What is Osteoporosis
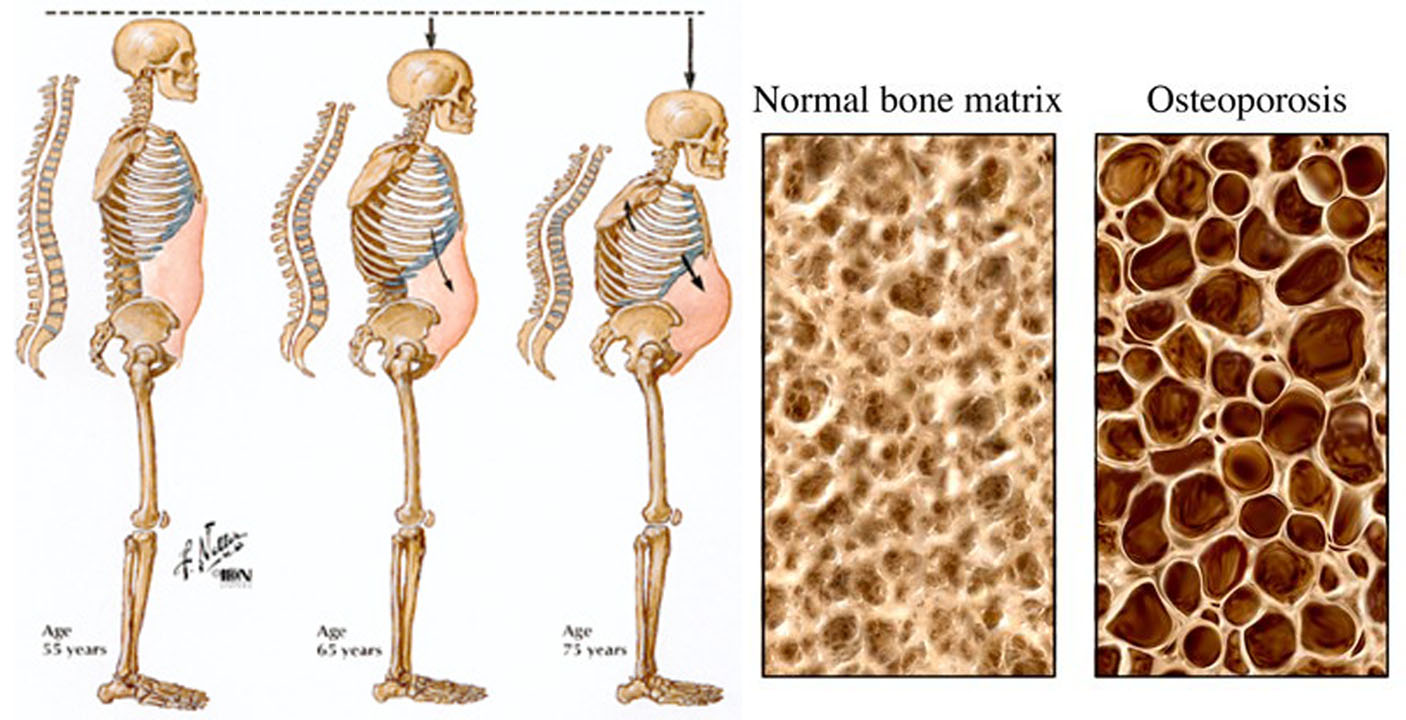
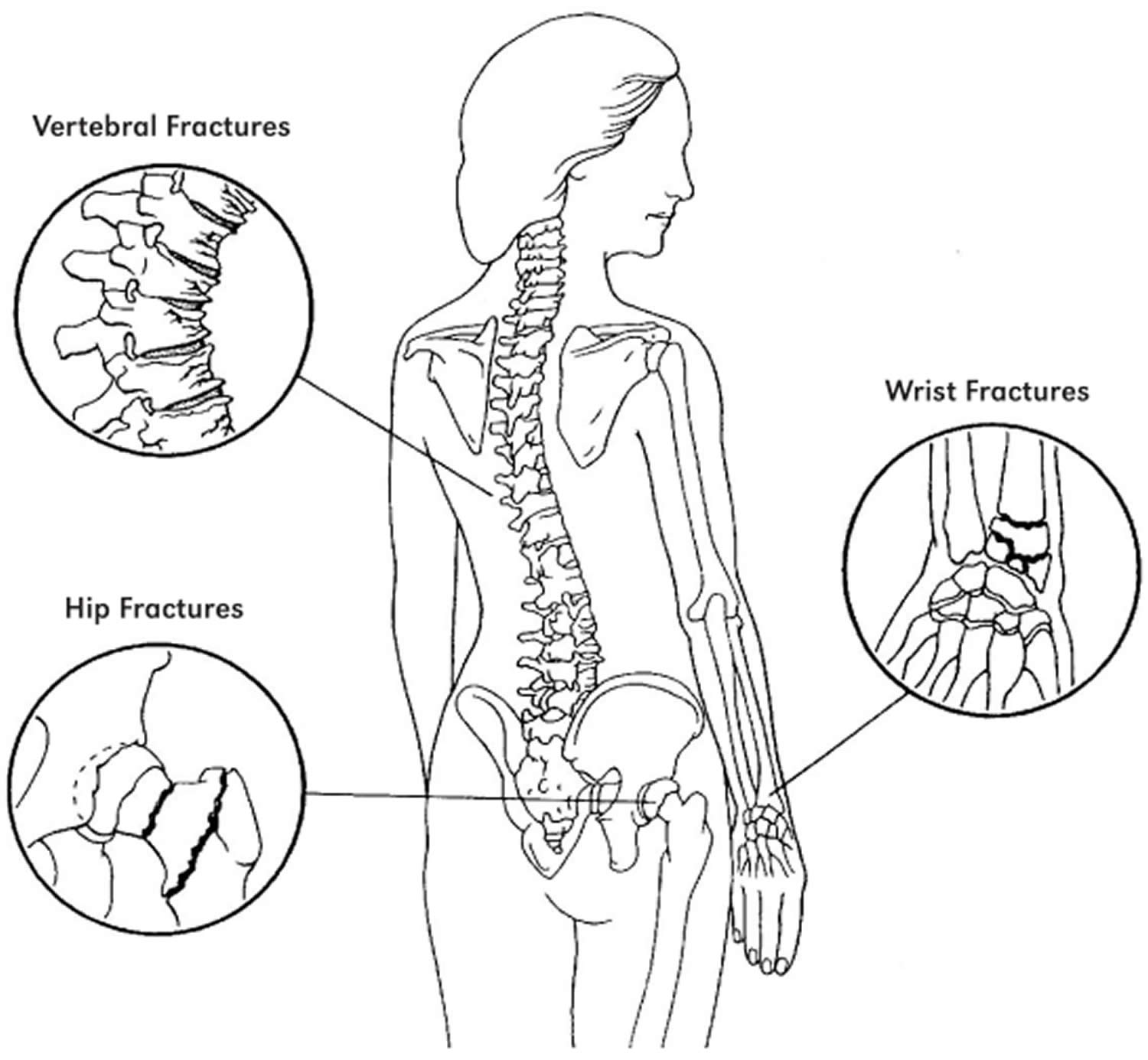
Osteoporosis literally means “porous bone.” Osteoporosis is a disease of the bones that causes you to lose bone mass. Having osteoporosis raises your risk of experiencing fractures 1, 2. Osteoporosis is characterized by too little bone formation, excessive bone loss, or a combination of both, leading to bone fragility and an increased risk of fractures of the hip, spine and wrist 3.
Osteoporosis occurs most often in older adults. Osteoporosis affects men and women of all races. But white and Asian women, especially older women who are past menopause, are at highest risk. This is due to several factors. Women have less bone mass than men to begin with. Women also tend to live longer and absorb less calcium. In women, the rate of bone loss speeds up after menopause, when estrogen levels decrease. Since the ovaries make estrogen, faster bone loss may occur if both ovaries are removed by surgery.
Bone is living tissue that is constantly being broken down and replaced. Normally, bone formation and resorption are closely balanced. Osteoblasts (cells that make the organic matrix of bone and then mineralize bone) and osteoclasts (cells that resorb bone) are regulated by parathyroid hormone (PTH), calcitonin, estrogen, vitamin D, various cytokines, and other local factors such as prostaglandins 4. Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
You may not know you have osteoporosis until your symptoms are severe. There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms of osteoporosis that include:
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped posture or a hunched back
- A bone that breaks much more easily than expected
Signs of osteoporosis include frequent broken bones or fractures, low back pain, or a hunched back. You may get shorter over time due to osteoporosis. Osteoporosis can cause your vertebrae (the bones in your spine) to collapse. These problems tend to occur after a lot of bone calcium has already been lost.
The good news is that medications, healthy diet and weight-bearing exercise can help prevent bone loss or strengthen already weak bones.
To diagnose osteoporosis, your doctor will do a bone density scan called a dual energy X-ray absorptiometry (DEXA or DXA) scan. This is a common test that measures your bone density. The DEXA bone scan often checks your hips, spine, and wrist. These are the most common places to have osteoporosis.
The American Academy of Family Physicians does not recommend that doctors use DEXA scans for women younger than 65 or men younger than 70 unless there are risk factors 5. The American Academy of Family Physicians recommends that women who are 65 years and older or have an equal or greater fracture risk be screened for osteoporosis 5.
What is Bone
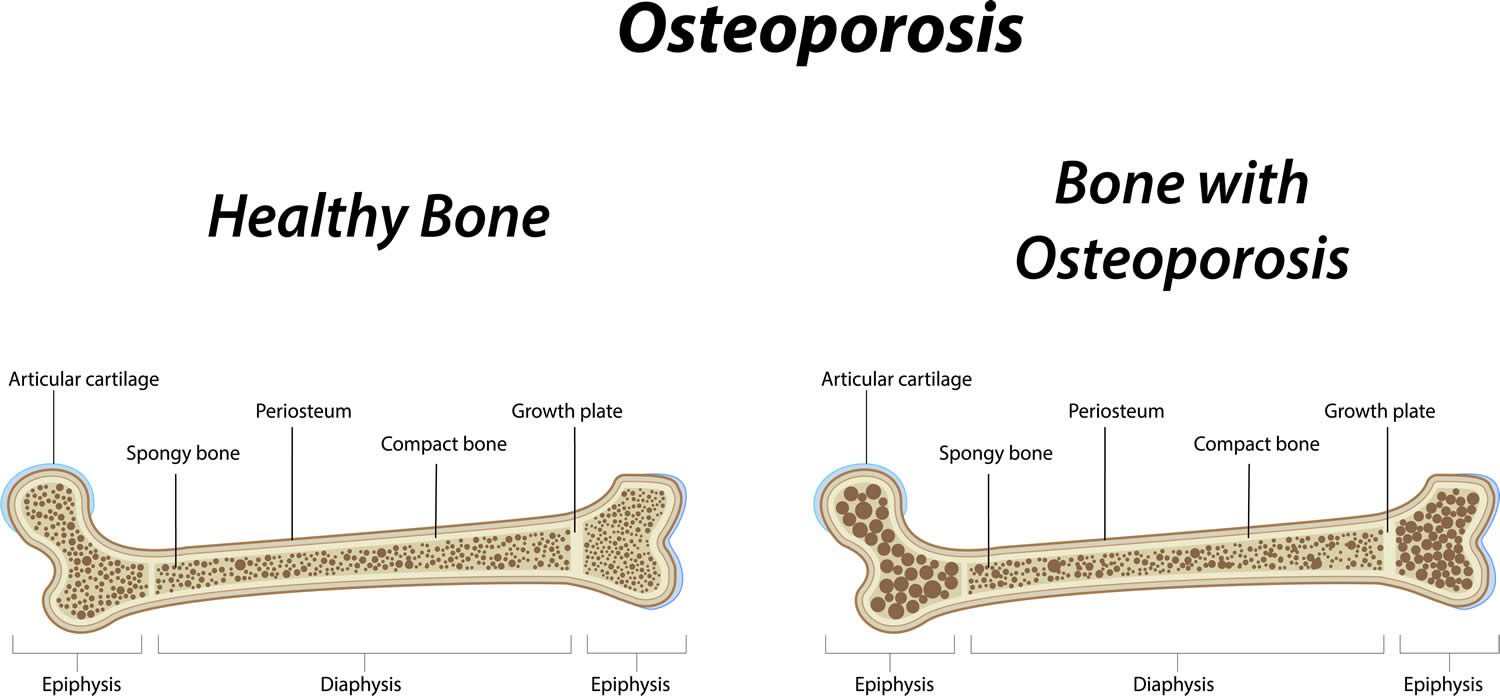
To understand osteoporosis, it is important to learn about bone. Made mostly of collagen, bone is living, growing tissue. Collagen is a protein that provides a soft framework, and calcium phosphate is a mineral that adds strength and hardens the framework. This combination of collagen and calcium makes bone strong and flexible enough to withstand stress. More than 99 percent of the body’s calcium is contained in the bones and teeth. The remaining 1 percent is found in the blood 6.
Two types of bone found in the body—cortical and trabecular. Cortical bone is dense and compact. It forms the outer layer of the bone. Trabecular bone makes up the inner layer of the bone and has a spongy, honeycomb-like structure.
Bone Remodeling: throughout life, bone is constantly renewed through a two-part process called remodeling. This process consists of resorption and formation. During resorption, special cells called osteoclasts break down and remove old bone tissue. During bone formation, new bone tissue is laid down to replace the old. Several hormones including calcitonin, parathyroid hormone, vitamin D, estrogen (in women), and testosterone (in men), among others, regulate osteoclast and osteoblast function 6.
Think of bone as a bank account where you “deposit” and “withdraw” bone tissue. During childhood and the teenage years, new bone is added to the skeleton faster than old bone is removed. As a result, bones become larger, heavier, and denser. For most people, bone formation continues at a faster pace than removal until bone mass peaks during the third decade of life.
After age 25, bone “withdrawals” can begin to exceed “deposits.” For many people, this bone loss can be prevented by continuing to get calcium, vitamin D, and exercise and by avoiding tobacco and excessive alcohol use. Osteoporosis develops when bone removal occurs too quickly, replacement occurs too slowly, or both. You are more likely to develop osteoporosis if you did not reach your maximum peak bone mass during your bone-building years.
Bone mass in older adults equals the peak bone mass achieved by age 18–25 minus the amount of bone subsequently lost. Peak bone mass is determined largely by genetic factors, with contributions from nutrition, endocrine status, physical activity, and health during growth 7. Blacks reach higher peak bone mass than whites and Asians, whereas Hispanics have intermediate values. Men have higher bone mass than women. After achieving peak, bone mass plateaus for about 10 yr, during which time bone formation approximately equals bone resorption. After this, bone loss occurs at a rate of about 0.3 to 0.5%/yr. Beginning with menopause, bone loss accelerates in women to about 3 to 5%/yr for about 5 to 7 yr and then the rate of loss decelerates 4.
Women are more likely than men to develop osteoporosis. This is because women generally have smaller, thinner bones than men have and because women can lose bone tissue rapidly in the first 4 to 8 years after menopause because of the sharp decline in production of the hormone estrogen. Produced by the ovaries, estrogen has been shown to have a protective effect on bone. Women usually go through menopause between age 45 and 55. After menopause, bone loss in women greatly exceeds that in men. However, by age 65, women and men tend to lose bone tissue at the same rate. Although men do not undergo the equivalent of menopause, production of the male hormone testosterone may decrease, and this can lead to increased bone loss and a greater risk of developing osteoporosis.
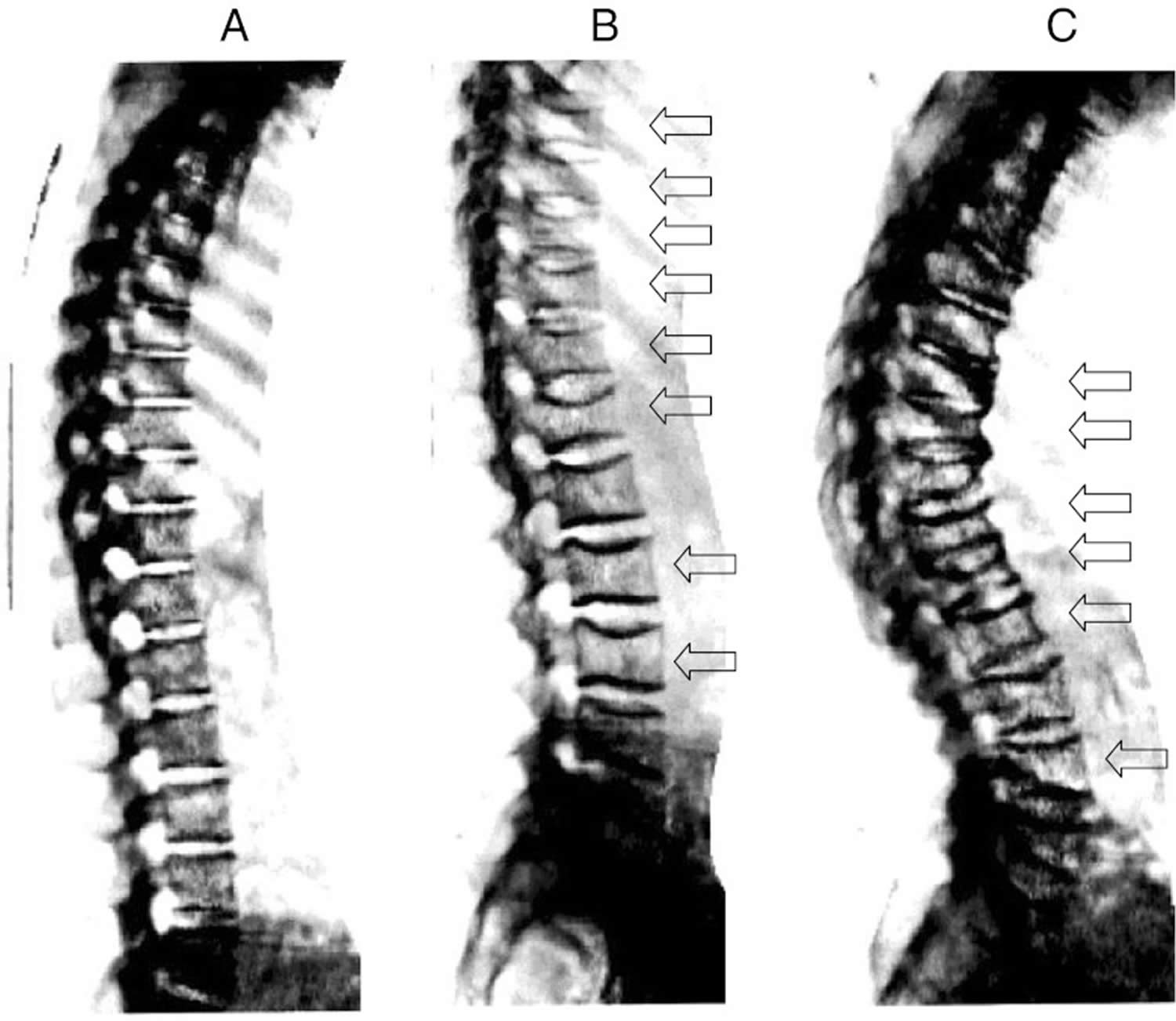
Osteoporotic bone loss affects cortical and trabecular (cancellous) bone. Cortical thickness and the number and size of trabeculae decrease, resulting in increased porosity. Trabeculae may be disrupted or entirely absent. Trabecular bone loss occurs more rapidly than cortical bone loss because trabecular bone is more porous and bone turnover is higher. However, loss of both types contributes to skeletal fragility 4.
The process of bone remodeling that maintains a healthy skeleton may be considered a preventive maintenance program, continually removing older bone and replacing it with new bone. Bone loss occurs when this balance is altered, resulting in greater bone removal than replacement. The imbalance occurs with menopause and advancing age. With the onset of menopause, the rate of bone remodeling increases, magnifying the impact of the remodeling imbalance. The loss of bone tissue leads to disordered skeletal architecture and an increase in fracture risk 8.
The U.S. Preventive Services Task Force, an independent panel of experts in primary care and prevention, recommends that all women age 65 and older be screened for osteoporosis. The task force also recommends screening for women under the age of 65 who are at high risk for fractures. Men over the age 65 who are at high risk for fractures should talk to their doctor about screening. If you are over 50 and have broken a bone, you may have osteoporosis or be at increased risk for the disease. You should also ask your doctor about osteoporosis if you notice that you have lost height or your posture has become stooped or hunched, or if you experience sudden back pain. You may also want to be evaluated for osteoporosis and fracture risk if you have a chronic disease or eating disorder known to increase the risk of osteoporosis, are taking one or more medications known to cause bone loss, or have multiple risk factors for osteoporosis and osteoporosis-related fractures 9.
Having weak bones that easily break is a sign of osteoporosis. It is normal for your bones to become less dense as you grow older, but osteoporosis speeds up this process. This condition can particularly lead to problems in older age because broken bones do not heal as easily in older people as they do in young people, and the consequences are more serious. In general, osteoporosis is more common in women, and they often develop it at a younger age.
Osteoporosis does not affect everyone to the same degree. Women, especially older women, are much more likely to get the disease than are men. In fact, women over age 50 accounted for over 75 percent (7.8 million) of the total cases of osteoporosis at the hip in 2002 10. Women are more susceptible than men to osteoporosis because they begin with less bone mass and lose it at a somewhat faster rate.
Treatment of Osteoporosis = Prevention of Fractures
Individuals with osteoporosis are at high risk of suffering one or more fractures, injuries that can often be physically debilitating and potentially lead to a downward spiral in physical and mental health 11. Generalized osteoporosis is the most common form of the disease, affecting most of the skeleton. Osteoporosis can also occur in localized parts of the skeleton as a result of injury or conditions that reduce muscle forces on the bone, such as limb paralysis. There are a variety of different types of osteoporosis. The most common form of osteoporosis is known as “primary osteoporosis”—that is, osteoporosis that is not caused by some other specific disorder. Bone loss caused by specific diseases or medications (see below) is referred to as “secondary osteoporosis.”
