroid. 2021;31:96–105. doi: 10.1089/thy.2020.0299
- Ostrowska L., Gier D., Zyśk B. The Influence of Reducing Diets on Changes in Thyroid Parameters in Women Suffering from Obesity and Hashimoto’s Disease. Nutrients. 2021;13:862. doi: 10.3390/nu13030862
- Avard N., Grant S. A Case Report of a Novel, Integrative Approach to Hashimoto’s Thyroiditis with Unexpected Results. Adv. Integr. Med. 2018;5:75–79. doi: 10.1016/j.aimed.2018.03.003
- Abbott R.D., Sadowski A., Alt A.G. Efficacy of the Autoimmune Protocol Diet as Part of a Multi-Disciplinary, Supported Lifestyle Intervention for Hashimoto’s Thyroiditis. Cureus. 2019;11:e4556. doi: 10.7759/cureus.4556
- Al-Bayyari N.S. Successful Dietary Intervention Plan for Hashimoto’s Thyroiditis: A Case Study. Rom. J. Diabetes Nutr. Metab. Dis. 2020;27:381–385.
- Ragusa F., Fallahi P., Elia G., Gonnella D., Paparo S.R., Giusti C., Churilov L.P., Ferrari S.M., Antonelli A. Hashimotos’ Thyroiditis: Epidemiology, Pathogenesis, Clinic and Therapy. Best Pract. Res. Clin. Endocrinol. Metab. 2019;33:101367. doi: 10.1016/j.beem.2019.101367
- Shukla S.K., Singh G., Ahmad S., Pant P. Infections, Genetic and Environmental Factors in Pathogenesis of Autoimmune Thyroid Diseases. Microb. Pathog. 2018;116:279–288. doi: 10.1016/j.micpath.2018.01.004
- Weetman A.P. An Update on the Pathogenesis of Hashimoto’s Thyroiditis. J. Endocrinol. Invest. 2021;44:883–890. doi: 10.1007/s40618-020-01477-1
- Ferrari S.M., Fallahi P., Antonelli A., Benvenga S. Environmental Issues in Thyroid Diseases. Front. Endocrinol. 2017;8:50. doi: 10.3389/fendo.2017.00050
- Wiersinga W.M. Clinical Relevance of Environmental Factors in the Pathogenesis of Autoimmune Thyroid Disease. Endocrinol. Metab. 2016;31:213–222. doi: 10.3803/EnM.2016.31.2.213
- Ralli M., Angeletti D., Fiore M., D’Aguanno V., Lambiase A., Artico M., de Vincentiis M., Greco A. Hashimoto’s Thyroiditis: An Update on Pathogenic Mechanisms, Diagnostic Protocols, Therapeutic Strategies, and Potential Malignant Transformation. Autoimmun. Rev. 2020;19:102649. doi: 10.1016/j.autrev.2020.102649
- Effraimidis G., Wiersinga W.M. Mechanisms in Endocrinology: Autoimmune Thyroid Disease: Old and New Players. Eur. J. Endocrinol. 2014;170:R241–R252. doi: 10.1530/EJE-14-0047
- Ajjan R.A., Weetman A.P. The Pathogenesis of Hashimoto’s Thyroiditis: Further Developments in Our Understanding. Horm. Metab. Res. 2015;47:702–710. doi: 10.1055/s-0035-1548832
- Leung AKC, Leung AAC. Evaluation and management of the child with hypothyroidism. World J Pediatr. 2019 Apr;15(2):124-134. doi: 10.1007/s12519-019-00230-w
- Yuan J, Sun C, Jiang S, Lu Y, Zhang Y, Gao XH, Wu Y, Chen HD. The Prevalence of Thyroid Disorders in Patients With Vitiligo: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2019 Jan 15;9:803. doi: 10.3389/fendo.2018.00803
- Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017 Sep 23;390(10101):1550-1562. doi: 10.1016/S0140-6736(17)30703-1
- Ott J, Promberger R, Kober F, Neuhold N, Tea M, Huber JC, Hermann M. Hashimoto’s thyroiditis affects symptom load and quality of life unrelated to hypothyroidism: a prospective case-control study in women undergoing thyroidectomy for benign goiter. Thyroid. 2011 Feb;21(2):161-7. doi: 10.1089/thy.2010.0191. Epub 2010 Dec 27. Erratum in: Thyroid. 2011 Apr;21(4):467.