Osteoporosis affects all bones in the body. However, breaks are most common in the hip, wrist, and spine, also called vertebrae . Vertebrae support your body, helping you to stand and sit up. Osteoporosis in the vertebrae can cause serious problems for women. A fracture in this area occurs from day-to-day activities like climbing stairs, lifting objects, or bending forward. Signs of osteoporosis 12:
- Sloping shoulders
- Curve in the back
- Height loss
- Back pain
- Hunched posture
- Protruding abdomen
Getting older does not mean that you will automatically develop osteoporosis, but the risk does increase with age. People over the age of 70 are more likely to have low bone density. Plus, the risk of falling increases in old age, which then also makes fractures more likely.
But there are several things you can do to protect and strengthen your bones — even if you are already older.
- For access to the free Fracture Risk Assessment Tool (FRAX tool) go here (https://frax.shef.ac.uk/FRAX/tool.aspx?country=9)
What is Osteopenia vs Osteoporosis
Differentiating Osteopenia, Osteoporosis and Osteomalacia
Two metabolic bone diseases decrease bone mass: osteoporosis and osteomalacia.
- In osteoporosis, bone mass decreases, but the ratio of bone mineral to bone matrix is normal.
- In osteomalacia, the ratio of bone mineral to bone matrix is low.
Osteoporosis results from a combination of low peak bone mass, increased bone resorption, and impaired bone formation. Osteomalacia is due to impaired mineralization, usually because of severe vitamin D deficiency or abnormal vitamin D metabolism (see Vitamin D). Osteomalacia can be caused by disorders that interfere with vitamin D absorption (eg, celiac disease) and by certain drugs (eg, phenytoin, phenobarbital). Osteoporosis is much more common than osteomalacia in the US. The two disorders may coexist, and their clinical expression is similar; moreover, mild to moderate vitamin D deficiency can occur in osteoporosis 4.
Osteomalacia should be suspected if the vitamin D level is consistently very low. To definitively differentiate between the two disorders, clinicians can do a tetracycline-labeled bone biopsy 4.
There are many causes for osteopenia including calcium and vitamin D deficiency and inactivity. Osteopenia frequently develops in people taking antiretroviral drugs for HIV; however, the association between antiretroviral drugs drugs and osteopenia is unclear 15. Genetics plays an important role in a person’s bone mineral density and often Caucasian women with a thin body habitus who are premenopausal are found to have osteopenia. Correction of calcium and vitamin D deficiency and walking 3 to 5 miles a week can often improve bone density in the hip and spine. There are a variety of pharmaceutical agents that have been recommended for the treatment of osteopenia and osteoporosis including hormone replacement therapy, selective estrogen receptor modulator therapy, anti-resorptive therapy. In addition patients with osteoporosis who have failed anti-resorptive therapy can have a significant improvement in their bone density with anabolic therapy 13.
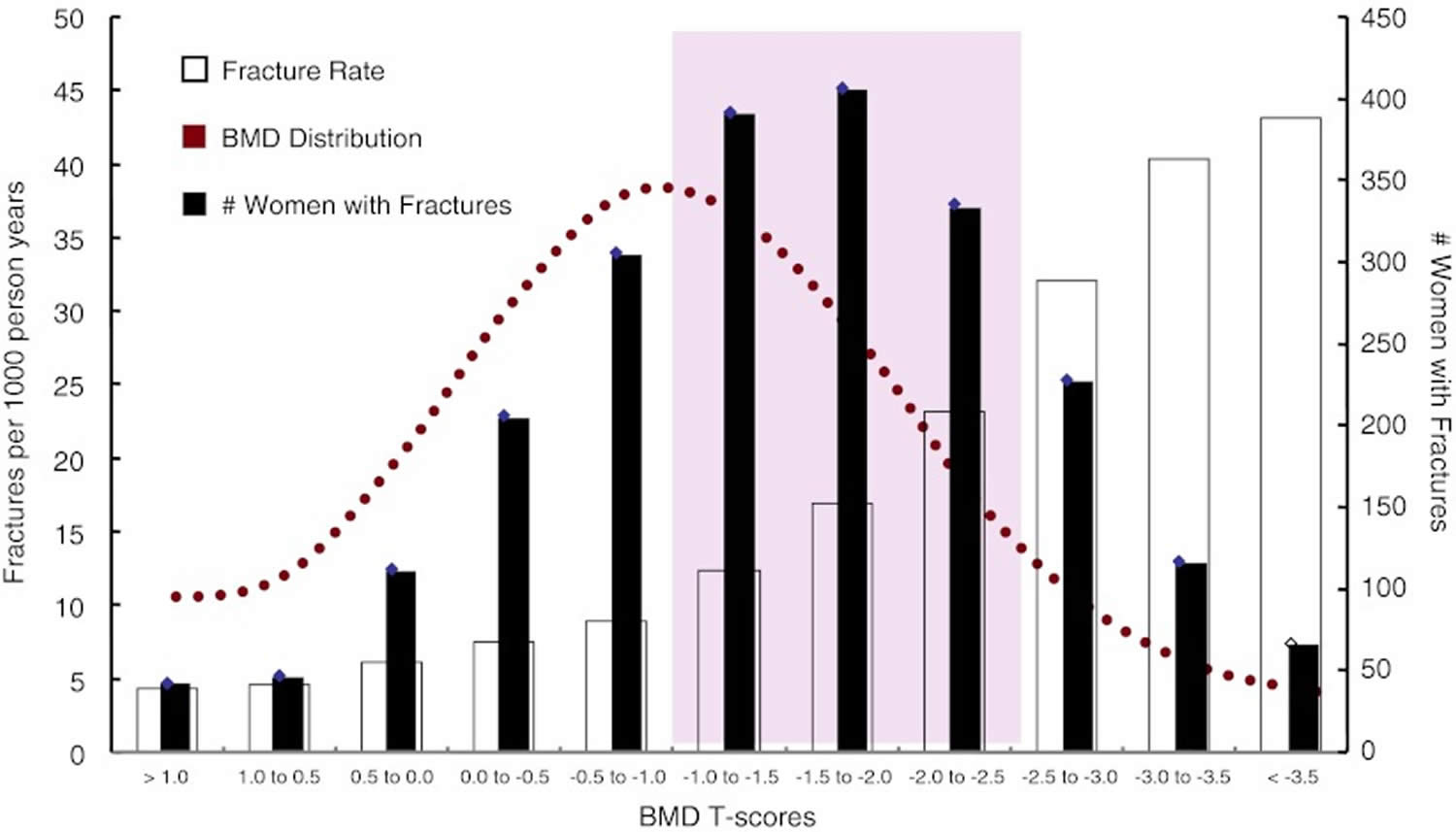
While pharmacological treatment of patients with prevalent osteoporotic fractures is universally accepted, the treatment of patients at increased risk of fracture due to low bone mass is more controversial. Our ability to detect patients at increased risk has improved significantly after the widespread availability of Dual Energy X-ray Absorptiometry (DXA), which provides a precise assessment of the amount of mineralized bone in the skeleton. According to the WHO criteria for assessment of DXA measurements, patients are considered having low bone mass (osteopenic), when their bone mineral density (BMD) t-score of the spine or hip lies between −1 and −2,5. Although fracture risk increases with decreases in bone mineral density, the vast majority of osteoporotic fractures occur in osteopenic patients. This is due to the fact that even though the risk of fracture is lower in the osteopenia than in osteoporosis, the number of subjects at risk is much higher in the osteopenic range due to the Gaussian distribution of bone mineral density values in the population (see below Fig. 1). In an analysis of self reported fractures from the National Osteoporosis Risk Assessment study Siris et al. 16 reported that 82% of postmenopausal women with fractures had T scores better than −2.5. The study comprised 149,524 white postmenopausal women aged 50 to 104 years (mean age, 64.5 years). New fractures were reported by 2,259 women, including 393 hip fractures; but only 6.4% exhibited baseline T scores of −2.5 or less. Although fracture rates were highest in women with a t-score <−2,5, only 18% of the osteoporotic fractures and 26% of hip fractures occurred in this group 16.
Figure 1. Bone fracture rates according to bone mineral density (BMD)
Footnotes: Distribution of fracture rates and number of women with fractures according to bone mineral density (BMD) T-scores from the The National Osteoporosis Risk Assessment (NORA) study, which comprised 149,524 white postmenopausal women aged 50 to 104 years (mean age, 64.5 years). Bone mineral density (BMD) was assessed by peripheral bone densitometry at the heel, finger, or forearm. Although fracture rates were highest in women with the lowest t-scores (open bars), the largest absolute number of fractures (black bars) was seen in the osteopenic range of T-score (−1 to −2,5).
[Source 16 ]Identification of osteopenic patients at increased risk of fracture
Bone mineral density is related to bone strength and low bone mineral density is a major risk factor for fractures. However, most patients presenting with a fracture do not have bone mineral density based osteoporosis, defined according to the World Health Organization (WHO) definition as a T score of −2.5 or below. The most poignant example is hip fracture, where only half the patients exhibit t-scores below −2.5 17. In addition, and independent of bone-related risks, extraskeletal risk factors such as falls contribute to fracture risk and are present in the majority of patients older than 50 years presenting with a clinical fracture, and falls are the dominant event leading to forearm and hip fracture 18.
Summary: An ever increasing array of effective treatments is at our disposal, to protect patients with osteopenia against fractures. While there is general consensus on treating osteopenic individuals with prevalent low energy fractures, the treatment of osteopenia without fracture is still debatable 19. However, current evidence indicates that specific drug therapy should be instituted if an osteopenic patients has prevalent fractures or suffers new fractures, be it clinical or asymptomatic. Moreover, a significant accumulation of several significant risk factors, for example as indicated by the Fracture Risk Assessment Tool (FRAX tool) may constitute an indication for medical treatment by means of drugs. Patients without such risk factors should be counselled on a “bone friendly” lifestyle with nutritional modifications, regular exercise, moderation in alcohol use and If possible smoking cessation. In patients with low vitamin D levels, Calcium plus vitamin D supplementation may also be indicated 19.
- For access to the free Fracture Risk Assessment Tool (FRAX tool) go here (https://frax.shef.ac.uk/FRAX/tool.aspx?country=9)
How common is osteoporosis?
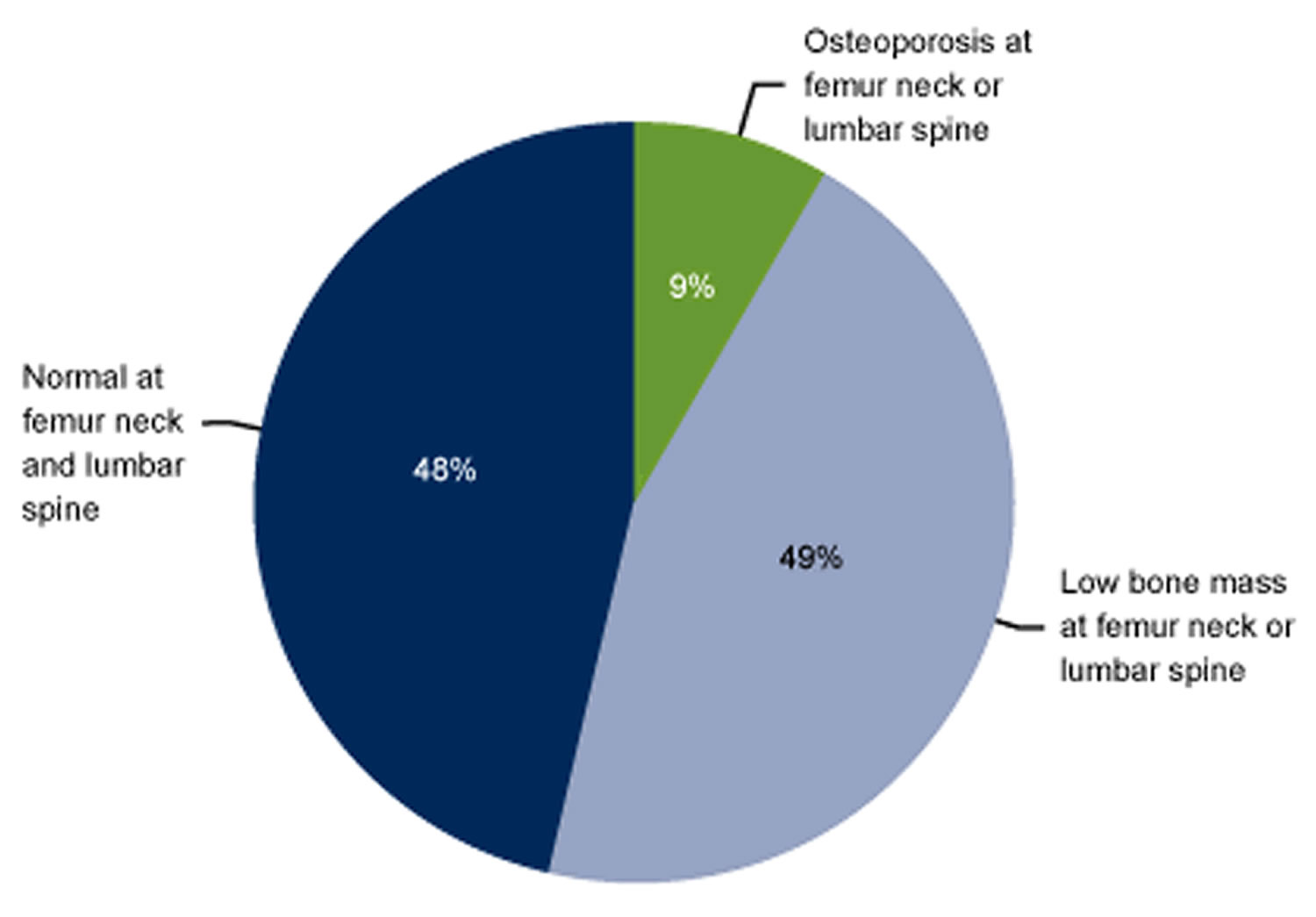
In the US, data from the National Health and Nutrition Examination Survey, 2005–2008, 4 percent of men 50 years of age and over have osteoporosis of the femur neck or lumbar spine and 16 percent of women 50 years of age and over with osteoporosis of the femur neck or lumbar spine 20.
- 9% of adults aged 50 years and over had osteoporosis, as defined by the World Health Organization, at either the femur neck or lumbar spine. About one-half had low bone mass at either site, while 48% had normal bone mass at both sites.
- Estimates of poor skeletal status at the femur neck or lumbar spine when considered alone were not the same as estimates based on the two skeletal sites together because some individuals had the condition at one site but not the other.
- The prevalence of osteoporosis or low bone mass at either the femur neck or lumbar spine differed by age, sex, and race and ethnicity. The prevalence was higher in women and increased with age. Differences between racial and ethnic groups varied by sex and skeletal status category.
This data brief presents the most recent national data on osteoporosis or low bone mass at either the femur neck or lumbar spine among older adults in the United States population based on these WHO categories. Results are presented by age, sex, and race and ethnicity.
Footnote: The percentages shown will not add up to 100% due to double counting among those with osteoporosis at either skeletal site or low bone mass at either skeletal site.
[Source 21 ]The prevalence of osteoporosis or low bone mass at either the femur neck or lumbar spine is higher in women than men in each decade or when compared overall for aged 50 years and over after adjusting for age differences between the two sexes. The age-adjusted prevalence of osteoporosis at either skeletal site was 16% in women compared with 4% in men. The age-adjusted prevalence of low bone mass at either skeletal site was 61% in women compared with 38% in men.
The prevalence of osteoporosis or low bone mass at either skeletal site differ by race and ethnicity in men after adjusting for age differences between the racial and ethnic groups. The age-adjusted prevalence of osteoporosis at either skeletal site in men of other races (9%) was higher than the prevalence in non-Hispanic white men (4%). The age-adjusted prevalence of low bone mass at either skeletal site was lower in non-Hispanic black men (24%) compared with non-Hispanic white men (39%).
The prevalence of osteoporosis or low bone mass at either the femur neck or lumbar spine differ by race and ethnicity in women after adjusting for age differences between the racial and ethnic groups. When compared with the age-adjusted prevalence of osteoporosis in non-Hispanic white women (15%), the age-adjusted prevalence of osteoporosis at either skeletal site is higher in Mexican-American women (26%) and lower in non-Hispanic black women (9%). When compared with the age-adjusted prevalence in non-Hispanic white women (62%), the age-adjusted prevalence of low bone mass at either skeletal site is higher in women of other races (72%) and lower in non-Hispanic black women (44%).
According to the Robert Koch Institute, 8% of men and 13% of women in Germany between the ages of 60 and 69 report being diagnosed with osteoporosis. But it is not known exactly how many people in Germany actually have osteoporosis or how many bone fractures are caused by osteoporosis. Also, not everyone with osteoporosis ends up with a bone fracture 3.
Hip fractures in particular can have serious consequences. This is a problem that almost only affects older people: In Germany, 6 to 7 out of 1,000 people over the age of 65 break their hip bone (femoral neck) every year. Most of them are over the age of 75.
- For access to the free Fracture Risk Assessment Tool (FRAX tool) go here (https://frax.shef.ac.uk/FRAX/tool.aspx?country=9)
Causes of Osteoporosis
Inside bones there is a supporting structure with interconnecting bony plates and rods called trabeculae. This structure is called trabecular or spongy bone because it looks a bit like a sponge or honeycomb. Osteoporosis develops when a large amount of the spongy bone tissue breaks down, leaving bigger spaces. The bone becomes more porous as a result. This affects the fine structure of the bones, and they become brittle. Some people’s bones become so fragile that even tripping over something or lifting a heavy shopping bag is enough to cause vertebrae to break. Osteoporosis makes your bones brittle and breakable.
When you’re young, your bones are dense and strong. Bone density starts to gradually decrease once you turn 30, even if you do not have osteoporosis. Around the age of 50 this process speeds up, especially in women. Before menopause, the female sex hormone estrogen helps protect the bones by slowing down bone loss. So after menopause, when this hormone level drops, bone tissue is lost more quickly.
Osteoporosis can develop as a primary disorder or secondarily due to some other factor. The sites of fracture are similar in primary osteoporosis and secondary osteoporosis.
If no cause for the bone loss can be found, it is called primary osteoporosis. Secondary osteoporosis is when bones have become fragile due to something else, like another condition or long-term corticosteroid use.
Some people have both primary osteoporosis and secondary osteoporosis. Talk to your family doctor about your risk factors.
Primary osteoporosis
More than 95% of osteoporosis in women and about 80% in men is primary osteoporosis. Most cases occur in postmenopausal women and older men. Gonadal insufficiency is an important factor in both men and women. Other factors that may accelerate bone loss in patients with primary osteoporosis include decreased calcium intake, low vitamin D levels, certain drugs, and hyperparathyroidism. Some patients have an inadequate intake of calcium during the bone growth years of adolescence and thus never achieve peak bone mass 4.
Primary osteoporosis risk factors:
- Sex: Osteoporosis is more common in women than men.
- Age: The older you are, the greater your chance of having osteoporosis.
- Race: Caucasians and Asians are more likely to have osteoporosis.
- Genetics: Your risk of osteoporosis is higher if it runs in your family.
- Menopause: This period in a woman’s life causes physical and hormonal effects. For example, it lowers your estrogen. These changes can increase your risk of osteoporosis. Your risk is even higher if you have early menopause (before age 45).
- Body frame: People who have small, thin frames are more likely to develop osteoporosis.
- Health: Certain conditions, such as cancer or stroke, can lead to osteoporosis.
The major mechanism of bone loss is increased bone resorption, resulting in decreased bone mass and microarchitectural deterioration, but sometimes bone formation is impaired. The mechanisms of bone loss may involve the following:
- Local changes in the production of bone-resorbing cytokines, such as increases in cytokines that stimulate bone resorption
- Impaired formation response during bone remodeling (probably caused by age-related decline in the number and activity of osteoblasts)
- Other factors such as a decline in local and systemic growth factors
Fragility fractures rarely occur in children, adolescents, premenopausal women, or men < 50 yr with normal gonadal function and no detectable secondary cause, even in those with low bone mass (low Z-scores on dual-energy x-ray absorptiometry [DEXA]). Such uncommon cases are considered idiopathic osteoporosis.
Secondary osteoporosis
Secondary osteoporosis accounts for < 5% of osteoporosis in women and about 20% in men. The causes (see Causes of Secondary Osteoporosis) may also further accelerate bone loss and increase fracture risk in patients with primary osteoporosis 4.
Patients with chronic kidney disease may have several reasons for low bone mass, including secondary hyperparathyroidism, elevated serum phosphate, calcitriol deficiency, abnormalities of serum calcium and vitamin D, osteomalacia, and low-turnover bone disorders (adynamic bone disease).
Causes of Secondary Osteoporosis
- Alcohol abuse
- Cancer (eg, multiple myeloma)
- Chronic obstructive pulmonary disease (COPD) (due to the disorder itself, as well as tobacco use and/or treatment with glucocorticoids). Chronic obstructive pulmonary disease is airflow limitation caused by an inflammatory response to inhaled toxins, often cigarette smoke. Alpha-1 antitrypsin deficiency and various occupational exposures are less common causes in nonsmokers.
- Chronic kidney disease
- Drugs (eg, glucocorticoids, anticonvulsants, medroxyprogesterone, aromatase inhibitors, rosiglitazone, pioglitazone, thyroid replacement therapy, heparin, ethanol, tobacco)
- Endocrine disease or hormonal imbalances (eg, glucocorticoid excess, hyperparathyroidism, hyperthyroidism, hypogonadism, hyperprolactinemia, diabetes mellitus)
- Eating disorders, such as anorexia nervosa
- Hypercalciuria
- Hypervitaminosis A
- Hypophosphatasia
- Hypovitaminosis D
- Inactive lifestyle or lack of exercise
- Lack of calcium and/or vitamins
- Liver disease
- Long-term use of certain medicines. Examples include corticosteroids and proton pump inhibitors (PPIs). Corticosteroids treat inflammation, pain, and chronic conditions, such as asthma and rheumatoid arthritis. Proton pump inhibitors (PPIs) help reduce stomach acid. These medicines can make it hard for your body to absorb calcium and cause osteoporosis.
- Malabsorption syndromes
- Prolonged weightlessness (as occurs in space flight)
- Rheumatoid arthritis
- Smoking or tobacco use.
Risk factors for osteoporosis
There are a number of factors that can increase someone’s risk of developing osteoporosis. Some can be influenced, whereas others cannot. The main risk factors for osteoporosis include:
Factors that you can’t control:
- Being female. Women develop osteoporosis more often than men, and they are also more likely to have bone fractures.
- Getting older. As we get older, our bone density decreases and the risk of developing osteoporosis increases. Men over the age of 65 and post-menopausal women are at the greatest risk.
- Sex hormone deficiencies. The most common manifestation of estrogen deficiency in premenopausal women is amenorrhea, the abnormal absence of menstrual periods. Missed or irregular periods can be caused by various factors, including hormonal disorders as well as extreme levels of physical activity combined with restricted calorie intake—for example, in female marathon runners, ballet dancers, and women who spend a great deal of time and energy working out at the gym. Low estrogen levels in women after menopause and low testosterone levels in men also increase the risk of osteoporosis. Lower than normal estrogen levels in men may also play a role. Low testosterone and estrogen levels are often a cause of osteoporosis in men being treated with certain medications for prostate cancer.
- Having a small, thin body (under 127 pounds)
- Having a family history of osteoporosis. Women whose mother or father broke their hip because of osteoporosis are at greater risk of developing osteoporosis themselves.
- Being white or Asian, but African American women and Latinas are also at risk
- Not getting your period (if you should be getting it)
- Having a disorder that increases your risk of getting osteoporosis, (such as rheumatoid arthritis, type 1 diabetes, premature menopause, anorexia nervosa)
- Not getting enough exercise or sedentary lifestyle
- Long-term use of certain medicines, including:
- Glucocorticoids — medicines used to treat many illnesses, including arthritis, asthma, and lupus
- Some antiseizure medicines
- Gonadotropin-releasing hormone — used to treat endometriosis
- Antacids with aluminum — the aluminum blocks calcium absorption
- Some cancer treatments
- Too much replacement thyroid hormone
Factors that you can control:
- Smoking
- Drinking too much alcohol. Experts recommend no more than 1 drink a day for women.
- A diet low in dairy products or other sources of calcium and vitamin D
- Not getting enough exercise
- Low body weight (compared to body size). Anorexia nervosa, for example, is an eating disorder that leads to abnormally low body weight, malnutrition, amenorrhea, and other effects on the body that adversely affect bone health. Late onset of puberty and early menopause reduce lifetime estrogen exposure in women and also increase the risk of osteoporosis.
- Diet low in calcium
- Vitamin D deficiency
- Long-term steroid use
- Use of other medications, such as some antidepressants (SSRIs), diabetes medicines (glitazones), glucocorticoids and some anticonvulsants lead to bone loss and increased risk of osteoporosis. Other drugs that may lead to bone loss include anticlotting drugs, such as heparin; drugs that suppress the immune system, such as cyclosporine; and drugs used to treat prostate cancer.
Osteoporosis prevention
You cannot always avoid osteoporosis. However, there are some changes you can make to prevent or reduce your risk. The best way to prevent weak bones is to work on building strong ones. No matter how old you are, it is never too late to start. Building strong bones during childhood and the teen years is one of the best ways to keep from getting osteoporosis later. As you get older, your bones don’t make new bone fast enough to keep up with the bone loss. And after menopause, bone loss happens more quickly. But there are things you can do to slow the natural bone loss with aging and to prevent your bones from becoming weak and brittle. These include getting regular exercise, quitting smoking and getting enough calcium and vitamin D in your diet. They help keep your bones healthy as you age. Dietary supplements can be used as an additional source of calcium and vitamin D if you are not getting enough in your diet.
The National Academy of Medicine recommends 600 IU daily of vitamin D from food in patients up to 70 years of age and 800 IU of vitamin D in those older than 70 years. For calcium, they recommend 1,000 mg daily for adults up to 50 years of age, increasing to 1,200 mg daily for those older than 50 years. However, because supplements do not reduce fractures, the U.S. Preventive Services Task Force (USPSTF) recommends against supplementing with 1,000 mg calcium and 400 IU vitamin D in postmenopausal women. The evidence is insufficient for larger doses and supplementation in premenopausal women.
- Calcium. Women 50 years of age and younger and men 70 years of age and younger should get 1,000 mg of calcium per day. Women older than 50 years of age and men older than 70 years of age should get 1,200 mg of calcium per day. Women who are post-menopausal may need 1,500 mg of calcium per day. It is best to get your calcium from food. Nonfat and low-fat dairy products are good sources of calcium. Other options include dried beans, salmon, spinach, and broccoli. If you don’t get enough calcium from the food you eat, your doctor may suggest taking a calcium supplement.
- Vitamin D. Most people need about 800 International Units (IU) of vitamin D each day. It helps your body absorb calcium. You can get vitamin D from sunlight, food, and supplements. Your skin makes vitamin D when it is exposed to sunlight. However, you should be careful of sun exposure. Too much can cause skin cancer. Your doctor can test your blood to measure your vitamin D level. If your vitamin D level is low, your doctor may suggest taking a supplement.
Lifestyle Approaches to Promote Bone Health
There is much that individuals can do to promote their own bone health throughout life. This section outlines recommendations for diet, physical activity, and other lifestyle practices that can help to achieve that goal. Moreover, the activities and practices suggested in this section contribute not only to bone health, but to overall health and vitality. In fact, bone-specific recommendations fit well within an overall program of good nutrition and physical activity that should be followed in order to prevent the onset of many of the major chronic diseases affecting Americans.
Calcium
Ninety-nine percent of the calcium in the human body is stored in the bones and teeth. Calcium is a mineral that the body needs for numerous functions, including building and maintaining bones and teeth, blood clotting, the transmission of nerve impulses, and the regulation of the heart’s rhythm 22. Calcium is required for vascular contraction and vasodilation, muscle function, nerve transmission, intracellular signaling and hormonal secretion, though less than 1% of total body calcium is needed to support these critical metabolic functions 23. Serum calcium is very tightly regulated and does not fluctuate with changes in dietary intakes; the body uses bone tissue as a reservoir for, and source of calcium, to maintain constant concentrations of calcium in blood, muscle, and intercellular fluids 23.
The body gets the calcium it needs in two ways. One is by eating foods or supplements that contain calcium. Good sources include dairy products, which have the highest concentration per serving of highly absorbable calcium, and dark leafy greens or dried beans, which have varying amounts of absorbable calcium. Calcium supplements often contain vitamin D; taking calcium paired with vitamin D seems to be more beneficial for bone health than taking calcium alone 22.
The other way the body gets calcium is by pulling it from bones. This happens when blood levels of calcium drop too low, usually when it’s been awhile since having eaten a meal containing calcium. Ideally, the calcium that is “borrowed” from the bones will be replaced at a later point. But, this doesn’t always happen. Most important, this payback can’t be accomplished simply by eating more calcium 22.
Not all calcium consumed is actually absorbed in the gut. Humans absorb about 30% of the calcium in foods, but this varies depending upon the type of food consumed 23. Other factors also affect calcium absorption including the following:
- Amount consumed: the efficiency of absorption decreases as calcium intake increases 23.
- Age and life stage: net calcium absorption is as high as 60% in infants and young children, who need substantial amounts of the mineral to build bone 24. Absorption decreases to 15%–20% in adulthood (though it is increased during pregnancy) and continues to decrease as people age; compared with younger adults, recommended calcium intakes are higher for females older than 50 years and for both males and females older than 70 years 25.
- Vitamin D intake: this nutrient, obtained from food and produced by skin when exposed to sunlight of sufficient intensity, improves calcium absorption 23.
- Other components in food: phytic acid and oxalic acid, found naturally in some plants, bind to calcium and can inhibit its absorption. Foods with high levels of oxalic acid include spinach, collard greens, sweet potatoes, rhubarb, and beans. Among the foods high in phytic acid are fiber-containing whole-grain products and wheat bran, beans, seeds, nuts, and soy isolates 23. The extent to which these compounds affect calcium absorption varies. Research shows, for example, that eating spinach and milk at the same time reduces absorption of the calcium in milk 26. In contrast, wheat products (with the exception of wheat bran) do not appear to lower calcium absorption 27. For people who eat a variety of foods, these interactions probably have little or no nutritional consequence and, furthermore, are accounted for in the overall calcium DRIs, which factor in differences in absorption of calcium in mixed diets.
Some absorbed calcium is eliminated from the body in urine, feces, and sweat. This amount is affected by such factors as the following:
- Sodium (salt) and protein intakes: high sodium intake increases urinary calcium excretion 28. High protein intake also increases calcium excretion and was therefore thought to negatively affect calcium status 28. However, more recent research suggests that high protein intake also increases intestinal calcium absorption, effectively offsetting its effect on calcium excretion, so whole body calcium retention remains unchanged 29.
- Caffeine intake: this stimulant in coffee and tea can modestly increase calcium excretion and reduce absorption 30. One cup of regular brewed coffee, for example, causes a loss of only 2–3 mg of calcium 28. Moderate caffeine consumption (1 cup of coffee or 2 cups of tea per day) in young women has no negative effects on bone 31.
- Alcohol intake: alcohol intake can affect calcium status by reducing its absorption 32 and by inhibiting enzymes in the liver that help convert vitamin D to its active form 33. However, the amount of alcohol required to affect calcium status and whether moderate alcohol consumption is helpful or harmful to bone is unknown.
- Phosphorus intake: the effect of this mineral on calcium excretion is minimal. Several observational studies suggest that consumption of carbonated soft drinks with high levels of phosphate is associated with reduced bone mass and increased fracture risk. However, the effect is probably due to replacing milk with soda rather than the phosphorus itself 34.
- Fruit and vegetable intakes: metabolic acids produced by diets high in protein and cereal grains increase calcium excretion 35. Fruits and vegetables, when metabolized, shift the acid/base balance of the body towards the alkaline by producing bicarbonate, which reduces calcium excretion. However, it is unclear if consuming more fruits and vegetables affects bone mineral density. These foods, in addition to reducing calcium excretion, could possibly reduce calcium absorption from the gut and therefore have no net effect on calcium balance.
It is important to get plenty of calcium in the foods you eat. Foods rich in calcium include:
- Dairy products such as milk, cheese, and yogurt
- Leafy, green vegetables
- Fish with soft bones that you eat, such as canned sardines and salmon
- Calcium-enriched foods such as breakfast cereals, fruit juices, soy and rice drinks, and tofu. Check the product labels.
The exact amount of calcium you need depends on your age and other factors. Growing children and teenagers need more calcium than young adults. Older women need plenty of calcium to prevent osteoporosis. People who do not eat enough high-calcium foods should take a calcium supplement.
Lifelong adequate calcium intake is necessary for the acquisition of peak bone mass and subsequent maintenance of bone health. The skeleton contains 99 % of the body’s calcium stores; when the exogenous supply is inadequate, bone tissue is resorbed from the skeleton to maintain serum calcium at a constant level.
Americans obtain most of their calcium from dairy products. Most Americans above age 9 on average do not consume recommended levels of calcium 36. In fact, approximately three 8-ounce glasses of milk each day, combined with the calcium from the rest of a normal diet, is enough to meet the recommended daily requirements for most adults.
For postmenopausal women, the recommended total daily calcium intake is 1,200 mg per day in two or more doses. These levels of intake can be achieved through dietary sources of calcium, including both dairy and non-dairy products. In addition, calcium supplements (e.g., calcium carbonate, calcium citrate, other calcium salts) are available in the form of pills, chewable tablets, and liquids 37.
Here’s how much calcium you need each day 38:
Table 1. Daily calcium requirements
| Life Stage | Recommended Amount |
|---|---|
| Birth to 6 months | 200 mg |
| Infants 7–12 months | 260 mg |
| Children 1–3 years | 700 mg |
| Children 4–8 years | 1,000 mg |
| Children 9–13 years | 1,300 mg |
| Teens 14–18 years | 1,300 mg |
| Adults 19–50 years | 1,000 mg |
| Adult men 51–70 years | 1,000 mg |
| Adult women 51–70 years | 1,200 mg |
| Adults 71 years and older | 1,200 mg |
| Pregnant and breastfeeding teens | 1,300 mg |
| Pregnant and breastfeeding adults | 1,000 mg |
Pregnant or nursing women need the same amount of calcium as other women of the same age.
There is no evidence that calcium intake in excess of these amounts confers additional bone strength. Some research suggests that high calcium intakes might increase the risk of heart disease and prostate cancer. The Tolerable Upper Intake Levels (ULs) for calcium established by the Food and Nutrition Board are listed in Table 2. They are based on observational evidence from the Women’s Health Initiative (WHI) showing a link between higher intakes of supplemental calcium (1,000 mg/day for 7 years) and a greater risk of kidney stones 40, 41. However, two subsequent systematic reviews of the evidence from 10 studies in more than 8,000 adults with osteoporosis who took 120 to 1,500 mg supplemental calcium daily for 3 days to 3 years 42 and 11 randomized controlled trial in 51,419 adults 50 years and older who took 1,000 to 1,600 mg calcium with or without vitamin D for 2 to 7 years 43 found no such association.
High levels of calcium in the blood and urine can cause poor muscle tone, poor kidney function, low phosphate levels, constipation, nausea, weight loss, extreme tiredness, frequent need to urinate, abnormal heart rhythms, and a high risk of death from heart disease. However, high levels of calcium in the blood and urine are usually caused by a health condition such as high levels of parathyroid hormone or cancer, not by high calcium intakes 44.
The daily upper limits for calcium include intakes from all sources—food, beverages, and supplements—and are listed below.
Table 2. Tolerable Upper Intake Levels (ULs) for Calcium
| Life Stage | Upper Limit |
|---|---|
| Birth to 6 months | 1,000 mg |
| Infants 7–12 months | 1,500 mg |
| Children 1–8 years | 2,500 mg |
| Children 9–18 years | 3,000 mg |
| Adults 19–50 years | 2,500 mg |
| Adults 51 years and older | 2,000 mg |
| Pregnant and breastfeeding teens | 3,000 mg |
| Pregnant and breastfeeding adults | 2,500 mg |
Calcium Rich Foods
Calcium is found in many foods. You can get recommended amounts of calcium by eating a variety of foods, including the following:
- Milk, yogurt, and cheese are the main food sources of calcium for most people in the United States.
- Canned sardines and salmon with bones contain calcium.
- Certain vegetables, such as kale, broccoli, and Chinese cabbage (bok choi) also contain calcium.
- Calcium is added to some beverages, including many fruit juices and milk substitutes such as soy and almond beverages, as well as some brands of tofu and ready-to-eat cereals. To find out whether these foods have calcium added, check the product labels.
- Most grains (such as breads, pastas, and unfortified cereals) do not have high amounts of calcium. However, because people eat them often, what they contribute adds up.
The U.S. Department of Agriculture’s (USDA’s) Nutrient Database website lists the nutrient content of many foods with calcium arranged by nutrient content 45 and by food name 46.
Table 3. Calcium content of selected foods
| Food* | Milligrams (mg) per serving | Percent DV* |
|---|---|---|
| Yogurt, plain, low fat, 8 ounces | 415 | 32 |
| Orange juice, calcium fortified, 1 cup | 349 | 27 |
| Yogurt, fruit, low fat, 8 ounces | 344 | 27 |
| Mozzarella, part skim, 1.5 ounces | 333 | 26 |
| Sardines, canned in oil, with bones, 3 ounces | 325 | 25 |
| Milk, nonfat, 1 cup** | 299 | 23 |
| Soymilk, calcium fortified, 1 cup | 299 | 23 |
| Milk, whole (3.25% milk fat), 1 cup** | 276 | 21 |
| Tofu, firm, made with calcium sulfate, ½ cup*** | 253 | 19 |
| Salmon, pink, canned, solids with bones, 3 ounces | 181 | 14 |
| Cottage cheese, 1% milk fat, 1 cup | 138 | 11 |
| Tofu, soft, made with calcium sulfate, ½ cup*** | 138 | 11 |
| Soybeans, cooked, ½ cup | 131 | 10 |
| Breakfast cereals, fortified with 10% of the DV for calcium, 1 serving | 130 | 10 |
| Spinach, boiled, drained, ½ cup | 123 | 9 |
| Frozen yogurt, vanilla, soft serve, ½ cup | 103 | 8 |
| Turnip greens, fresh, boiled, ½ cup | 99 | 8 |
| Kale, fresh, cooked, 1 cup | 94 | 7 |
| Chia seeds, 1 tablespoon | 76 | 6 |
| Chinese cabbage (bok choi), raw, shredded, 1 cup | 74 | 6 |
| Beans, pinto, canned, drained, ½ cup | 54 | 4 |
| Tortilla, corn, one, 6” diameter | 46 | 4 |
| Sour cream, reduced fat, 2 tablespoons | 31 | 2 |
| Bread, whole-wheat, 1 slice | 30 | 2 |
| Kale, raw, chopped, 1 cup | 24 | 2 |
| Broccoli, raw, ½ cup | 21 | 2 |
| Apple, golden delicious, with skin, 1 medium | 10 | 0 |
Footnotes:
* DV = Daily Value. The U.S. Food and Drug Administration (FDA) developed DVs to help consumers compare the nutrient contents of foods and dietary supplements within the context of a total diet. The DV for calcium is 1,300 mg for adults and children age 4 years and older [13]. FDA requires food labels to list calcium content. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
** Calcium content varies slightly by fat content; the more fat in the food, the less calcium it contains.
*** Calcium content is for tofu processed with a calcium salt. Tofu processed with other salts does not provide significant amounts of calcium.
Calcium supplements
The two main forms of calcium in supplements are carbonate and citrate. Calcium carbonate is more commonly available and is both inexpensive and convenient 48. Due to its dependence on stomach acid for absorption, calcium carbonate is absorbed most efficiently when taken with food, whereas calcium citrate is absorbed equally well when taken with or without food 49. Calcium citrate is also useful for people with achlorhydria, inflammatory bowel disease, or absorption disorders 23. Other calcium forms in supplements or fortified foods include gluconate, lactate, and phosphate. Calcium citrate malate is a well-absorbed form of calcium found in some fortified juices 50.
Calcium supplements contain varying amounts of elemental calcium. For example, calcium carbonate is 40% calcium by weight, whereas calcium citrate is 21% calcium. Fortunately, elemental calcium is listed in the Supplement Facts panel, so consumers do not need to calculate the amount of calcium supplied by various forms of calcium supplements.
The percentage of calcium absorbed depends on the total amount of elemental calcium consumed at one time; as the amount increases, the percentage absorption decreases. Absorption is highest in doses ≤500 mg 23. So, for example, one who takes 1,000 mg/day of calcium from supplements might split the dose and take 500 mg at two separate times during the day.
Some individuals who take calcium supplements might experience gastrointestinal side effects including gas, bloating, constipation, or a combination of these symptoms. Calcium carbonate appears to cause more of these side effects than calcium citrate 23, so consideration of the form of calcium supplement is warranted if these side effects are reported. Other strategies to alleviate symptoms include spreading out the calcium dose throughout the day and/or taking the supplement with meals.
Vitamin D
Vitamin D plays a major role in calcium absorption, health of bone, bone mineralization (hardening), muscle performance, balance and risk of falling. Vitamin D is produced in your skin when it is exposed to sunlight. You need 10 to 15 minutes of sunlight to the hands, arms, and face, two to three times a week to make enough vitamin D. The amount of time depends on how sensitive your skin is to light. It also depends on your use of sunscreen, your skin color, and the amount of pollution in the air. You can also get vitamin D by eating foods, such as milk, or by taking vitamin pills. Vitamin D taken in the diet by food or pills is measured in international units (IU). Look at the pill bottle or food label for the IU amount.
The National Osteoporosis Foundation recommends an intake of 800 to 1000 international units (IU) of vitamin D per day for adults age 50 and older. Vitamin D is synthesized in the skin through sunlight exposure, or it may be taken as a supplement. However, the skin of older individuals does not synthesize vitamin D as well as the skin of younger individuals, and in some parts of the country, the winter sun does not produce vitamin D in the skin of all individuals. In addition, vitamin D is not available in many foods other than fortified milk, which contains 100 IU (international units) per cup. Thus, many individuals will need to take a supplement, especially those who avoid sun exposure, use sun block, or do not drink milk. The recommended dose of vitamin D is 200 to 600 IU daily, with the dose dependent on age, as shown in the table below 51. However, many experts are recommending more vitamin D for the frail elderly 52.
Institute of Medicine Dietary Reference Intakes for vitamin D are 600 IU/day until age 70 and 800 IU/day for adults age 71 years and older.
Here’s how much vitamin D you need each day.
Table 4. Recommended Dietary Allowances (RDAs) for Vitamin D
| Life Stage | Recommended Amount |
|---|---|
| Birth to 12 months | 10 mcg (400 IU) |
| Children 1–13 years | 15 mcg (600 IU) |
| Teens 14–18 years | 15 mcg (600 IU) |
| Adults 19–70 years | 15 mcg (600 IU) |
| Adults 71 years and older | 20 mcg (800 IU) |
| Pregnant and breastfeeding teens and women | 15 mcg (600 IU) |
Footnotes: The amount of vitamin D contained in supplements is sometimes expressed in international units (IU) where 40 IU is equal to one microgram (1 mcg) of vitamin D.
The total daily vitamin D intake of persons who are not vitamin D deficient should not exceed 2,000 IU 54. Many calcium supplements contain vitamin D. Most multivitamins contain 400 IU of vitamin D. Vitamin D supplements can be taken on their own, or with calcium or food.
Adults who are vitamin D deficient require treatment with higher doses of vitamin D, may be treated with 50,000 IU of vitamin D2 or vitamin D3 once a week or the equivalent daily dose (7000 IU vitamin D2 or vitamin D3) for 8–12 weeks to achieve a 25(OH)D blood level of approximately 30 ng/ml. This regimen should be followed by maintenance therapy of 1500–2000 IU/day or whatever dose is needed to maintain the target blood level 55, 56.
Vitamin D deficiency can lead to secondary hyperparathyroidism with normal levels of blood calcium. It should be noted that the optimal range for 25-hydroxyvitamin D is higher than the “normal” ranges reported from clinical laboratories, since these ranges are obtained from a population that includes individuals with sub-optimal levels. Patients can be treated with vitamin D supplementation of 50,000 IU once a week for up to 3 months with follow-up blood tests of vitamin D, calcium, and PTH (parathyroid hormone) levels. Some patients may require longer courses of treatment 57.