- Klubo-Gwiezdzinska J., Wartofsky L. Hashimoto Thyroiditis: An Evidence-Based Guide to Etiology, Diagnosis and Treatment. Pol. Arch. Intern. Med. 2022;132:16222. doi: 10.20452/pamw.16222
- Kust D., Matesa N. The Impact of Familial Predisposition on the Development of Hashimoto’s Thyroiditis. Acta Clin. Belg. 2020;75:104–108. doi: 10.1080/17843286.2018.1555115
- Torino F., Barnabei A., Paragliola R., Baldelli R., Appetecchia M., Corsello S.M. Thyroid Dysfunction as an Unintended Side Effect of Anticancer Drugs. Thyroid. 2013;23:1345–1366. doi: 10.1089/thy.2013.0241
- Carlé A., Pedersen I.B., Knudsen N., Perrild H., Ovesen L., Rasmussen L.B., Jørgensen T., Laurberg P. Moderate Alcohol Consumption May Protect against Overt Autoimmune Hypothyroidism: A Population-Based Case-Control Study. Eur. J. Endocrinol. 2012;167:483–490. doi: 10.1530/EJE-12-0356
- Effraimidis G., Tijssen J.G.P., Wiersinga W.M. Alcohol Consumption as a Risk Factor for Autoimmune Thyroid Disease: A Prospective Study. Eur. Thyroid J. 2012;1:99–104. doi: 10.1159/000338920
- Effraimidis G., Tijssen J.G.P., Brosschot J.F., Wiersinga W.M. Involvement of Stress in the Pathogenesis of Autoimmune Thyroid Disease: A Prospective Study. Psychoneuroendocrinology. 2012;37:1191–1198. doi: 10.1016/j.psyneuen.2011.12.009
- Markomanolaki ZS, Tigani X, Siamatras T, Bacopoulou F, Tsartsalis A, Artemiadis A, Megalooikonomou V, Vlachakis D, Chrousos GP, Darviri C. Stress Management in Women with Hashimoto’s thyroiditis: A Randomized Controlled Trial. J Mol Biochem. 2019;8(1):3-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6688766
- Rostami R., Nourooz-Zadeh S., Mohammadi A., Khalkhali H.R., Ferns G., Nourooz-Zadeh J. Serum Selenium Status and Its Interrelationship with Serum Biomarkers of Thyroid Function and Antioxidant Defense in Hashimoto’s Thyroiditis. Antioxidants. 2020;9:1070. doi: 10.3390/antiox9111070
- Mazokopakis EE, Papadomanolaki MG, Tsekouras KC, Evangelopoulos AD, Kotsiris DA, Tzortzinis AA. Is vitamin D related to pathogenesis and treatment of Hashimoto’s thyroiditis? Hell J Nucl Med. 2015 Sep-Dec;18(3):222-7.
- Wiebolt J., Achterbergh R., den Boer A., van der Leij S., Marsch E., Suelmann B., de Vries R., van Haeften T.W. Clustering of Additional Autoimmunity Behaves Differently in Hashimoto’s Patients Compared with Graves’ Patients. Eur. J. Endocrinol. 2011;164:789–794. doi: 10.1530/EJE-10-1172
- Rydzewska M., Jaromin M., Pasierowska I.E., Stożek K., Bossowski A. Role of the T and B Lymphocytes in Pathogenesis of Autoimmune Thyroid Diseases. Thyroid Res. 2018;11:2. doi: 10.1186/s13044-018-0046-9
- Caturegli P., De Remigis A., Rose N.R. Hashimoto Thyroiditis: Clinical and Diagnostic Criteria. Autoimmun. Rev. 2014;13:391–397. doi: 10.1016/j.autrev.2014.01.007
- Williams DE, Le SN, Godlewska M, Hoke DE, Buckle AM. Thyroid Peroxidase as an Autoantigen in Hashimoto’s Disease: Structure, Function, and Antigenicity. Horm Metab Res. 2018 Dec;50(12):908-921. doi: 10.1055/a-0717-5514
- Yoo WS, Chung HK. Recent Advances in Autoimmune Thyroid Diseases. Endocrinol Metab (Seoul). 2016 Sep;31(3):379-385. doi: 10.3803/EnM.2016.31.3.379
- Iddah M.A., Macharia B.N. Autoimmune Thyroid Disorders. ISRN Endocrinol. 2013;2013:e509764. doi: 10.1155/2013/509764
- Burch HB. Drug Effects on the Thyroid. N Engl J Med. 2019 Aug 22;381(8):749-761. doi: 10.1056/NEJMra1901214