What foods provide vitamin D?
The flesh of fatty fish (such as salmon, tuna, and mackerel) and fish liver oils are among the best sources of vitamin D 58, 59. An animal’s diet affects the amount of vitamin D in its tissues. Small amounts of vitamin D are found in beef liver, cheese, and egg yolks. Vitamin D in these foods is primarily in the form of vitamin D3 and its metabolite 25(OH)D3 60. Mushrooms provide variable amounts of vitamin D2 61. Some mushrooms available on the market have been treated with UV light to increase their levels of vitamin D2. In addition, the Food and Drug Administration (FDA) has approved UV-treated mushroom powder as a food additive for use as a source of vitamin D2 in food products 62. Very limited evidence suggests no substantial differences in the bioavailability of vitamin D from various foods 63.
The U.S. Department of Agriculture’s (USDA’s) FoodData Central (https://fdc.nal.usda.gov) lists the nutrient content of many foods and provides a comprehensive list of foods containing vitamin D arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/VitaminD-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/VitaminD-Food.pdf). However, FoodData Central does not include the amounts of 25(OH)D in foods. A variety of foods and their vitamin D levels per serving are listed in Table 3.
Animal-based foods typically provide some vitamin D in the form of 25-hydroxyvitamin D (25(OH)D or calcidiol) in addition to vitamin D3 (cholecalciferol). The impact of this form on vitamin D status is an emerging area of research. Studies show that 25-hydroxyvitamin D (25(OH)D or calcidiol) appears to be approximately five times more potent than the parent vitamin D for raising serum 25(OH)D concentrations 61. One study found that when the 25-hydroxyvitamin D (25(OH)D or calcidiol) content of beef, pork, chicken, turkey, and eggs is taken into account, the total amount of vitamin D in the food is 2 to 18 times higher than the amount in the parent vitamin D alone, depending on the food 64.
Fortified foods provide most of the vitamin D in the American diet 58, 65. For example, almost all of the U.S. milk supply is voluntarily fortified with about 3 mcg/cup (120 IU), usually in the form of vitamin D3 66. In the 1930s, a milk fortification program was implemented in the United States to combat rickets, then a major public health problem 58. In Canada, milk must be fortified with 0.88–1.0 mcg/100 mL (35–40 IU), and the required amount for margarine is at least 13.25 mcg/100 g (530 IU). Other dairy products made from milk, such as cheese and ice cream, are not usually fortified in the United States or Canada. Plant milk alternatives (such as beverages made from soy, almond, or oats) are often fortified with similar amounts of vitamin D to those in fortified cow’s milk (about 3 mcg [120 IU]/cup); the Nutrition Facts label lists the actual amount 67. Ready-to-eat breakfast cereals often contain added vitamin D, as do some brands of orange juice, yogurt, margarine, and other food products.
Both the United States and Canada mandate the fortification of infant formula with vitamin D: 1–2.5 mcg/100 kcal (40–100 IU) vitamin D in the United States and 1–2 mcg/100 kcal (40–80 IU) in Canada 58.
Fortified foods provide most of the vitamin D in American diets 58:
- Fatty fish such as salmon, tuna, and mackerel are among the best sources.
- Beef liver, cheese, and egg yolks provide small amounts.
- Mushrooms provide some vitamin D. In some mushrooms that are newly available in stores, the vitamin D content is being boosted by exposing these mushrooms to ultraviolet light.
- Almost all of the U.S. milk supply is fortified with 400 IU of vitamin D per quart. But foods made from milk, like cheese and ice cream, are usually not fortified.
- Vitamin D is added to many breakfast cereals and to some brands of orange juice, yogurt, margarine, and soy beverages; check the labels.
A variety of foods and their vitamin D levels per serving are listed in Table 5.
Table 5. Vitamin D content of selected foods
| Food | Micrograms (mcg) per serving | International Units (IU) per serving | Percent DV* |
|---|---|---|---|
| Cod liver oil, 1 tablespoon | 34 | 1360 | 170 |
| Trout (rainbow), farmed, cooked, 3 ounces | 16.2 | 645 | 81 |
| Salmon (sockeye), cooked, 3 ounces | 14.2 | 570 | 71 |
| Mushrooms, white, raw, sliced, exposed to UV light, ½ cup | 9.2 | 366 | 46 |
| Milk, 2% milkfat, vitamin D fortified, 1 cup | 2.9 | 120 | 15 |
| Soy, almond, and oat milks, vitamin D fortified, various brands, 1 cup | 2.5-3.6 | 100-144 | 13-18 |
| Ready-to-eat cereal, fortified with 10% of the DV for vitamin D, 1 serving | 2 | 80 | 10 |
| Sardines (Atlantic), canned in oil, drained, 2 sardines | 1.2 | 46 | 6 |
| Egg, 1 large, scrambled** | 1.1 | 44 | 6 |
| Liver, beef, braised, 3 ounces | 1 | 42 | 5 |
| Tuna fish (light), canned in water, drained, 3 ounces | 1 | 40 | 5 |
| Cheese, cheddar, 1.5 ounce | 0.4 | 17 | 2 |
| Mushrooms, portabella, raw, diced, ½ cup | 0.1 | 4 | 1 |
| Chicken breast, roasted, 3 ounces | 0.1 | 4 | 1 |
| Beef, ground, 90% lean, broiled, 3 ounces | 0 | 1.7 | 0 |
| Broccoli, raw, chopped, ½ cup | 0 | 0 | 0 |
| Carrots, raw, chopped, ½ cup | 0 | 0 | 0 |
| Almonds, dry roasted, 1 ounce | 0 | 0 | 0 |
| Apple, large | 0 | 0 | 0 |
| Banana, large | 0 | 0 | 0 |
| Rice, brown, long-grain, cooked, 1 cup | 0 | 0 | 0 |
| Whole wheat bread, 1 slice | 0 | 0 | 0 |
| Lentils, boiled, ½ cup | 0 | 0 | 0 |
| Sunflower seeds, roasted, ½ cup | 0 | 0 | 0 |
| Edamame, shelled, cooked, ½ cup | 0 | 0 | 0 |
Footnotes:
* DV = Daily Value. The FDA developed DVs to help consumers compare the nutrient contents of foods and dietary supplements within the context of a total diet. The DV for vitamin D is 20 mcg (800 IU) for adults and children aged 4 years and older 68. The labels must list vitamin D content in mcg per serving and have the option of also listing the amount in IUs in parentheses. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
** Vitamin D is in the yolk.
[Source 69 ]Other Nutrients Important to Bone
The Institute of Medicine 54 recently provided recommended intakes for other bone-related nutrients, including phosphorus and magnesium (see Table 6: Adequate Intakes (Al) or Recommended Daily Allowances (RDA) and Tolerable Upper Intake Levels (UL) for Calcium, Vitamin D, Phosphorus, and Magnesium by Life-Stage Group for United States and Canada). Most Americans consume adequate quantities of phosphorus through their regular intake of meats, cereals, milk, and processed foods. While some beverages such as soft drinks also contain phosphorus, they are not a preferred source of phosphorus because they may displace calcium-rich beverages like milk 70.
Magnesium intakes may be suboptimal in those who do not eat enough green leafy vegetables, whole grains, nuts, and dairy products. Fortunately, most diets contain adequate levels of other bone-related micronutrients, such as vitamins K and C, copper, manganese, zinc, and iron, to promote bone health.
Some dietary components may potentially have negative effects on bone health, especially if calcium intakes are not adequate. For example, high levels of sodium or caffeine intake can increase calcium excretion in the urine. The effects of these factors can be overcome by increasing the amount of calcium in the diet 71. Studies have linked excessive amounts of phosphorus to altered calcium metabolism, but it appears that the typical level of phosphorus consumed by most individuals in the United States should not negatively affect bone health 72. Excessive amounts of preformed vitamin A (e.g., retinol) can also have negative effects on bone, so individuals should not consume more than the recommended dietary allowance for this vitamin 73. The vitamin A precursor (beta carotene) found in many fruits and vegetables does not have negative effects on bone, however.
Table 6. Adequate Intakes (Al) or Recommended Daily Allowances (RDA) and Tolerable Upper Intake Levels (UL) for Calcium, Vitamin D, Phosphorus, and Magnesium by Life-Stage Group for United States and Canada
| Life-stage group | Calcium (mg/day) | Vitamin D (IU/day) | Phosphorous (mg/day) | Magnesium (mg/day) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Al | UL | Al | UL | RDA | UL | RDA | UL† | ||
| Male | Female | ||||||||
| 0–6 months | 210 | ND* | 200 | 1000 | 100 | ND* | 30 | 30 | ND* |
| 7–12 months | 270 | ND* | 200 | 1000 | 275 | ND* | 75 | 75 | ND* |
| 1–3 years | 500 | 2500 | 200 | 2000 | 460 | 3000 | 80 | 80 | 65 |
| 4–8 years | 800 | 2500 | 200 | 2000 | 500 | 3000 | 130 | 130 | 110 |
| 9–13 years | 1300 | 2500 | 200 | 2000 | 1250 | 4000 | 240 | 240 | 350 |
| 14–18 years | 1300 | 2500 | 200 | 2000 | 1250 | 4000 | 410 | 360 | 350 |
| 19–30 years | 1000 | 2500 | 200 | 2000 | 700 | 4000 | 400 | 310 | 350 |
| 31–50 years | 1000 | 2500 | 200 | 2000 | 700 | 4000 | 420 | 320 | 350 |
| 51–70 years | 1200 | 2500 | 400 | 2000 | 700 | 4000 | 420 | 320 | 350 |
| > 70 years | 1200 | 2500 | 600 | 2000 | 700 | 3000 | 420 | 320 | 350 |
| Pregnancy: | |||||||||
| <18 years | 1300 | 2500 | 200 | 2000 | 1250 | 3500 | 400 | 350 | |
| 19–30 years | 1000 | 2500 | 200 | 2000 | 700 | 3500 | 350 | 350 | |
| 31–50 years | 1000 | 2500 | 200 | 2000 | 700 | 3500 | 360 | 350 | |
| Lactation: | |||||||||
| <18 years | 1300 | 2500 | 200 | 2000 | 1250 | 4000 | 360 | 350 | |
| 19–3 years | 1000 | 2500 | 200 | 2000 | 700 | 4000 | 310 | 350 | |
| 31–50 years | 1000 | 2500 | 200 | 2000 | 700 | 4000 | 320 | 350 |
Footnote: Represents intake from pharmacological agents only, does not include intake from food and water.
Abbreviations: AI = Adequate Intakes; UL = Tolerable Upper Intake Levels (represents intake from pharmacological agents only, does not include intake from food and water.); RDA = Recommended Daily Allowances; ND = Not Determinable
[Source 74 ]Vitamin K and Osteoporosis
Vitamin K has thus been clinically applied for the treatment and prevention of osteoporosis 75, 76, 77, 78. Vitamin K is the term used to name a family of fat-soluble compounds that is naturally present in some foods and is available as a dietary supplement that is important for blood clotting and healthy bones and other diverse physiological functions 79. The three main forms are vitamin K are phylloquinone (vitamin K1), menaquinones (vitamin K2) and menadione (vitamin K3) 80.
Vitamin K1 (phylloquinone), which is the major dietary source, is concentrated in leafy vegetables (e.g., green vegetables) because it is directly involved in photosynthesis and is the vitamin K form best characterized in terms of food composition and dietary intakes. Vitamin K1 (phylloquinone) is active in animals and is responsible for the production of coagulation factors. Vitamin K1 (phylloquinone) is also can be converted into vitamin K2 (menaquinones) in animals 80. Vitamin K2 or menaquinones are the product of bacterial production or intestinal bacteria conversion from dietary vitamin K1 (phylloquinone) and are also found in fermented foods (e.g., cheeses and the Japanese soybean product natto) (Figure 1) 81, 82. Vitamin K2 (menaquinones) have unsaturated isoprenyl side chains and are designated as MK-4 through MK-13, based on the length of their side chain 80, 83. MK-4, MK-7, and MK-9 are the most well-studied menaquinones. Food composition databases are limited for vitamin K2 (menaquinones) and their presence in foods varies by region. Dietary intakes of all forms of vitamin K vary widely among age groups and population subgroups. Similarly, the utilization of vitamin K from different forms and food sources appear to vary, although our understanding of vitamin K is still rudimentary in light of new developments regarding the vitamin K2 (menaquinones) 84.
In the United States, vitamin K3 (menadione) is used in poultry feed and some swine feeds as a source of vitamin K 80. As such, menaquinone-4 (MK-4) formed from vitamin K3 (menadione) is present in poultry and pork products in the U.S. food supply and is the primary dietary source of MK-4 85. Menaquinone-4 (MK-4) is present at high concentrations in human, poultry and pork tissues 86. Although humans generally obtain vitamin K1 (phylloquinone) and menaquinone-7 (MK-7) from the diet, intake of menaquinone-4 (MK-4) in animal foods is extremely low. Vitamin K3 (menadione), a synthetic vitamin K analog (Figure 1), is the primary source of vitamin K in poultry feed and some swine feeds, along with small amounts of phylloquinone (vitamin K1) 80. As such, MK-4 formed from vitamin K3 (menadione) is present in poultry and pork products in the U.S. food supply and is the primary dietary source of MK-4 85. Although menaquinone-4 (MK-4) is also formed from tissue-specific conversion of phylloquinone (vitamin K1) 87, the impact on dietary intake from this conversion is likely negligible as animal organs containing high MK-4 concentrations including kidney, brain, and pancreas, are not commonly consumed in most regions of the world. Menaquinone-4 (MK-4) is also found in modest amounts in milk, butter, and cheeses, which may make a small contribution to total vitamin K intake. The high consumption of poultry, pork, and dairy products in the United States 88, however, suggests that MK-4 may make a relevant contribution to total vitamin K intake. In regions where food systems do not use vitamin K3 (menadione) in animal feed or consumption of dairy products is low, MK-4 is most likely not an important dietary source of vitamin K. For example, MK-4 has been estimated to account for ∼3% of total vitamin K intake in the Netherlands 89 and is found in animal products in relatively lower amounts compared with the United States and Japan 86.
Menaquinone-4 (MK-4) is unique among the vitamin K2 (menaquinones) in that it is produced by the body from vitamin K1 (phylloquinone) via a conversion process that does not involve bacterial action. Instead, menaquinone-4 (MK-4) is formed by a realkylation step from vitamin K3 (menadione) present in animal feeds or is the product of tissue-specific conversion directly from dietary vitamin K1 (phylloquinone) 90, 91, 92. In the United States, vitamin K3 (menadione) is the synthetic form of vitamin K used in poultry feed. As such, MK-4 formed from vitamin K3 (menadione) is present in poultry products in the US food supply 93. However, MK-4 formed from vitamin K1 (phylloquinone) is limited to organs not commonly consumed in the diet including kidney. The exceptions are dairy products with menaquinone-4 (MK-4) found in milk, butter, and cheese, albeit in modest amounts. Therefore it is unlikely that menaquinone-4 (MK-4) is an important dietary source of vitamin K in food supplies that do not use vitamin K3 (menadione) for poultry feed nor are rich in dairy products.
Matrix Gla-protein, a vitamin K-dependent protein present in vascular smooth muscle, bone, and cartilage, is the focus of considerable scientific research because it might help reduce abnormal calcification 94, 95. Low plasma concentrations of vitamin K are associated with a high risk of bone fractures in both northern Europeans and Asians populations of both sexes 96, 97, 98.
Vitamin K is a cofactor for the gamma-carboxylation of many proteins, including osteocalcin, one of the main proteins in bone 99. Some research indicates that high serum levels of undercarboxylated osteocalcin are associated with lower bone mineral density 79, 99. Some, but not all, studies also link higher vitamin K intakes with higher bone mineral density and/or lower hip fracture incidence 100, 101, 102, 103, 104, 105.
Although vitamin K is involved in the carboxylation of osteocalcin, it is unclear whether supplementation with any form of vitamin K reduces the risk of osteoporosis. Wu et al. 106 showed that both phylloquinone (vitamin K1) and vitamin K2 or menaquinones (MK-4 and MK-7) inhibit osteoclast-mediated effects on bone resorption in a dose dependent manner. Furthermore, Rangel et al. 107 demonstrated increased compact bone mass, increased bone formation markers and decreased bone resorption markers in ovariectomized mice supplemented with vitamin K. Also, the effect of coadministration of vitamin K2 (menaquinones) and other antiosteoporotic drugs, such as Teriparatide in ovariectomized mice 108 and bisphosphonates, has been investigated in uremic osteoporosis (chronic kidney disease–related osteoporosis) 109.
In 2006, Cockayne and colleagues conducted a systematic review and meta-analysis of randomized controlled trials that examined the effects of vitamin K supplementation on bone mineral density and bone fracture 110. Most of the trials were conducted in Japan and involved postmenopausal women; trial duration ranged from 6 to 36 months. Thirteen trials were included in the systematic review, and 12 showed that supplementation with either phytonadione or MK-4 improved bone mineral density. Seven of the 13 trials also had fracture data that were combined in a meta-analysis. All of these trials used MK-4 at either 15 mg/day (1 trial) or 45 mg/day (6 trials). MK-4 supplementation significantly reduced rates of hip fractures, vertebral fractures, and all nonvertebral fractures.
In their meta-analysis, Hao et al. 111 showed a statistically significant inverse association between dietary vitamin phylloquinone (vitamin K1) intake and risk of fractures (highest vs. the lowest intake). The authors did not find any significant association between low vitamin phylloquinone (vitamin K1) and bone mineral density (BMD) 111. Recently, 374 postmenopausal women with osteoporosis were studied showing a lower serum vitamin phylloquinone (vitamin K1) in the group with fractures (prevalent fractures: 0.53 (0.41), no fractures: 0.65 (0.66) μg/L) and independently associated with fracture risk 112. Dp-uc MGP was detectable in 97 (75%) participants with serum vitamin phylloquinone (vitamin K1) of 0.26 (0.15) μg/L, whilst vitamin K dependent protein PIVKA-II was above the clinical threshold in only 3.8% 112.
To date, a limited number of randomized controlled trials have evaluated the effects of phylloquinone (vitamin K1) and menaquinones (vitamin K2) supplementation on fracture risk showing a potential positive effect and few trials are ongoing 113, 114, 115, 116. In a double blind, randomized, controlled study, 244 postmenopausal women received vitamin K2 MK-7 (180 μg MK-7/day) capsules or placebo for 3 years to investigate its effect on vertebral fractures. MK-7 significantly decreased the loss in vertebral height of the lower thoracic region at the mid-site of the vertebrae after 2 and 3 years 116. An interventional study 241 osteoporotic patients were enrolled in a 24-month randomized open-label study: in the control group (without treatment; n = 121) and the vitamin K2–treated group (n = 120), which received 45 mg/day orally MK-4 (45 mg/day orally). They found a reduction in the vitamin K2-treated group of the incidence of bone fractures lower than the control group 117.
In Japan, vitamin K2 MK-4 was approved for a drug for osteoporosis treatment in 1995 based on domestic clinical trials showing the efficacy on bone mineral density. Now, MK-4 is in use for osteoporosis treatment in several Asian countries. For the last two decades, interventional clinical trials were conducted throughout the world. Many trials used MK-4 as vitamin K treatment, MK-7 or vitamin K1 was also used in some trials as well. According to the most recent meta-analysis 118, a favorable effect of vitamin K on clinical fractures was statistically significant, although the effect on vertebral or hip fractures was not statistically significant. Among the clinical trials, the largest one was conducted in Japan 119. This study involved more than 4000 Japanese women with three years of intervention and a one-year follow-up period 119. This study failed to demonstrate the fracture-preventive effect of vitamin K2 (MK-4) in the whole group of subjects 119. However, the significant effect on new vertebral fractures was observed in the subgroup analysis of high-risk patients with at least five pre-existing vertebral fractures 120.
Based on this information, long-term supplementation with vitamin K in postmenopausal women with osteoporosis might have some potential utility, in particular, given its negligible risk of serious side effects. This is also supported by the fact that vitamin K2 MK-4 in relatively high doses (45 mg) is registered in Japan and other parts of Asia for postmenopausal osteoporosis 121, 122, 79. The European Food Safety Authority has approved a health claim for vitamin K, noting that “a cause and effect relationship has been established between the dietary intake of vitamin K and the maintenance of normal bone” 123. The FDA has not authorized a health claim for vitamin K in the United States.
Magnesium and Osteoporosis
Magnesium is an abundant mineral in your body, is naturally present in many foods, added to other food products, available as a dietary supplement, and present in some medicines (such as antacids and laxatives) 124. Approximately 30% to 40% of the dietary magnesium consumed is typically absorbed by the body 125. Magnesium is a cofactor in more than 300 enzyme systems that regulate diverse biochemical reactions in your body, including protein synthesis, muscle and nerve function, blood glucose control, and blood pressure regulation 126. Magnesium is required for energy production, oxidative phosphorylation, and glycolysis. Magnesium is involved in bone formation and influences the activities of osteoblasts and osteoclasts 127. Magnesium also affects the concentrations of both parathyroid hormone (PTH) and the active form of vitamin D, which are major regulators of bone homeostasis. Several population-based studies have found positive associations between magnesium intake and bone mineral density in both men and women 128. Other research has found that women with osteoporosis have lower serum magnesium levels than women with osteopenia and those who do not have osteoporosis or osteopenia 129. These and other findings indicate that magnesium deficiency might be a risk factor for osteoporosis 127.
Magnesium is also required for the synthesis of DNA, RNA, and the antioxidant glutathione. Magnesium also plays a role in the active transport of calcium and potassium ions across cell membranes, a process that is important to nerve impulse conduction, muscle contraction, and normal heart rhythm 126.
Although limited in number, studies suggest that increasing magnesium intakes from food or supplements might increase bone mineral density in postmenopausal and elderly women 130. For example, one short-term study found that 290 mg/day elemental magnesium (as magnesium citrate) for 30 days in 20 postmenopausal women with osteoporosis suppressed bone turnover compared with placebo, suggesting that bone loss decreased 131.
Diets that provide recommended levels of magnesium enhance bone health, but further research is needed to elucidate the role of magnesium in the prevention and management of osteoporosis.
An adult body contains approximately 25 g magnesium, with 50% to 60% present in the bones and most of the rest in soft tissues 132. Less than 1% of total magnesium is in blood serum, and these levels are kept under tight control. Normal serum magnesium concentrations range between 0.75 and 0.95 millimoles (mmol)/L 133. Hypomagnesemia is defined as a serum magnesium level less than 0.75 mmol/L 134. Magnesium homeostasis is largely controlled by the kidney, which typically excretes about 120 mg magnesium into the urine each day 135. Urinary excretion is reduced when magnesium status is low 130.
Assessing magnesium status is difficult because most magnesium is inside cells or in bone 126. The most commonly used and readily available method for assessing magnesium status is measurement of serum magnesium concentration, even though serum levels have little correlation with total body magnesium levels or concentrations in specific tissues 134. Other methods for assessing magnesium status include measuring magnesium concentrations in red blood cells, saliva, and urine; measuring ionized magnesium concentrations in blood, plasma, or serum; and conducting a magnesium-loading (or “tolerance”) test. No single method is considered satisfactory 136. Some experts 132 but not others 126 consider the tolerance test (in which urinary magnesium is measured after parenteral infusion of a dose of magnesium) to be the best method to assess magnesium status in adults. To comprehensively evaluate magnesium status, both laboratory tests and a clinical assessment might be required 134.
How much magnesium do I need?
The amount of magnesium you need depends on your age and sex. Average daily recommended amounts are listed below in milligrams (mg). Table 7 lists the current Recommended Dietary Allowances (RDAs) for magnesium 130. For infants from birth to 12 months, the Food and Nutrition Board at the Institute of Medicine of the National Academies established an Adequate Intake (AI) for magnesium that is equivalent to the mean intake of magnesium in healthy, breastfed infants, with added solid foods for ages 7–12 months.
- Recommended Dietary Allowance (RDA): average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy people.
- Adequate Intake (AI): established when evidence is insufficient to develop an RDA and is set at a level assumed to ensure nutritional adequacy.
- Tolerable Upper Intake Level (UL): maximum daily intake unlikely to cause adverse health effects 130.
Table 7. Recommended Dietary Allowances (RDAs) for Magnesium
| Age | Male | Female | Pregnancy | Lactation |
| Birth to 6 months | 30 mg* | 30 mg* | ||
| 7–12 months | 75 mg* | 75 mg* | ||
| 1–3 years | 80 mg | 80 mg | ||
| 4–8 years | 130 mg | 130 mg | ||
| 9–13 years | 240 mg | 240 mg | ||
| 14–18 years | 410 mg | 360 mg | 400 mg | 360 mg |
| 19–30 years | 400 mg | 310 mg | 350 mg | 310 mg |
| 31–50 years | 420 mg | 320 mg | 360 mg | 320 mg |
| 51+ years | 420 mg | 320 mg |
Footnotes:
Recommended Dietary Allowance (RDA): Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
Adequate Intake (AI): Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an Recommended Dietary Allowance (RDA).
[Source 130 ]What foods provide magnesium?
Magnesium is found naturally in many foods and is added to some fortified foods. Green leafy vegetables, such as spinach, legumes, nuts, seeds, and whole grains, are good sources 126. You can get recommended amounts of magnesium by eating a variety of foods, including the following:
- Legumes, nuts, seeds, whole grains, and green leafy vegetables (such as spinach)
- Fortified breakfast cereals and other fortified foods
- Milk, yogurt, and some other milk products
In general, foods containing dietary fiber provide magnesium. Magnesium is also added to some breakfast cereals and other fortified foods. Some types of food processing, such as refining grains in ways that remove the nutrient-rich germ and bran, lower magnesium content substantially 130. Selected food sources of magnesium are listed in Table 8.
Tap, mineral, and bottled waters can also be sources of magnesium, but the amount of magnesium in water varies by source and brand (ranging from 1 mg/L to more than 120 mg/L) 126.
The U.S. Department of Agriculture’s (USDA’s) FoodData Central (https://fdc.nal.usda.gov) lists the nutrient content of many foods and provides comprehensive list of foods containing magnesium arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/Magnesium-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/Magnesium-Food.pdf).
Table 8. Magnesium content of selected foods
| Food | Milligrams (mg) per serving | Percent DV* |
| Pumpkin seeds, roasted, 1 ounce | 156 | 37 |
| Chia seeds, 1 ounce | 111 | 26 |
| Almonds, dry roasted, 1 ounce | 80 | 19 |
| Spinach, boiled, ½ cup | 78 | 19 |
| Cashews, dry roasted, 1 ounce | 74 | 18 |
| Peanuts, oil roasted, ¼ cup | 63 | 15 |
| Cereal, shredded wheat, 2 large biscuits | 61 | 15 |
| Soymilk, plain or vanilla, 1 cup | 61 | 15 |
| Black beans, cooked, ½ cup | 60 | 14 |
| Edamame, shelled, cooked, ½ cup | 50 | 12 |
| Peanut butter, smooth, 2 tablespoons | 49 | 12 |
| Potato, baked with skin, 3.5 ounces | 43 | 10 |
| Rice, brown, cooked, ½ cup | 42 | 10 |
| Yogurt, plain, low fat, 8 ounces | 42 | 10 |
| Breakfast cereals, fortified with 10% of the DV for magnesium, 1 serving | 42 | 10 |
| Oatmeal, instant, 1 packet | 36 | 9 |
| Kidney beans, canned, ½ cup | 35 | 8 |
| Banana, 1 medium | 32 | 8 |
| Salmon, Atlantic, farmed, cooked, 3 ounces | 26 | 6 |
| Milk, 1 cup | 24–27 | 6 |
| Halibut, cooked, 3 ounces | 24 | 6 |
| Raisins, ½ cup | 23 | 5 |
| Bread, whole wheat, 1 slice | 23 | 5 |
| Avocado, cubed, ½ cup | 22 | 5 |
| Chicken breast, roasted, 3 ounces | 22 | 5 |
| Beef, ground, 90% lean, pan broiled, 3 ounces | 20 | 5 |
| Broccoli, chopped and cooked, ½ cup | 12 | 3 |
| Rice, white, cooked, ½ cup | 10 | 2 |
| Apple, 1 medium | 9 | 2 |
| Carrot, raw, 1 medium | 7 | 2 |
Footnote: *DV = Daily Value. The U.S. Food and Drug Administration (FDA) developed DVs to help consumers compare the nutrient contents of foods and dietary supplements within the context of a total diet. The DV for magnesium is 420 mg for adults and children aged 4 years and older. FDA does not require food labels to list magnesium content unless magnesium has been added to the food. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
[Source 137 ]Magnesium supplements
Magnesium supplements are available in a variety of forms, including magnesium oxide, citrate, and chloride 126. The Supplement Facts panel on a dietary supplement label declares the amount of elemental magnesium in the product, not the weight of the entire magnesium-containing compound.
Absorption of magnesium from different kinds of magnesium supplements varies. Forms of magnesium that dissolve well in liquid are more completely absorbed in the gut than less soluble forms 138. Small studies have found that magnesium in the aspartate, citrate, lactate, and chloride forms is absorbed more completely and is more bioavailable than magnesium oxide and magnesium sulfate 139. One study found that very high doses of zinc from supplements (142 mg/day) can interfere with magnesium absorption and disrupt the magnesium balance in the body 140.
Several types of medications have the potential to interact with magnesium supplements or affect magnesium status. A few examples are provided below. People taking these and other medications on a regular basis should discuss their magnesium intakes with their healthcare providers.
- Bisphosphonates: Magnesium-rich supplements or medications can decrease the absorption of oral bisphosphonates, such as alendronate (Fosamax®), used to treat osteoporosis 141. Use of magnesium-rich supplements or medications and oral bisphosphonates should be separated by at least 2 hours.
- Antibiotics: Magnesium can form insoluble complexes with tetracyclines, such as demeclocycline (Declomycin®) and doxycycline (Vibramycin®), as well as quinolone antibiotics, such as ciprofloxacin (Cipro®) and levofloxacin (Levaquin®). These antibiotics should be taken at least 2 hours before or 4–6 hours after a magnesium-containing supplement 142.
- Diuretics: Chronic treatment with loop diuretics, such as furosemide (Lasix®) and bumetanide (Bumex®), and thiazide diuretics, such as hydrochlorothiazide (Aquazide H®) and ethacrynic acid (Edecrin®), can increase the loss of magnesium in urine and lead to magnesium depletion 143. In contrast, potassium-sparing diuretics, such as amiloride (Midamor®) and spironolactone (Aldactone®), reduce magnesium excretion 143.
- Proton pump inhibitors: Prescription proton pump inhibitor (PPI) drugs, such as esomeprazole magnesium (Nexium®) and lansoprazole (Prevacid®), when taken for prolonged periods (typically more than a year) can cause hypomagnesemia 144. In cases that FDA reviewed, magnesium supplements often raised the low serum magnesium levels caused by PPIs. However, in 25% of the cases, supplements did not raise magnesium levels and the patients had to discontinue the PPI. FDA advises healthcare professionals to consider measuring patients’ serum magnesium levels prior to initiating long-term PPI treatment and to check magnesium levels in these patients periodically 144.
Health risks from excessive magnesium
Too much magnesium from food does not pose a health risk in healthy individuals because the kidneys eliminate excess amounts in the urine 145. However, high doses of magnesium from dietary supplements or medications often result in diarrhea that can be accompanied by nausea and abdominal cramping 130. Forms of magnesium most commonly reported to cause diarrhea include magnesium carbonate, chloride, gluconate, and oxide 138. The diarrhea and laxative effects of magnesium salts are due to the osmotic activity of unabsorbed salts in the intestine and colon and the stimulation of gastric motility.
Very large doses of magnesium-containing laxatives and antacids (typically providing more than 5,000 mg/day magnesium) have been associated with magnesium toxicity 146, including fatal hypermagnesemia in a 28-month-old boy 147 and an elderly man 148. Symptoms of magnesium toxicity, which usually develop after serum concentrations exceed 1.74–2.61 mmol/L, can include hypotension, nausea, vomiting, facial flushing, retention of urine, ileus, depression, and lethargy before progressing to muscle weakness, difficulty breathing, extreme hypotension, irregular heartbeat, and cardiac arrest 145. The risk of magnesium toxicity increases with impaired renal function or kidney failure because the ability to remove excess magnesium is reduced or lost 145.
The Food and Nutrition Board at the Institute of Medicine of the National Academies has established Tolerable Upper Intake Levels (ULs) for magnesium that apply only to supplemental magnesium for healthy infants, children, and adults (see Table 9) 130.
Table 9. Tolerable Upper Intake Levels (ULs) for Supplemental Magnesium
| Age | Male | Female | Pregnant | Lactating |
| Birth to 12 months | None established | None established | ||
| 1–3 years | 65 mg | 65 mg | ||
| 4–8 years | 110 mg | 110 mg | ||
| 9–18 years | 350 mg | 350 mg | 350 mg | 350 mg |
| 19+ years | 350 mg | 350 mg | 350 mg | 350 mg |
Physical Activity
Weight-bearing, strength, and balance-training exercises are also an important part of any osteoporosis prevention and treatment program, regardless of age. They can help increase or preserve bone mass and may also help reduce the risk of falling. All types of physical activity can contribute to bone health. Activities that are weight bearing or involve impact are most useful for increasing or maintaining bone mass. Since continued physical activity provides a positive stimulus for bone, muscle, and other aspects of health, a lifelong commitment to physical activity and exercise is critical. Ending a physical activity regimen will result in bone mass returning to the level that existed before the activity began. Since repetitive programs of physical activity may be discontinued due to lack of motivation or interest, variety and creativity are important if physical activity is to be continued over the long term.
Physical activity will only affect bone at the skeletal sites that are stressed (or loaded) by the activity. In other words, physical activity programs do not necessarily benefit the whole skeleton, although any type of activity provides more benefit to bone than does no activity at all. For bone gain to occur, the stimulus must be greater than that which the bone usually experiences. Static loads applied continuously (such as standing) do not promote increased bone mass.
Complete lack of activity, such as periods of immobility, causes bone loss. When it is not possible to avoid immobility (e.g., bed rest during sickness), even brief daily weight-bearing movements can help to reduce bone loss. General physical activity every day and some weight-bearing, strength-building, and balance-enhancing activities 2 or more times a week are generally effective for promoting bone health for most persons.
Any activity that imparts impact (such as jumping or skipping) may increase bone mass more than will low- and moderate-intensity, endurance-type activities, such as brisk walking. However, endurance activities may still play an important role in skeletal health by increasing muscle mass and strength, balance, and coordination, and they may also help prevent falls in the elderly. Endurance activity is also very important for other aspects of health, such as helping to prevent obesity, diabetes, or cardiovascular disease.
Load-bearing physical activities such as jumping need not be engaged in for long periods of time to provide benefits to skeletal health. In fact, 5–10 minutes daily may suffice. Most adults should begin with weight-bearing exercise and gradually add some skipping and jumping activity. Longer periods (30–45 minutes) may be needed for weight training or walking/jogging. Those who have been inactive should work up to this amount of time gradually using a progressive program, e.g., start with shorter times and easier activities (light weights or walking) and then increase time or intensity slowly (by no more than 10 percent each week) in order to avoid injury.
Activities that are not weight bearing or are low impact may help improve balance and coordination and maintain muscle mass, which can help prevent falls. To encourage increased levels of physical activity among all age groups, “Physical Activity and Health: A Surgeon General’s Report” 149 recommends a “minimum of 30 minutes of physical activity of moderate intensity (such as brisk walking) on most, if not all, days of the week”. Since the skeleton responds preferentially to strength training and short bouts of high-load impact activity (such as skipping or jumping), the same report recommends that adults supplement their cardiorespiratory endurance activity with strength-developing exercise at least two times per week.
For those who cannot engage in regular physical activity due to disability, mechanical stimulation of the skeleton might prove beneficial. Recent, small studies found that use of vibrating platforms increased BMD (bone mineral density) and slowed bone loss 150, 151, 152. This may provide another way to reduce fracture risk both in the elderly and in younger individuals with disabling conditions that limit their ability to exercise. However, the long-term safety and efficacy of such approaches remain to be determined, and therefore specific rehabilitation and exercise programs aimed at increasing activity and function remain critically important in the frail elderly and in younger individuals with neuromuscular disabilities.
As noted earlier, the evidence does not lead to a specific set of exercises or practices but rather a set of principles that can be applied and varied according to the age and current physical condition of an individual. Many of these principles have been reviewed by expert panels of the American College of Sports Medicine 153 and they lead to the following suggestions for the frequency, intensity, length, and type of physical activity regimens to benefit bone health for individuals of all ages:
- Physical activities that include a variety of loading patterns (such as strength training or aerobic classes) may promote increased bone mass more than do activities that involve normal or regular loading patterns (such as running).
- General physical activity every day and some weight-bearing, strength-building, and balance-enhancing activities 2 or more times a week are generally effective for promoting bone health for most persons.
- Any activity that imparts impact (such as jumping or skipping) may increase bone mass more than will low- and moderate-intensity, endurance-type activities, such as brisk walking. However, endurance activities may still play an important role in skeletal health by increasing muscle mass and strength, balance, and coordination, and they may also help prevent falls in the elderly. Endurance activity is also very important for other aspects of health, such as helping to prevent obesity, diabetes, or cardiovascular disease.
- Load-bearing physical activities such as jumping need not be engaged in for long periods of time to provide benefits to skeletal health. In fact, 5–10 minutes daily may suffice. Most adults should begin with weight-bearing exercise and gradually add some skipping and jumping activity. Longer periods (30–45 minutes) may be needed for weight training or walking/jogging. Those who have been inactive should work up to this amount of time gradually using a progressive program, e.g., start with shorter times and easier activities (light weights or walking) and then increase time or intensity slowly (by no more than 10 percent each week) in order to avoid injury.
- Physical activities that include a variety of loading patterns (such as strength training or aerobic classes) may promote increased bone mass more than do activities that involve normal or regular loading patterns (such as running).
Physical Activity for Older Adults
Most elderly individuals should strongly consider engaging in regular physical activity. Physical activity is the only single therapy that can simultaneously improve muscle mass, muscle strength, balance, and bone strength. As a result, it may decrease the risk of fractures, in part by reducing the risk of falling. In fact, fall-risk reduction may be the biggest benefit of physical activity for the elderly.
This summary of a Cochrane review 154 presents what we know from research about the effect of exercise on bone mass in postmenopausal women. The review shows that for postmenopausal women the results suggest a relatively small statistically significant, but possibly important, effect of exercise on bone density compared with control groups. Exercise has the potential to be a safe and effective way to avert bone loss in postmenopausal women.
- Exercise will improve bone mineral density slightly.
- Exercise will reduce the chances of having a fracture slightly.
The following guidelines should be used to maximize the potential fall prevention benefits of physical activity in the elderly:
- Physical activity needs to be of sufficient intensity to improve muscle strength, since poor muscle strength is a known risk factor for falls. Strength or resistance training is best for building muscle, but even aerobic endurance activity can yield some improvements in muscle strength.
- Improving balance can be an important component of any physical activity program designed to decrease falls. This program may include balance training exercises or a movement activity such as Tai Chi. Any activity that requires weight bearing and challenges the postural system can improve balance and potentially help reduce falls.
- Physical activity must be performed on average 3 times per week for 30–45 minutes per session for at least three months for strength and balance benefits to be realized, and it must be continued if benefits are to be maintained.
- Those who suffer a fall that requires a visit to a health care provider or an emergency room should ask for a fall risk assessment that includes a program of physical activity.
Fall Prevention
Falls are not just the result of getting older and falls represent perhaps the biggest threat to the bone health and the functional independence of older individuals. Falls are common and frequently are the precipitating event that leads to a fracture or fractures in an individual. Thus, fall prevention offers another important opportunity to protect the bones throughout life, but particularly in those over age 60. Falls occur for a variety of reasons, with multiple factors often contributing to a single fall. These factors include problems with balance, mobility, vision, lower extremity weakness, and/or blood pressure or circulation. Often these problems are compounded by an acute illness (e.g., infection, fever, dehydration, arrhythmia), a new medication, or an environmental stress (e.g., standing or walking on an unsafe surface, poor lighting) that leads to the fall. To reduce the risk of falls, a variety of fall prevention measures should be encouraged for frail, elderly individuals. These include regular vision checks; elimination (where possible) of medications and/or dosages that may cause dizziness, low blood pressure, or confusion; and addressing environmental problems or obstacles that can lead to falls, including removing throw rugs, installing night lights, installing railings on stairs and grab bars in showers, encouraging use of rubber-soled shoes and slippers, and attaching phone cords and other wires to the baseboard of the wall. Hip protectors or hip pads might also be useful in reducing the impact of those falls that do occur.
Many falls can be prevented. Falls are usually caused by a number of things. By changing some of these things, you can lower your chances of falling:
- Begin a regular exercise program: Exercise is one of the most important ways to reduce your chances of falling. It makes you stronger and helps you feel better. Exercises that improve balance and coordination (like tai chi) are the most helpful. Lack of exercise leads to weakness and increases your chances of falling. Ask your doctor or health care worker about the best type of exercise program for you.
- Have your eyes checked by an eye doctor. You may be wearing the wrong glasses or have a condition such as glaucoma or cataracts that limits your vision. Poor vision can increase your chances of falling.
- Make your home safer: About half of all falls happen at home. To make your home safer:
- Remove things you can trip over (such as papers, books, clothes, and shoes) from stairs and places where you walk.
- Remove small throw rugs or use double-sided tape to keep the rugs from slipping.
- Keep items you use often in cabinets you can reach easily without using a stepstool.
- Have grab bars put in next to your toilet and in the tub or shower.
- Use nonslip mats in the bathtub and on shower floors.
- Improve the lighting in your home. As you get older, you need brighter lights to see well. Lamp shades or frosted bulbs can reduce glare.
- Have handrails and lights put in on all staircases.
- Wear shoes that give good support and have thin nonslip soles. Avoid wearing slippers and athletic shoes with deep treads.
Nutrition
Nutrition has been shown to be important during recovery from hip fracture. Supplementation with calcium, vitamin D, and protein (20 grams per day) have been reported to improve hospital and rehabilitation courses and to increase bone mineral density a year after the fracture 155.
- Healthy nutrition, since many nutrients are important for bone health, it is important to eat a well-balanced diet containing a variety of foods. Following the Dietary Guidelines for Americans (2015-2020) 156. From childhood into old age, a diet low in calcium and vitamin D can increase your risk of osteoporosis and fractures. Excessive dieting or inadequate caloric intake can also be bad for bone health. People who are very thin and do not have much body fat to cushion falls have an increased risk of fracture.
In addition to having a healthy diet, sufficient physical activity, and avoiding falls, there are some other bone-healthy behaviors that can help protect the skeleton throughout life:
- Maintain a healthy body weight.
- Avoid smoking. Most studies indicate that smoking is a risk factor for osteoporosis and fracture, although the exact reasons for the harmful effects of tobacco use on bone health are unclear.
- If you drink alcoholic beverages, do so in moderation (i.e., one drink per day for women and two drinks per day for men). People who drink heavily are more prone to bone loss and fractures because of poor nutrition and harmful effects on calcium balance and hormonal factors. Drinking too much also increases the risk of falling, which is likely to increase fracture risk 157.
- For women, see a health care provider if menstrual periods stop for three months.
- For those who have a medical condition or who use medications that can affect the skeleton, talk to a health care provider about ways to safeguard your skeleton.
- An inactive lifestyle or extended bed rest: Low levels of physical activity and prolonged periods of inactivity can contribute to an increased rate of bone loss. They also leave you in poor physical condition, which can increase your risk of falling and breaking a bone.
Signs and symptoms of osteoporosis
You may not know you have osteoporosis until your symptoms are severe. Patients with osteoporosis are asymptomatic unless a fracture has occurred. Sometimes there are obvious signs that a person has osteoporosis – for example they may ”shrink” a little and develop a stooped posture. But often the first sign that someone has osteoporosis is when they break a bone, sometimes without knowing how or why it happened. This kind of break is called a “spontaneous fracture.” When bone mass is lost the risk of breaking a bone (fractures) is higher. Osteoporosis that has already caused a fracture is referred to as “established” osteoporosis.
Once your bones have been weakened by osteoporosis, you might have signs and symptoms of osteoporosis that include:
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped posture or a hunched back
- A bone that breaks much more easily than expected
The bones of the spinal column (vertebrae) are the most likely to break or “collapse” in someone who has osteoporosis. Sometimes this will cause back pain, but most people do not notice anything.
Broken vertebrae are one reason why many older people stoop over and develop what is often called a “dowager’s hump” at the top of their spine.
Osteoporosis also commonly affects the wrist, the upper arm and the femur (thigh bone).
Nonvertebral fractures are typically symptomatic, but about two thirds of vertebral compression fractures are asymptomatic (although patients may have underlying chronic back pain due to other causes such as osteoarthritis). A vertebral compression fracture that is symptomatic begins with acute onset of pain that usually does not radiate, is aggravated by weight bearing, may be accompanied by point spinal tenderness, and typically begins to subside in 1 week. However, residual pain may last for months or be constant.
Multiple thoracic compression fractures eventually cause dorsal kyphosis, with exaggerated cervical lordosis (dowager’s hump). Abnormal stress on the spinal muscles and ligaments may cause chronic, dull, aching pain, particularly in the lower back. Patients may have shortness of breath due to the reduced intrathoracic volume and/or abdominal discomfort due to the compression of the abdominal cavity as the rib cage approaches the pelvis.
Osteoporosis complications
Bone fractures, particularly in the spine or hip, are the most serious complications of osteoporosis. Hip fractures often are caused by a fall and can result in disability and even an increased risk of death within the first year after the injury.
In some cases, spinal fractures can occur even if you haven’t fallen. The bones that make up your spine (vertebrae) can weaken to the point of collapsing, which can result in back pain, lost height and a hunched forward posture.
Figure 2. Common bone fracture areas in osteoporosis
[Source 11 ]Figure 3. Spine x-rays showing severe compression fractures due to osteoporosis
Footnotes: Spine x-ray imaging as obtained from on DEXA scanner. Normal spine (a); young woman with vertebral deformities (arrows) after post partum osteoporosis (b); severe osteoporosis in 68 year old woman with multiple moderate and severe compression fractures (c)
[Source 19 ]How is Osteoporosis Diagnosed?
To diagnose osteoporosis, your doctor will do a bone density scan called a dual energy X-ray absorptiometry (DEXA or DXA) scan. This is a common test that measures your bone density. During this painless test, you lie on a padded table as a scanner passes over your body. The DEXA bone scan often checks your hips, spine, and wrist. These are the most common places to have osteoporosis.
The American Academy of Family Physicians does not recommend that doctors use DEXA scans for women younger than 65 or men younger than 70 unless there are risk factors 5. The American Academy of Family Physicians recommends that women who are 65 years and older or have an equal or greater fracture risk be screened for osteoporosis 5.
Bone density scan
Bone density scan also called bone densitometry, dual-energy x-ray absorptiometry, DEXA or DXA, uses a very small dose of ionizing radiation to produce pictures of the inside of your body (usually the lower lumbar spine and hips) to measure bone mineral density (BMD) or bone loss.
DEXA scan is most often used to diagnose osteoporosis, to assess an individual’s risk for developing osteoporotic fractures. DEXA is also effective in tracking the effects of treatment for osteoporosis and other conditions that cause bone loss.
The DEXA bone scan can also assess an individual’s risk for developing fractures. The risk of fracture is affected by age, body weight, history of prior fracture, family history of osteoporotic fractures and life style issues such as cigarette smoking and excessive alcohol consumption. These factors are taken into consideration when deciding if a patient needs therapy.
DEXA scan is simple, quick and noninvasive. It’s also the most commonly used and the most standard method for diagnosing osteoporosis. The DEXA bone density test is usually completed within 10 to 30 minutes, depending on the equipment used and the parts of the body being examined.
Bone density testing is strongly recommended if you 158:
- are a post-menopausal woman and not taking estrogen.
- have a personal or maternal history of hip fracture or smoking.
- are a post-menopausal woman who is tall (over 5 feet 7 inches) or thin (less than 125 pounds).
- are a man with clinical conditions associated with bone loss, such as rheumatoid arthritis, chronic kidney disease or liver disease.
- use medications that are known to cause bone loss, including corticosteroids such as Prednisone, various anti-seizure medications such as Dilantin and certain barbiturates, or high-dose thyroid replacement drugs.
- have type 1 diabetes, liver disease, kidney disease or a family history of osteoporosis.
- have high bone turnover, which shows up in the form of excessive collagen in urine samples.
- have a thyroid condition, such as hyperthyroidism (overactive thyroid).
- have a parathyroid condition, such as hyperparathyroidism.
- have experienced a fracture after only mild trauma.
- have had x-ray evidence of vertebral fracture or other signs of osteoporosis.
An additional procedure called Vertebral Fracture Assessment (VFA) is now being done at many centers. The Vertebral Fracture Assessment (VFA) is a low-dose x-ray examination of the spine to screen for vertebral fractures that is performed on the DEXA machine, may be recommended for older patients, especially if:
- they have lost more than an inch of height.
- have unexplained back pain.
- if a DEXA scan gives borderline readings.
- the DEXA images of the spine suggest a vertebral deformity or fracture.
The VFA test adds only a few minutes to the DEXA procedure.
The dual-energy x-ray absorptiometry (DEXA) scan requires little to no special preparation. You will probably be asked to fill out a questionnaire that will help the doctor determine if you have medical conditions or take certain medications that either increase or decrease your risk of a fracture.
Tell your doctor and the technologist if there is a possibility you are pregnant or if you recently had a barium exam or received an injection of contrast material for a CT or radioisotope scan. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. You should not take calcium supplements for at least 24 hours before your exam.
DEXA scan results
A radiologist, a doctor trained to supervise and interpret radiology examinations, will analyze your dual-energy x-ray absorptiometry (DEXA) scan images. The radiologist will send a signed report to your primary care or referring physician who will discuss the results with you.
Dual-energy x-ray absorptiometry (DEXA) scans are also interpreted by other physicians such as rheumatologists and endocrinologists.
Your DEXA test results will be in the form of two scores:
- T score: This number shows the amount of bone you have compared with a young adult of the same gender with peak bone mass. A T-score of -1 (minus 1) and above is considered normal. A T-score between -1.1 and -2.4 is classified as osteopenia (low bone mass). A T-score of -2.5 and below is defined as osteoporosis. The T-score is used to estimate your risk of developing a fracture and also to determine if treatment is required.
- Z score: This number reflects the amount of bone you have compared with other people in your age group and of the same size and gender. If your Z-score is unusually high or low, it may indicate a need for further medical tests.
Small changes may normally be observed between scans due to differences in positioning and usually are not significant.
What are the limitations of a bone density scan?
- A DEXA test cannot predict who will experience a fracture but can provide a relative risk and it is used to determine whether treatment is required.
- Despite its effectiveness as a method of measuring bone density, DEXA is of limited use in people with a spinal deformity or those who have had previous spinal surgery. The presence of vertebral compression fractures or osteoarthritis may interfere with the accuracy of the test; in such instances, CT scans may be more useful.
- Central DEXA devices are more sensitive and better standardized than peripheral DEXA devices but they are also somewhat more expensive.
- In the central DEXA examination, which measures bone density of the hip and spine, the patient lies on a padded table. An x-ray generator is located below the patient and an imaging device, or detector, is positioned above. To assess the spine, the patient’s legs are supported on a padded box to flatten the pelvis and lower (lumbar) spine. To assess the hip, the patient’s foot is placed in a brace that rotates the hip inward. In both cases, the detector is slowly passed over the area, generating images on a computer monitor. You must hold very still and may need to hold your breath for a few seconds while the technologist takes the x-ray. This helps reduce the possibility of a blurred image. The technologist will walk behind a wall or into the next room to activate the x-ray machine.
- In the peripheral DEXA scan, the finger, hand, forearm or foot is placed in a small device that obtains a bone density reading within a few minutes.
- A test done on a peripheral location, such as the heel or wrist, may help predict the risk of fracture in the spine or hip. These tests are not as helpful in following response to treatment, however, and if they indicate that drug therapy is needed, a baseline central DEXA scan should be obtained.
- Follow-up DEXA exams should be performed at the same institution and ideally with the same machine. Bone density measurements obtained with different DXA equipment cannot be directly compared.
Other testing
An evaluation for secondary causes of bone loss should be considered in a patient with a Z-score ≤ -2.0 or if a cause of secondary bone loss is clinically suspected. Laboratory testing 4 should usually include the following:
- Serum calcium, magnesium, and phosphorus
- 25-Hydroxy vitamin D level
- Liver function tests, including an alkaline phosphatase (hypophosphatasia)
- Intact PTH level (hyperparathyroidism)
- Serum testosterone in men (hypogonadism)
- 24-h urine for calcium and creatinine (hypercalciuria)
Other tests such as thyroid-stimulating hormone or free thyroxine to check for hyperthyroidism, measurements of urinary free cortisol, and blood counts and other tests to rule out cancer, especially myeloma (eg, serum and urine protein electrophoresis), should be considered depending on the clinical presentation.
Patients with weight loss should be screened for GI disorders (eg, malabsorption, celiac disease, inflammatory bowel disease) as well as cancer. Bone biopsy is reserved for unusual cases (eg, young patients with fragility fractures and no apparent cause, patients with chronic kidney disease who may have other bone disorders, patients with persistently very low vitamin D levels suspected of having osteomalacia).
Levels of fasting serum C-telopeptide cross-links (CTX) or urine N-telopeptide cross-links reflect increased bone resorption 4. Although reliability varies for routine clinical use, C-telopeptide cross-links and N-telopeptide cross-links may be helpful in monitoring response to therapy or with the timing of a drug holiday.
Treatment of Osteoporosis
One of the primary goals in the treatment of osteoporosis and other bone diseases is to maintain bone health by preventing bone loss and perhaps even by building new bone. Another goal is to minimize the risk and/or impact of falls, since they are typically the precursor to the most devastating consequence of bone disease: fractures. The best way to realize these goals is to employ a combination of various prevention and treatment strategies.
- The first step in the prevention and treatment of osteoporosis and the prevention of fractures is to build a foundation of nutrition and lifestyle measures that maximize bone health. The diet should not only be adequate in calcium and vitamin D, but should have a healthy balance of other nutrients. A weight-bearing exercise program should be developed. Cigarette smoking and excessive alcohol use must be avoided. In the older individual, at high risk for fractures, the changes in lifestyle would include a plan not only to maximize physical activity, but also to minimize the risk of falls. The use of hip protectors can be considered in some high-risk patients. Diseases that increase the risk of falls by causing visual impairment, postural hypotension (a drop in blood pressure on standing, which leads to dizziness), or poor balance should be treated. Drugs that cause bone loss or increase the risk of falls should be avoided or given at the lowest effective dose.
- The Second Step: The next step is to identify and treat diseases that produce secondary osteoporosis or aggravate primary osteoporosis. These measures are the foundation upon which specific pharmacotherapy is built and should never be forgotten.
- The Third Step: If there is sufficiently high risk of fracture to warrant pharmacotherapy, the patient is usually started on antiresorptives. Anabolic agents are used in individuals in whom antiresorptive therapy is not adequate to prevent bone loss or fractures 159.
Bisphosphonates
For both men and women at increased risk of fracture, the most widely prescribed osteoporosis medications are bisphosphonates. Biophosphonates help reduce your risk of breaks and fractures. Biophosphonates also increase bone density. Biophosphonates come in oral (pill) form or intravenous (IV or injection) form.
Examples of biophosphonates include:
- Alendronate (Binosto, Fosamax). This medicine is used to help prevent and treat osteoporosis. This medicine helps reduce your risk of fractures by decreasing the rate of bone loss. This medicine is available in pill form. Their most common side effect is an upset stomach.
- Ibandronate (Boniva). This medicine helps to slow bone loss and increase bone density. It is available as a pill or injection. You have 2 options for the pill. You can take it daily or monthly. For the injection, your doctor or nurse will give you a shot every 3 months. Side effects may include lower back or side pain, shortness of breath, tightness in your chest, and bloody or cloudy urine.
- Risedronate (Actonel, Atelvia). This medicine is used to help prevent and treat osteoporosis. This medicine helps reduce your risk of fractures by decreasing the rate of bone loss. This medicine is available in pill form. Their most common side effect is an upset stomach.
- Zoledronic acid (Reclast, Zometa). This medicine is given through IV once a year.
Side effects of bisphosphonates include nausea, abdominal pain and heartburn-like symptoms. You may have irritation of the esophagus (the tube that connects your mouth and stomach). These are less likely to occur if the medicine is taken properly. Intravenous forms of bisphosphonates don’t cause stomach upset but can cause fever, headache and muscle aches.
A very rare complication of bisphosphonates is a break or crack in the middle of the thighbone. A second rare complication is delayed healing of the jawbone (osteonecrosis of the jaw). This can occur after an invasive dental procedure, such as removing a tooth.
Some people cannot take biophosphonates. This includes people who have kidney disease or low levels of calcium in their blood, and women who are pregnant or nursing.
Oral bisphosphonates must be taken on an empty stomach with a full (8-oz, 250 mL) glass of water, and the patient must remain upright for at least 30 min (60 min for ibandronate) and not take anything else by mouth during this time period. These drugs are safe to use in patients with a creatinine clearance > 35 mL/min. Bisphosphonates can cause esophageal irritation 4. Esophageal disorders that delay transit time and symptoms of upper GI disorders are relative contraindications to oral bisphosphonates. IV bisphosphonates are indicated if a patient is unable to tolerate or is nonadherent with oral bisphosphonates 4.
Osteonecrosis of the jaw has been associated with use of bisphosphonates; however, this condition is rare in patients taking oral bisphosphonates 160. Current screening and diagnostic tests are unreliable for predicting a patient’s risk of developing the condition 160. Osteonecrosis of the jaw may occur spontaneously or after dental extraction or trauma, radiation therapy to the head and neck (osteoradionecrosis), or high-dose IV bisphosphonate therapy (eg, for cancer treatment). Osteonecrosis of the jaw may be a refractory osteomyelitis rather than true osteonecrosis, particularly when associated with bisphosphonate use. There is no evidence that routine use of oral bisphosphonates for treatment or prevention of osteoporosis increases risk of ONJ. Currently, otherwise appropriate bisphosphonate use should not be discouraged. However, it seems reasonable to do any necessary oral surgery before beginning bisphosphonate therapy and to encourage good oral hygiene while patients are taking bisphosphonates 160. The benefits of reduction of osteoporosis-related fractures far outweigh this small risk.
Long-term bisphosphonate use may also increase the risk of atypical femoral fractures 4. These fractures occur in the mid-shaft of the femur with minimal or no trauma and may be preceded by weeks or months of thigh pain. The fractures may also be bilateral. To minimize fracture incidence, consideration should be given to stopping bisphosphonates (a bisphosphonate holiday) 4 after about:
- 3 to 5 yr of use in patients with osteoporosis (by DEXA scan) but few or no other risk factors for bone loss (3 yr for IV zoledronic acid and 5 yr for oral bisphosphonates)
- 5 to 10 yr of use in patients with osteoporosis (by DEXA scan) and more risk factors
Patients on a bisphosphonate holiday should be closely monitored for a new fracture or accelerated bone loss evident on a DXA scan. During therapy with an antiresorptive drug, such as a bisphosphonate, bone turnover is suppressed as evidenced by low fasting N-telopeptide cross-links (< 40 nmol/L) or C-telopeptide cross-links. These markers may remain low for ≥ 2 yr of a drug holiday.
In untreated patients, an increase in levels of bone turnover markers indicates an increased risk of fracture. However, it is not clear whether levels of bone turnover markers should be used as criteria for when to start or end a drug holiday. The decision to begin or end a drug holiday is complex and should take into account the patient’s risk factors.
Estrogen, especially when started soon after menopause, can help maintain bone density. However, estrogen therapy can increase the risk of breast cancer and blood clots, which can cause strokes. Therefore, estrogen is typically used for bone health in younger women or in women whose menopausal symptoms also require treatment.
Raloxifene (Evista) is a selective estrogen receptor modulator (SERM) that mimic estrogen’s beneficial effects on bone density in postmenopausal women, without some of the risks associated with estrogen. Taking Raloxifene can reduce the risk of some types of breast cancer. Hot flashes are a possible side effect. Raloxifene also may increase your risk of blood clots.
In men, osteoporosis might be linked with a gradual age-related decline in testosterone levels. Testosterone replacement therapy can help improve symptoms of low testosterone, but osteoporosis medications have been better studied in men to treat osteoporosis and thus are recommended alone or in addition to testosterone.
Calcitonin is a hormone that helps slow down bone loss. Calcitonin is available as an injection or nasal spray. Side effects of the injection include diarrhea, stomach pain, nausea, and vomiting. Side effects of the nose spray include headache and irritation of your nose lining.
Bone-building medications
If you have severe osteoporosis or if the more common treatments for osteoporosis don’t work well enough, your doctor might suggest trying:
- Teriparatide (Bonsity, Forteo). This powerful drug is similar to parathyroid hormone (PTH) and stimulates new bone growth. It’s given by daily injection under the skin for up to two years.
- Abaloparatide (Tymlos) is another drug similar to parathyroid hormone (PTH). This drug can be taken for only two years.
- Romosozumab (Evenity). This is the newest bone-building medication to treat osteoporosis. It is given as an injection every month at your doctor’s office and is limited to one year of treatment.
After you stop taking any of these bone-building medications, you generally will need to take another osteoporosis drug to maintain the new bone growth.
Denosumab
Denosumab (Prolia, Xgeva) is a fully humanized monoclonal antibody against RANKL (receptor activator of nuclear factor kappa-B ligand) and reduces bone resorption by osteoclasts 4. A RANK ligand (RANKL) inhibitor is approved for postmenopausal women with osteoporosis and men who are at high risk for fracture. Denosumab is given as a subcutaneous injection of 60 mg once every 6 months.
Denosumab (Prolia, Xgeva) is used when other drugs don’t work or if you can’t tolerate other treatment options. Denosumab increases your bone density. Denosumab can be used by both women and men 161, 162, 163, 164. Denosumab has been shown to reduce the incidence of vertebral, non-vertebral and hip fractures in postmenopausal women with osteoporosis 165 and safety and efficacy are maintained over 10 years of treatment 164.
Denosumab side effects can include lower calcium levels (hypocalcemia), skin infection, predominantly cellulitis, eczema, flatulence or pain in the arms and legs. Rare adverse effects of denosumab include osteonecrosis of the jaw and atypical femoral fractures.
Denosumab is contraindicated in patients with hypocalcemia (low blood calcium), with hypersensitivity to any of the constituents of the formulation and in pregnant women 4. Denosumab is also contraindicated in those under 18 years of age. Hypocalcemia, as a side-effect of denosumab treatment, increases with the degree of kidney impairment; patients should be advised to report symptoms of hypocalcemia. Pre-existing hypocalcemia must be investigated and, where due to vitamin D deficiency, treated with vitamin D (e.g., 100,000 to 300,000 IU orally as a loading dose in divided doses) before denosumab treatment is initiated 166. Adequate intake of calcium and vitamin D is important in all patients, especially those with severe kidney impairment. The US Food and Drug Administration (FDA) states all patients should have calcium level checked prior to each dose 167. In patients predisposed to hypocalcemia (e.g., patients with a creatinine clearance < 35 ml/min), serum calcium levels should also be checked within 2 weeks after the initial dose 168.
Similar to bisphosphonates, denosumab has the same rare complication of causing breaks or cracks in the middle of the thighbone and osteonecrosis of the jaw. If you take denosumab, you might need to continue to do so indefinitely. Recent research indicates there could be a high risk of spinal column fractures after stopping the drug.
Denosumab may be helpful in patients not tolerant of or unresponsive to other therapies or in patients with impaired renal function.
Denosumab cessation leads to rapid reductions in bone mass density (BMD) and elevations in bone turnover to levels above those seen before treatment initiation 169. Patients who discontinue denosumab have an increased risk of sustaining multiple vertebral fractures. In a post hoc analysis of the FREEDOM study and its extension, women discontinuing denosumab had an increased rate of vertebral fracture over an average of 3–6 months since the last denosumab injection was due. Of those patients who sustained vertebral fractures, 60.7% sustained multiple fractures compared to 38.7% of those discontinuing placebo 170, 171. The increase in vertebral fracture risk following cessation of denosumab therapy emphasises the need to consider continued treatment with an alternative anti-resorptive drug following denosumab withdrawal. An intravenous infusion of 5 mg of zoledronate, 6 months after the last denosumab injection, reduces subsequent bone loss 172, 173, 174, 175, although this effect is not seen in all patients and may not be maintained beyond one year, particularly in those who have had more than 3 years of denosumab treatment 176. Monitoring bone turnover markers at 3 and 6 months post zoledronate infusion can help guide the timing of subsequent infusions. Where bone turnover markers are not available, a second infusion of zoledronate after 6 months has been proposed 177. Oral alendronate 70 mg once weekly, was shown to maintain BMD for 12 months in most patients following one year of denosumab therapy, although significant bone loss occurred in a minority 178. Given the difficulties in stopping denosumab treatment, particularly careful consideration is needed before starting denosumab in younger postmenopausal women, and men 166.
Compared with bisphosphonates, denosumab produces similar or better bone density results and reduces the chance of all types of fractures 165, 164.
Calcitriol
Calcitriol (1,25-dihydroxyvitamin D3) is the active form of vitamin D and is approved for the treatment of established postmenopausal osteoporosis in an oral dose of 0.25 mcg twice daily 166. Calcitriol (1,25-dihydroxyvitamin D3) acts mainly by inhibiting bone resorption 53. Calcitriol (1,25-dihydroxyvitamin D3) has been shown to reduce vertebral fracture risk in postmenopausal women with osteoporosis but effects on non-vertebral and hip fractures have not been demonstrated 179. Calcitriol (1,25-dihydroxyvitamin D3) is contraindicated in patients with hypercalcemia or with metastatic calcification. Because calcitriol can cause hypercalcemia and/or hypercalciuria, serum calcium and creatinine levels should be monitored at 1, 3, and 6 months after starting treatment and at 6 monthly intervals thereafter 166.
Treatment of Osteoporotic Fractures
For all osteoporotic fractures, the consistent goal is for patients to regain their pre-fracture level of function. All patients with low-trauma fractures should be evaluated for other bone diseases, secondary causes of bone loss and they should also be evaluated with respect to the need for additional preventive measures (calcium, vitamin D, exercise, fall prevention) and for drug therapy. What follows is a review of the various available treatments for specific types of osteoporotic-related fractures, including fractures of the hip, spine, and wrist.
Hip fractures
Surgery is the most common treatment for individuals who suffer a hip fracture. Virtually all intertrochanteric fractures (those in the major part of the hip) and most femoral neck fractures (those in the neck section of the hip) are surgically stabilized with the use of internal metal devices. A large percentage of displaced (unconnected) femoral neck fractures are treated with partial or total replacement of the hip because of the significant risk of healing complications 180.
Spine fractures
Spine fractures usually occur in the middle or lower section of the back as a result of minor strain, such as lifting a grocery bag. Some patients develop fractures without any identifiable trauma. Spine fractures due to osteoporosis result in the progressive collapse of bones in these areas, which typically cause increasing levels of spinal deformity and pain. However, about two-thirds of spine fractures go undiagnosed because there is little or no pain, or the pain is attributed to one of the many other causes of back pain 181. Similarly, other signs of a spine fracture, including deformities and height loss, are often accepted as a normal part of aging and thus not investigated further.
It is not unusual for patients to have prolonged pain and disability following spine fractures. Treatment of spine fractures typically focuses on pain control and progressive increases in levels of mobilization. Back braces are of limited benefit. More recently, procedures have been developed to treat patients who have prolonged pain. Vertebroplasty is a technique in which acrylic cement (or orthopedic cement mixture) is injected into the spine bone for the purpose of stabilizing the fracture 182. Kyphoplasty involves using a balloon to re-expand the collapsed bone and then filling the cavity with bone cement. This procedure has the potential to stabilize the fracture, prevent further collapse, and restore some degree of height to the bone 183. Both vertebroplasty and kyphoplasty have been shown to provide effective pain relief and stabilization of the fracture 182, 183. Although complications from these procedures have been infrequent, they can be significant if the bone cement leaks out into the blood stream or into the spinal canal, causing nerve damage. Unfortunately, the potential benefit of these two procedures has not yet been accurately assessed in randomised double blind clinical trials, where they might be compared to each other and to nonsurgical management.
Wrist fractures
Wrist fractures commonly occur as a result of osteoporosis. They include fractures of the radius and/or ulna (the two long bones in the forearm), as well as of the small bones of the wrist. The term Colles’ fractures refers to fractures of the end of the radius, which has a large amount of trabecular bone. Wrist fractures are usually treated by either surgical repositioning and casting or placement of an external fixation device to prevent further fracture. Depending on the type of fracture, one of the following will be used to immobilize the wrist until an x-ray shows evidence of healing (usually in 4–8 weeks): a brace or splint, cast, external fixation, internal fixation, or combined external and internal fixation. Although most patients return to an adequate level of functioning, many do experience some loss of range of motion of the wrist.
Other fractures
Osteoporotic fractures occur in other areas of the body, including the upper arm, thigh, shin, collar bone, and ribs. These fractures are treated by a variety of surgical and non-surgical measures.
Exercises for those with osteoporotic fractures
Individuals who have already experienced osteoporotic fractures should avoid certain types of physical activities and exercises. For example, those who have had vertebral fractures may need to avoid activities that flex the spine.
Spine fractures
Walking should be encouraged even in frail individuals. Exercising in a way that safely challenges balance is also important for rehabilitation of spinal fracture patients, but resistance/strengthening exercises should not be initiated or resumed until the fracture has healed (in approximately 8 to 12 weeks). Since the risk of another spine fracture is high in patients who have had fractures, patients should be instructed to avoid exercises and activities that put high loads on the bones of the spine, such as flexing or rotating the spine (sit ups, toe touches). Exercises and activities done with good spine alignment and low to moderate amounts of weight should be gradually increased, with the goals of regaining muscle strength and promoting maintenance of bone mass. Abdominal strengthening (by tightening the muscles in the abdomen or belly without moving the back) is safe and important to reducing loads on the low back. Spinal extension exercise (i.e., stretching backwards) within a moderate range is safe and can improve hyperkyphosis (a spine that is bent excessively forward) and may help prevent new spine fractures 184.
Wrist fractures
Rehabilitation of the wrist after the cast, brace, or surgical metal is removed requires about 3 months. During healing of a wrist fracture, all of the following are important: arm elevation; early mobilization of the hand, elbow, and shoulder; and control of swelling. Progressive exercises, taught by either a physical or occupational therapist, typically include active and passive range of motion and resistance and grip strengthening, such as squeezing a ball 185. A small number of patients suffer from sympathetic dystrophy (complex regional pain syndrome) after a wrist fracture, resulting in swelling, weakness, and chronic pain in the wrist.
The foundation of a good physical activity regimen involves at least 30 minutes (adults) or 60 minutes (children) of moderate physical activity every day. This regimen can and should involve a variety of activities. Some can be routine activities like walking or gardening. Others may occur more infrequently and differ from day to day and week to week, such as dancing, aerobic classes, biking, swimming, tennis, golf, or hiking. However, it is clear from the evidence that physical activity to specifically benefit bone health should involve loading (stressing) the skeleton. As a result, weight-bearing activities such as walking should be included in an optimal physical activity regimen to benefit the musculoskeletal system. Moreover, the evidence suggests that the most beneficial physical activity regimens for bone health include strength-training or resistance-training activities. These activities place levels of loading on bone that are beyond those seen in everyday activities; examples include jumping for the lower limbs and weight lifting or resistance training for the lower and upper skeleton. Finally, while a focus on activities that build or maintain bone strength is appropriate and necessary, many older individuals will remain at high risk of fracture. For these individuals, balance training can provide the added benefit of helping to prevent potentially injurious falls.
Osteoporosis prognosis
If osteoporosis is detected early and treated, the outcomes are good 186. However, if osteoporosis remains untreated, it can lead to chronic pain and fractures. The risk of osteoporosis can be decreased through using bisphosphonates, exercise, and a diet rich in calcium and vitamin D (and may be vitamin K2). Unfortunately, bisphosphonates are not only expensive but have serious side effects. In addition, whether they can reduce fractures is still being debated. Overall, postmenopausal women remain at high risk for a hip fracture, which often results in prolonged recovery and nursing home placement.
Vertebral fractures are also common and can lead to kyphosis, chronic pain, respiratory compromise, and a high risk for developing pneumonia. Most patients lose their ability to live independently as they are not able to function.
Osteoporosis summary
Osteoporosis is a progressive metabolic bone disease that decreases bone density (bone mass per unit volume), with deterioration of bone structure. Nine percent of adults over age 50 years had osteoporosis at either the femur neck or lumbar spine and roughly one-half had low bone mass at either of these two skeletal sites. Having osteoporosis raises the risk of experiencing fractures. Skeletal weakness leads to fractures with minor or inapparent trauma, particularly in the thoracic and lumbar spine, wrist, and hip (called fragility fractures). Diagnosis is by dual-energy x-ray absorptiometry (DEXA scan) or by confirmation of a fragility fracture.
The prevalence of osteoporosis or low bone mass at either the femur neck or lumbar spine was not the same as the prevalence of these conditions when the two skeletal sites were considered separately because some individuals had these conditions at one of the skeletal sites but not the other. The prevalence of osteoporosis or low bone mass differed by age, sex, and race and ethnicity. The prevalence was higher in women and increased with age. Differences by race and ethnicity varied depending on sex and skeletal status category, but when compared with non-Hispanic white persons, Mexican-American persons, and persons of other races tended to be at higher risk, and non-Hispanic black persons tended to be at lower risk of either osteoporosis or low bone mass at the femur neck or lumbar spine.
Prevention and treatment involve risk factor modification, calcium and vitamin D supplements, exercises to maximize bone and muscle strength, improve balance, and minimize the risk of falls, and drug therapy to preserve bone mass or stimulate new bone formation.
Recommendations
- Diet must include adequate amounts of total calcium intake (1000 mg/day for men 50–70; 1200 mg/day for women 51 and older and men 71 and older), incorporating dietary supplements if diet is insufficient.
- Vitamin D intake (800–1000 IU/day), including supplements if necessary for individuals age 50 and older.
- Regular weight-bearing and muscle-strengthening exercise to improve agility, strength, posture, and balance; maintain or improve bone strength; and reduce the risk of falls and fractures. Since continued physical activity provides a positive stimulus for bone, muscle, and other aspects of health, a lifelong commitment to physical activity and exercise is critical.
- Assess risk factors for falls and offer appropriate modifications (e.g., home safety assessment, balance training exercises, correction of vitamin D insufficiency, avoidance of central nervous system depressant medications, careful monitoring of antihypertensive medication, and visual correction when needed).
- Cessation of tobacco smoking and avoidance of excessive alcohol intake.
There is good evidence that proper nutrition and lifestyle can promote bone health and that medications can slow bone loss or even build new bone. However, there is still no “cure” for osteoporosis.
- Kanis JA, McCloskey EV, Johansson H, et al. A reference standard for the description of osteoporosis. Bone 42(4) 67–75. 2008.[↩]
- National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. National Osteoporosis Foundation, Washington, DC. 1–36. 2008.[↩]
- National Center for Biotechnology Information, U.S. National Library of Medicine. – Osteoporosis – https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024680/[↩][↩]
- Merck Sharp & Dohme Corp., Merck Manual. Osteoporosis. https://www.merckmanuals.com/professional/musculoskeletal-and-connective-tissue-disorders/osteoporosis/osteoporosis[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- DEXA for Osteoporosis. https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/cw-osteoporosis.html[↩][↩][↩][↩]
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. Bone Basics. https://www.niams.nih.gov/Health_Info/Bone/Bone_Health/default.asp[↩][↩]
- Khosla S, Riggs BL. Pathophysiology of age-related bone loss and osteoporosis. Endocrinol Metab Clin N Am. 2005;34:1015–1030. doi: 10.1016/j.ecl.2005.07.009. https://www.ncbi.nlm.nih.gov/pubmed/16310636[↩]
- Osteoporos Int. 2014; 25(10): 2359–2381. – Clinician’s Guide to Prevention and Treatment of Osteoporosis – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4176573/[↩]
- National Institute of Health, Osteoporosis and Related Bone Diseases ~ National Resource Center. Osteoporosis Basics . https://www.niams.nih.gov/Health_Info/Bone/Osteoporosis/osteoporosis_hoh.asp[↩]
- National Center for Biotechnology Information, U.S. National Library of Medicine. – Bone Health and Osteoporosis: A Report of the Surgeon General. – https://www.ncbi.nlm.nih.gov/books/NBK45515/[↩]
- National Osteoporosis Foundation. Osteoporosis: What is it?. Washington, DC: National Osteoporosis Foundation; [Cited 2004 Mar 1]. Available from: http://www.nof.org/osteoporosis/index.htm.[↩][↩]
- Office on Women’s Health, U.S. Department of Health and Human Services. Osteoporosis. https://www.womenshealth.gov/a-z-topics/osteoporosis[↩]
- Reviews in Endocrine and Metabolic Disorders, December 2010, Volume 11, Issue 4, pp 237–251. Diagnosis and treatment of osteopenia. https://link.springer.com/article/10.1007%2Fs11154-010-9154-0[↩][↩]
- WHO Scientific Group on Assessment of Osteoporosis at Primary Health Care Level 2004. http://www.who.int/chp/topics/Osteoporosis.pdf[↩]
- AIDSInfo, U.S. Department of Health and Human Services. https://aidsinfo.nih.gov/understanding-hiv-aids/glossary/537/osteopenia [↩]
- Bone mineral density thresholds for pharmacological intervention to prevent fractures. Siris ES, Chen YT, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE, Berger ML. Arch Intern Med. 2004 May 24; 164(10):1108-12. https://www.ncbi.nlm.nih.gov/pubmed/15159268/[↩][↩][↩]
- Zoledronic acid and clinical fractures and mortality after hip fracture. Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S, HORIZON Recurrent Fracture Trial. N Engl J Med. 2007 Nov 1; 357(18):1799-809. https://www.ncbi.nlm.nih.gov/pubmed/17878149/[↩]
- Bone and fall-related fracture risks in women and men with a recent clinical fracture. van Helden S, van Geel AC, Geusens PP, Kessels A, Nieuwenhuijzen Kruseman AC, Brink PR. J Bone Joint Surg Am. 2008 Feb; 90(2):241-8. https://www.ncbi.nlm.nih.gov/pubmed/18245581/[↩]
- Rev Endocr Metab Disord. 2012 Sep; 13(3): 209–223. Published online 2011 Jun 28. doi: 10.1007/s11154-011-9187-z. Treatment of osteopenia. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3411311/[↩][↩][↩]
- Centers for Disease Control and Prevention. – Osteoporosis or Low Bone Mass at the Femur Neck or Lumbar Spine in Older Adults: United States, 2005–2008 – https://www.cdc.gov/nchs/data/databriefs/db93.htm[↩]
- CDC/NCHS, National Health and Nutrition Examination Survey, 2005–2008.[↩]
- Harvard University, Harvard School of Public Health. Calcium: What’s Best for Your Bones and Health ? https://www.hsph.harvard.edu/nutritionsource/calcium-full-story/[↩][↩][↩]
- Committee to Review Dietary Reference Intakes for Vitamin D and Calcium, Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Optimal calcium intake. NIH Consens Statement. 1994 Jun 6-8;12(4):1-31.[↩]
- Heaney RP, Recker RR, Stegman MR, Moy AJ. Calcium absorption in women: relationships to calcium intake, estrogen status, and age. J Bone Miner Res. 1989 Aug;4(4):469-75. doi: 10.1002/jbmr.5650040404[↩]
- Weaver CM, Heaney RP. Isotopic exchange of ingested calcium between labeled sources. Evidence that ingested calcium does not form a common absorptive pool. Calcif Tissue Int. 1991 Oct;49(4):244-7. doi: 10.1007/BF02556212[↩]
- Weaver CM, Heaney RP, Martin BR, Fitzsimmons ML. Human calcium absorption from whole-wheat products. J Nutr. 1991 Nov;121(11):1769-75. doi: 10.1093/jn/121.11.1769[↩]
- Heaney RP. Bone mass, nutrition, and other lifestyle factors. Nutr Rev. 1996 Apr;54(4 Pt 2):S3-10. doi: 10.1111/j.1753-4887.1996.tb03891.x[↩][↩][↩]
- Kerstetter JE, O’Brien KO, Caseria DM, Wall DE, Insogna KL. The impact of dietary protein on calcium absorption and kinetic measures of bone turnover in women. J Clin Endocrinol Metab. 2005 Jan;90(1):26-31. doi: 10.1210/jc.2004-0179[↩]
- Barrett-Connor E, Chang JC, Edelstein SL. Coffee-associated osteoporosis offset by daily milk consumption. The Rancho Bernardo Study. JAMA. 1994 Jan 26;271(4):280-3. doi: 10.1001/jama.1994.03510280042030[↩]
- Massey LK, Whiting SJ. Caffeine, urinary calcium, calcium metabolism and bone. J Nutr. 1993 Sep;123(9):1611-4. doi: 10.1093/jn/123.9.1611[↩]
- Hirsch PE, Peng TC. Effects of alcohol on calcium homeostasis and bone. In: Anderson J, Garner S, eds. Calcium and Phosphorus in Health and Disease. Boca Raton, FL: CRC Press, 1996:289-300.[↩]
- U.S. Department of Agriculture. Results from the United States Department of Agriculture’s 1994-96 Continuing Survey of Food Intakes by Individuals/Diet and Health Knowledge Survey, 1994-96.[↩]
- Heaney RP, Rafferty K. Carbonated beverages and urinary calcium excretion. Am J Clin Nutr. 2001 Sep;74(3):343-7. doi: 10.1093/ajcn/74.3.343[↩]
- Fenton TR, Eliasziw M, Lyon AW, Tough SC, Hanley DA. Meta-analysis of the quantity of calcium excretion associated with the net acid excretion of the modern diet under the acid-ash diet hypothesis. Am J Clin Nutr. 2008 Oct;88(4):1159-66. doi: 10.1093/ajcn/88.4.1159[↩]
- National Center for Biotechnology Information, U.S. National Library of Medicine – Bone Health and Osteoporosis: A Report of the Surgeon General.- https://www.ncbi.nlm.nih.gov/books/NBK45523/[↩]
- National Center for Biotechnology Information, U.S. National Library of Medicine. – Prevention and Treatment for Those Who Have Bone Diseases – https://www.ncbi.nlm.nih.gov/books/NBK45501/[↩]
- Office on Women’s Health, the U.S. Department of Health and Human Services. Osteoporosis. https://www.womenshealth.gov/a-z-topics/osteoporosis[↩]
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.[↩][↩]
- Jackson RD, LaCroix AZ, Gass M, Wallace RB, et al. Women’s Health Initiative Investigators. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006 Feb 16;354(7):669-83. doi: 10.1056/NEJMoa055218. Erratum in: N Engl J Med. 2006 Mar 9;354(10):1102.[↩]
- Wallace RB, Wactawski-Wende J, O’Sullivan MJ, Larson JC, Cochrane B, Gass M, Masaki K. Urinary tract stone occurrence in the Women’s Health Initiative (WHI) randomized clinical trial of calcium and vitamin D supplements. Am J Clin Nutr. 2011 Jul;94(1):270-7. doi: 10.3945/ajcn.110.003350[↩]
- Candelas G, Martinez-Lopez JA, Rosario MP, Carmona L, Loza E. Calcium supplementation and kidney stone risk in osteoporosis: a systematic literature review. Clin Exp Rheumatol. 2012 Nov-Dec;30(6):954-61. https://www.clinexprheumatol.org/abstract.asp?a=5491[↩]
- Kahwati LC, Weber RP, Pan H, Gourlay M, LeBlanc E, Coker-Schwimmer M, Viswanathan M. Vitamin D, Calcium, or Combined Supplementation for the Primary Prevention of Fractures in Community-Dwelling Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018 Apr 17;319(15):1600-1612. doi: 10.1001/jama.2017.21640[↩]
- Calcium. https://ods.od.nih.gov/factsheets/Calcium-Consumer[↩]
- The USDA Food Composition Databases. Calcium Content. https://ods.od.nih.gov/pubs/usdandb/Calcium-Content.pdf[↩]
- The USDA Food Composition Databases. Foods Calcium Content. https://ods.od.nih.gov/pubs/usdandb/Calcium-Food.pdf[↩]
- Calcium. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional[↩]
- The National Institute of Health, Office of Dietary Supplements. Calcium. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/ [↩]
- Straub DA. Calcium supplementation in clinical practice: a review of forms, doses, and indications. Nutr Clin Pract. 2007;22:286-96. https://www.ncbi.nlm.nih.gov/pubmed/17507729?dopt=Abstract[↩]
- Andon MB, Peacock M, Kanerva RL, De Castro JAS. Calcium absorption from apple and orange juice fortified with calcium citrate malate (CCM). J Am Coll Nutr 1996;15:313-6. https://www.ncbi.nlm.nih.gov/pubmed/8935449?dopt=Abstract[↩]
- Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington (DC): National Academy Press; 1997.[↩]
- Heaney RP, Weaver CM. Calcium and vitamin D. Endocrinol Metab Clin North Am. 2003 Mar;32(1):181–94. vii–viii. Review.[↩]
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.[↩][↩]
- Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, DC: National Academy Press; 1997. p. 432.[↩][↩]
- Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared to 2000–2004. Am J Clin Nutr. 2008;88(6):1519–1527. doi: 10.3945/ajcn.2008.26182. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2745830/[↩]
- Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690–693. https://www.ncbi.nlm.nih.gov/pubmed/10966885[↩]
- Pettifor JM. Nutritional and drug-induced rickets and osteomalacia. In: Favus MJ, editor. Primer on the metabolic bone diseases and disorders of mineral metabolism. 5. Washington, DC: American Society for Bone and Mineral Research; 2003. pp. 399–407. [↩]
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010[↩][↩][↩][↩][↩]
- U.S. Department of Agriculture, Agricultural Research Service. 2011. USDA National Nutrient Database for Standard Reference, Release 24. Nutrient Data Laboratory Home Page. https://www.ars.usda.gov/northeast-area/beltsville-md/beltsville-human-nutrition-research-center/nutrient-data-laboratory/[↩]
- Ovesen L, Brot C, Jakobsen J. Food contents and biological activity of 25-hydroxyvitamin D: a vitamin D metabolite to be reckoned with? Ann Nutr Metab. 2003;47(3-4):107-13. doi: 10.1159/000070031[↩]
- Roseland JM, Phillips KM, Patterson KY, Pehrsson PR, Taylor CL. Vitamin D in foods: An evolution of knowledge. Pages 41-78 in Feldman D, Pike JW, Bouillon R, Giovannucci E, Goltzman D, Hewison M, eds. Vitamin D, Volume 2: Health, Disease and Therapeutics, Fourth Edition. Elsevier, 2018.[↩][↩]
- U.S. Food and Drug Administration. Food additives permitted for direct addition to food for human consumption; vitamin D2 mushroom powder. Federal Register 2020;85:41916-20.[↩]
- Borel P, Caillaud D, Cano NJ. Vitamin D bioavailability: state of the art. Crit Rev Food Sci Nutr. 2015;55(9):1193-205. doi: 10.1080/10408398.2012.688897[↩]
- Taylor, C. L., Patterson, K. Y., Roseland, J. M., Wise, S. A., Merkel, J. M., Pehrsson, P. R., & Yetley, E. A. (2014). Including food 25-hydroxyvitamin D in intake estimates may reduce the discrepancy between dietary and serum measures of vitamin D status. The Journal of nutrition, 144(5), 654–659. https://doi.org/10.3945/jn.113.189811[↩]
- Calvo MS, Whiting SJ, Barton CN. Vitamin D fortification in the United States and Canada: current status and data needs. Am J Clin Nutr. 2004 Dec;80(6 Suppl):1710S-6S. doi: 10.1093/ajcn/80.6.1710S[↩]
- Yetley EA. Assessing the vitamin D status of the US population. Am J Clin Nutr. 2008 Aug;88(2):558S-564S. doi: 10.1093/ajcn/88.2.558S[↩]
- Vitamin D for Milk and Milk Alternatives. https://www.fda.gov/food/food-additives-petitions/vitamin-d-milk-and-milk-alternatives[↩]
- Food Labeling: Revision of the Nutrition and Supplement Facts Labels. https://www.federalregister.gov/documents/2016/05/27/2016-11867/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels[↩]
- U.S. Department of Agriculture, Agricultural Research Service. FoodData Central. https://fdc.nal.usda.gov/index.html[↩]
- Whiting SJ, Healey A, Psiuk S, Mirwald R, Kowalski K, Bailey DA. Relationship between carbonated and other low nutrient dense beverages and bone mineral content of adolescents. Nutr Res. 2001 Aug;21 (8):1107–15.[↩]
- Fitzpatrick L, Heaney RP. Got soda. J Bone Miner Res. 2003 Sep;18(9):1570–2. https://www.ncbi.nlm.nih.gov/pubmed/12968665[↩]
- Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, DC: National Academy Press; 1997. p. 432. [↩]
- Institute of Medicine. Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington, DC: National Academy Press; 2000. p. 800.[↩]
- IOM 1997 Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, DC: National Academy Press; 1997. p. 432.[↩]
- Hirota, Yoshihisa & Suhara, Yoshitomo. (2019). New Aspects of Vitamin K Research with Synthetic Ligands: Transcriptional Activity via SXR and Neural Differentiation Activity. International Journal of Molecular Sciences. 2019, 20(12), 3006; https://doi.org/10.3390/ijms20123006[↩]
- Fusaro M, Cianciolo G, Brandi ML, Ferrari S, Nickolas TL, Tripepi G, Plebani M, Zaninotto M, Iervasi G, La Manna G, Gallieni M, Vettor R, Aghi A, Gasperoni L, Giannini S, Sella S, M Cheung A. Vitamin K and Osteoporosis. Nutrients. 2020 Nov 25;12(12):3625. doi: 10.3390/nu12123625[↩]
- Fusaro M., Mereu M.C., Aghi A., Iervasi G., Gallieni M. Vitamin K and bone. Clin. Cases Miner. Bone Metab. 2017;14:200–206. doi: 10.11138/ccmbm/2017.14.1.200[↩]
- Bouckaert J.H., Said A.H. Fracture healing by vitamin K. Nature. 1960;185:849. doi: 10.1038/185849a0[↩]
- Suttie JW. Vitamin K. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:851-60.[↩][↩][↩]
- Booth S. L. (2012). Vitamin K: food composition and dietary intakes. Food & nutrition research, 56, 10.3402/fnr.v56i0.5505. https://doi.org/10.3402/fnr.v56i0.5505[↩][↩][↩][↩][↩]
- Booth SL, Tucker KL, Chen H, Hannan MT, Gagnon DR, Cupples LA, Wilson PW, Ordovas J, Schaefer EJ, Dawson-Hughes B, Kiel DP. Dietary vitamin K intakes are associated with hip fracture but not with bone mineral density in elderly men and women. Am J Clin Nutr. 2000 May;71(5):1201-8. doi: 10.1093/ajcn/71.5.1201[↩]
- Thane CW, Paul AA, Bates CJ, Bolton-Smith C, Prentice A, Shearer MJ. Intake and sources of phylloquinone (vitamin K1): variation with socio-demographic and lifestyle factors in a national sample of British elderly people. Br J Nutr. 2002 Jun;87(6):605-13. doi: 10.1079/BJNBJN2002583[↩]
- Ferland G. Vitamin K. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:230-47.[↩]
- National Institute of Health, Office of Dietary Supplements. Vitamin K. https://ods.od.nih.gov/factsheets/VitaminK-HealthProfessional/[↩]
- Elder SJ, Haytowitz DB, Howe J, Peterson JW, Booth SL. Vitamin k contents of meat, dairy, and fast food in the u.s. Diet. J Agric Food Chem. 2006 Jan 25;54(2):463-7. doi: 10.1021/jf052400h[↩][↩]
- Walther, B., Karl, J. P., Booth, S. L., & Boyaval, P. (2013). Menaquinones, bacteria, and the food supply: the relevance of dairy and fermented food products to vitamin K requirements. Advances in nutrition (Bethesda, Md.), 4(4), 463–473. https://doi.org/10.3945/an.113.003855[↩][↩]
- Okano T, Shimomura Y, Yamane M, Suhara Y, Kamao M, Sugiura M, Nakagawa K. Conversion of phylloquinone (Vitamin K1) into menaquinone-4 (Vitamin K2) in mice: two possible routes for menaquinone-4 accumulation in cerebra of mice. J Biol Chem. 2008 Apr 25;283(17):11270-9. doi: 10.1074/jbc.M702971200[↩]
- Wells HF, Buzby JC. Dietary assessment of major trends in U.S. food consumption, 1970–2005. Economic Information Bulletin No (EIB-33) p 27, March 2008.[↩]
- Gast GC, de Roos NM, Sluijs I, Bots ML, Beulens JW, Geleijnse JM, Witteman JC, Grobbee DE, Peeters PH, van der Schouw YT. A high menaquinone intake reduces the incidence of coronary heart disease. Nutr Metab Cardiovasc Dis. 2009 Sep;19(7):504-10. doi: 10.1016/j.numecd.2008.10.004[↩]
- Suttie JW. Vitamin K. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:305-16.[↩]
- Conversion of dietary phylloquinone to tissue menaquinone-4 in rats is not dependent on gut bacteria. Davidson RT, Foley AL, Engelke JA, Suttie JW. J Nutr. 1998 Feb; 128(2):220-3. https://www.ncbi.nlm.nih.gov/pubmed/9446847/[↩]
- Menadione is a metabolite of oral vitamin K. Thijssen HH, Vervoort LM, Schurgers LJ, Shearer MJ. Br J Nutr. 2006 Feb; 95(2):260-6. https://www.ncbi.nlm.nih.gov/pubmed/16469140/[↩]
- Vitamin K contents of meat, dairy, and fast food in the U.S. Diet. Elder SJ, Haytowitz DB, Howe J, Peterson JW, Booth SL. J Agric Food Chem. 2006 Jan 25; 54(2):463-7. https://www.ncbi.nlm.nih.gov/pubmed/16417305/[↩]
- Schurgers LJ. Vitamin K: key vitamin in controlling vascular calcification in chronic kidney disease. Kidney Int. 2013 May;83(5):782-4. doi: 10.1038/ki.2013.26[↩]
- Fusaro M., Gallieni M., Rizzo M.A., Stucchi A., Delanaye P., Cavalier E., Moysés R.M.A., Jorgetti V., Iervasi G., Giannini S., et al. Vitamin K plasma levels determination in human health. Clin. Chem. Lab. Med. 2017;55:789–799. doi: 10.1515/cclm-2016-0783[↩]
- Torbergsen A.C., Watne L.O., Wyller T.B., Frihagen F., Strømsøe K., Bøhmer T., Mowe M. Vitamin PK and 25(OH)D are independently and synergistically associated with a risk for hip fracture in an elderly population: A case control study. Clin. Nutr. 2015;34:101–106. doi: 10.1016/j.clnu.2014.01.016[↩]
- Finnes T.E., Lofthus C.M., Meyer H.E., Søgaard A.J., Tell G.S., Apalset E.M., Gjesdal C., Grimnes G., Schei B., Blomhoff R., et al. A combination of low serum concentrations of vitamins PK and D is associated with increased risk of hip fractures in elderly Norwegians: A NOREPOS study. Osteoporos. Int. 2016;27:1645–1652. doi: 10.1007/s00198-015-3435-0[↩]
- Yaegashi Y., Onoda T., Tanno K., Kuribayashi T., Sakata K., Orimo H. Association of hip fracture incidence and intake of calcium, magnesium, vitamin D, and vitamin K. Eur. J. Epidemiol. 2008;23:219–225. doi: 10.1007/s10654-008-9225-7[↩]
- Gundberg CM, Lian JB, Booth SL. Vitamin K-dependent carboxylation of osteocalcin: friend or foe? Adv Nutr 2012;3:149-57. https://www.ncbi.nlm.nih.gov/pubmed/22516722?dopt=Abstract[↩][↩]
- Yaegashi Y, Onoda T, Tanno K, Kuribayashi T, Sakata K, Orimo H. Association of hip fracture incidence and intake of calcium, magnesium, vitamin D, and vitamin K. Eur J Epidemiol 2008;23:219-25. https://www.ncbi.nlm.nih.gov/pubmed/18214692?dopt=Abstract[↩]
- Rejnmark L, Vestergaard P, Charles P, Hermann AP, Brot C, Eiken P, et al. No effect of vitamin K1 intake on bone mineral density and fracture risk in perimenopausal women. Osteoporos Int 2006;17:1122-32. https://www.ncbi.nlm.nih.gov/pubmed/16683180?dopt=Abstract[↩]
- Feskanich D, Weber P, Willett WC, Rockett H, Booth SL, Colditz GA. Vitamin K intake and hip fractures in women: a prospective study. Am J Clin Nutr 1999;69:74-9. https://www.ncbi.nlm.nih.gov/pubmed/9925126?dopt=Abstract[↩]
- Booth SL, Broe KE, Gagnon DR, Tucker KL, Hannan MT, McLean RR, et al. Vitamin K intake and bone mineral density in women and men. Am J Clin Nutr 2003;77:512-6. https://www.ncbi.nlm.nih.gov/pubmed/12540415?dopt=Abstract[↩]
- Booth SL, Tucker KL, Chen H, Hannan MT, Gagnon DR, Cupples LA, et al. Dietary vitamin K intakes are associated with hip fracture but not with bone mineral density in elderly men and women. Am J Clin Nutr 2000;71:1201-8. https://www.ncbi.nlm.nih.gov/pubmed/10799384?dopt=Abstract[↩]
- Chan R, Leung J, Woo J. No association between dietary vitamin K intake and fracture risk in chinese community-dwelling older men and women: a prospective study. Calcif Tissue Int 2012;90:396-403. https://www.ncbi.nlm.nih.gov/pubmed/22451220?dopt=Abstract[↩]
- Wu W.J., Kim M.S., Ahn B.Y. The inhibitory effect of vitamin K on RANKL-induced osteoclast differentiation and bone resorption. Food Funct. 2015;6:3351–3358. doi: 10.1039/C5FO00544B[↩]
- Rangel L.B., de Siqueira D., do Rosário Soares O., Santana H.S., de Castro Miguel E., da Cunha M., de Abreu Oliveira A.L., Pedrosa D.F., Resgala L.C., Neto H.A., et al. Vitamin K supplementation modulates bone metabolism and ultra-structure of ovariectomized mice. Cell. Physiol. Biochem. 2018;51:356–374. doi: 10.1159/000495234[↩]
- Nagura N, Komatsu J, Iwase H, Hosoda H, Ohbayashi O, Nagaoka I, Kaneko K. Effects of the combination of vitamin K and teriparatide on the bone metabolism in ovariectomized rats. Biomed Rep. 2015 May;3(3):295-300. doi: 10.3892/br.2015.431[↩]
- Kazama JJ, Iwasaki Y, Fukagawa M. Uremic osteoporosis. Kidney Int Suppl (2011). 2013 Dec;3(5):446-450. doi: 10.1038/kisup.2013.93[↩]
- Cockayne S, Adamson J, Lanham-New S, Shearer MJ, Gilbody S, Torgerson DJ. Vitamin K and the prevention of fractures: systematic review and meta-analysis of randomized controlled trials. Arch Intern Med 2006;166:1256-61. https://www.ncbi.nlm.nih.gov/pubmed/16801507?dopt=Abstract[↩]
- Hao G., Zhang B., Gu M., Chen C., Zhang Q., Zhang G., Cao X. Vitamin K intake and the risk of fractures: A meta-analysis. Med. (Baltim.) 2017;96:e6725. doi: 10.1097/MD.0000000000006725[↩][↩]
- Moore A.E., Kim E., Dulnoan D., Dolan A.L., Voong K., Ahmad I., Gorska R., Harrington D.J., Hampson G. Serum vitamin K. Bone. 2020:115630. doi: 10.1016/j.bone.2020.115630[↩][↩]
- Tanaka S., Miyazaki T., Uemura Y., Miyakawa N., Gorai I., Nakamura T., Fukunaga M., Ohashi Y., Ohta H., Mori S., et al. Comparison of concurrent treatment with vitamin K. J. Bone Miner. Metab. 2017;35:385–395. doi: 10.1007/s00774-016-0768-5[↩]
- Jiang Y., Zhang Z.L., Zhu H.M., Wu Y.Y., Cheng Q., Wu F.L., Xing X.P., Liu J.L., Yu W., Meng X.W. Menatetrenone versus alfacalcidol in the treatment of Chinese postmenopausal women with osteoporosis: A multicenter, randomized, double-blinded, double-dummy, positive drug-controlled clinical trial. Clin. Interv. Aging. 2014;9:121–127. doi: 10.2147/CIA.S54107[↩]
- Kasukawa Y., Miyakoshi N., Ebina T., Aizawa T., Hongo M., Nozaka K., Ishikawa Y., Saito H., Chida S., Shimada Y. Effects of risedronate alone or combined with vitamin K2 on serum undercarboxylated Osteocalcin and Osteocalcin levels in postmenopausal osteoporosis. J. Bone Miner. Metab. 2014;32:290–297. doi: 10.1007/s00774-013-0490-5[↩]
- Knapen M.H., Drummen N.E., Smit E., Vermeer C., Theuwissen E. Three-year low-dose menaquinone-7 supplementation helps decrease bone loss in healthy postmenopausal women. Osteoporos. Int. 2013;24:2499–2507. doi: 10.1007/s00198-013-2325-6[↩][↩]
- Shiraki M., Shiraki Y., Aoki C., Miura M. Vitamin K2 (menatetrenone) effectively prevents fractures and sustains lumbar bone mineral density in osteoporosis. J. Bone Miner. Res. 2000;15:515–521. doi: 10.1359/jbmr.2000.15.3.515[↩]
- Mott A., Bradley T., Wright K., Cockayne E.S., Shearer M.J., Adamson J., Lanham-New S.A., Torgerson D.J. Effect of vitamin K on bone mineral density and fractures in adults: An updated systematic review and meta-analysis of randomised controlled trials. Osteoporos Int. 2019 doi: 10.1007/s00198-019-04949-0[↩]
- Inoue T., Fujita T., Kishimoto H., Makino T., Nakamura T., Nakamura T., Sato T., Yamazaki K. Randomized controlled study on the prevention of osteoporotic fractures (OF study): A phase IV clinical study of 15-mg menatetrenone capsules. J. Bone Miner. Metab. 2009;27:66–75. doi: 10.1007/s00774-008-0008-8[↩][↩][↩]
- Azuma K, Inoue S. Multiple Modes of Vitamin K Actions in Aging-Related Musculoskeletal Disorders. Int J Mol Sci. 2019 Jun 11;20(11):2844. doi: 10.3390/ijms20112844[↩]
- Vermeer C, Schurgers LJ. A comprehensive review of vitamin K and vitamin K antagonists. Hematol Oncol Clin North Am. 2000 Apr;14(2):339-53. doi: 10.1016/s0889-8588(05)70137-4[↩]
- Rodríguez-Olleros Rodríguez C, Díaz Curiel M. Vitamin K and Bone Health: A Review on the Effects of Vitamin K Deficiency and Supplementation and the Effect of Non-Vitamin K Antagonist Oral Anticoagulants on Different Bone Parameters. J Osteoporos. 2019 Dec 31;2019:2069176. doi: 10.1155/2019/2069176[↩]
- European Food Safety Authority. Scientific opinion on the substantiation of health claims related to vitamin K and maintenance of bone pursuant to Article 13(1) of Regulation (EC) No 1924/2006. The EFSA Journal 2009;7:1228.[↩]
- Magnesium. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional[↩]
- Fine KD, Santa Ana CA, Porter JL, Fordtran JS. Intestinal absorption of magnesium from food and supplements. J Clin Invest. 1991 Aug;88(2):396-402. doi: 10.1172/JCI115317[↩]
- Rude RK. Magnesium. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, Mass: Lippincott Williams & Wilkins; 2012:159-75.[↩][↩][↩][↩][↩][↩][↩]
- Rude RK, Singer FR, Gruber HE. Skeletal and hormonal effects of magnesium deficiency. J Am Coll Nutr. 2009 Apr;28(2):131-41. doi: 10.1080/07315724.2009.10719764[↩][↩]
- Tucker KL. Osteoporosis prevention and nutrition. Curr Osteoporos Rep. 2009 Dec;7(4):111-7. doi: 10.1007/s11914-009-0020-5[↩]
- Mutlu M, Argun M, Kilic E, Saraymen R, Yazar S. Magnesium, zinc and copper status in osteoporotic, osteopenic and normal post-menopausal women. J Int Med Res. 2007 Sep-Oct;35(5):692-5. doi: 10.1177/147323000703500514[↩]
- Institute of Medicine (IOM). Food and Nutrition Board. Dietary Reference Intakes: Calcium, Phosphorus, Magnesium, Vitamin D and Fluoride. Washington, DC: National Academy Press, 1997.[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Aydin H, Deyneli O, Yavuz D, Gözü H, Mutlu N, Kaygusuz I, Akalin S. Short-term oral magnesium supplementation suppresses bone turnover in postmenopausal osteoporotic women. Biol Trace Elem Res. 2010 Feb;133(2):136-43. doi: 10.1007/s12011-009-8416-8[↩]
- Volpe SL. Magnesium. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Ames, Iowa; John Wiley & Sons, 2012:459-74.[↩][↩]
- Elin RJ. Assessment of magnesium status for diagnosis and therapy. Magnes Res. 2010 Dec;23(4):S194-8. doi: 10.1684/mrh.2010.0213[↩]
- Gibson, RS. Principles of Nutritional Assessment, 2nd ed. New York, NY: Oxford University Press, 2005.[↩][↩][↩]
- Rude RK. Magnesium. In: Coates PM, Betz JM, Blackman MR, Cragg GM, Levine M, Moss J, White JD, eds. Encyclopedia of Dietary Supplements. 2nd ed. New York, NY: Informa Healthcare; 2010:527-37.[↩]
- Witkowski M, Hubert J, Mazur A. Methods of assessment of magnesium status in humans: a systematic review. Magnes Res. 2011 Dec;24(4):163-80. doi: 10.1684/mrh.2011.0292[↩]
- U.S. Department of Agriculture, Agricultural Research Service. FoodData Central. https://fdc.nal.usda.gov[↩]
- Ranade VV, Somberg JC. Bioavailability and pharmacokinetics of magnesium after administration of magnesium salts to humans. Am J Ther. 2001 Sep-Oct;8(5):345-57. doi: 10.1097/00045391-200109000-00008[↩][↩]
- Walker AF, Marakis G, Christie S, Byng M. Mg citrate found more bioavailable than other Mg preparations in a randomised, double-blind study. Magnes Res. 2003 Sep;16(3):183-91.[↩]
- Spencer H, Norris C, Williams D. Inhibitory effects of zinc on magnesium balance and magnesium absorption in man. J Am Coll Nutr. 1994 Oct;13(5):479-84. doi: 10.1080/07315724.1994.10718438[↩]
- Dunn CJ, Goa KL. Risedronate: a review of its pharmacological properties and clinical use in resorptive bone disease. Drugs. 2001;61(5):685-712. doi: 10.2165/00003495-200161050-00013[↩]
- Arayne MS, Sultana N, Hussain F. Interactions between ciprofloxacin and antacids–dissolution and adsorption studies. Drug Metabol Drug Interact. 2005;21(2):117-29. doi: 10.1515/dmdi.2005.21.2.117[↩]
- Sarafidis PA, Georgianos PI, Lasaridis AN. Diuretics in clinical practice. Part II: electrolyte and acid-base disorders complicating diuretic therapy. Expert Opin Drug Saf. 2010 Mar;9(2):259-73. doi: 10.1517/14740330903499257[↩][↩]
- FDA Drug Safety Communication: Low magnesium levels can be associated with long-term use of Proton Pump Inhibitor drugs (PPIs). https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-low-magnesium-levels-can-be-associated-long-term-use-proton-pump[↩][↩]
- Musso CG. Magnesium metabolism in health and disease. Int Urol Nephrol. 2009;41(2):357-62. doi: 10.1007/s11255-009-9548-7[↩][↩][↩]
- Kutsal E, Aydemir C, Eldes N, Demirel F, Polat R, Taspnar O, Kulah E. Severe hypermagnesemia as a result of excessive cathartic ingestion in a child without renal failure. Pediatr Emerg Care. 2007 Aug;23(8):570-2. doi: 10.1097/PEC.0b013e31812eef1c[↩]
- McGuire JK, Kulkarni MS, Baden HP. Fatal hypermagnesemia in a child treated with megavitamin/megamineral therapy. Pediatrics. 2000 Feb;105(2):E18. doi: 10.1542/peds.105.2.e18[↩]
- Onishi S, Yoshino S. Cathartic-induced fatal hypermagnesemia in the elderly. Intern Med. 2006;45(4):207-10. doi: 10.2169/internalmedicine.45.1482[↩]
- US Department of Health and Human Services. Physical activity and health: A report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, President’s Council on Physical Fitness and Sports; 1996. p. 300.[↩]
- Rubin C, Recker R, Cullen D, Ryaby J, McCabe J, Mcleod K. Prevention of postmenopausal bone loss by a low-magnitude, high-frequency mechanical stimuli: A clinical trial assessing compliance, efficacy, and safety. J Bone Miner Res. 2004 Mar;19(3):343–51. https://www.ncbi.nlm.nih.gov/pubmed/15040821[↩]
- Verschueren SM, Roelants M, Delecluse C, Swinnen S, Vanderschueren D, Boonen S. Effect of 6-month whole body vibration training on hip density, muscle strength, and postural control in postmenopausal women: A randomized controlled pilot study. J Bone Miner Res. 2004 Mar;19(3):352–9. https://www.ncbi.nlm.nih.gov/pubmed/15040822[↩]
- Ward K, Alsop C, Caulton J, Rubin C, Adams J, Mughal Z. Low magnitude mechanical loading is osteogenic in children with disabling conditions. J Bone Miner Res. 2004 Mar;19(3):360–9. https://www.ncbi.nlm.nih.gov/pubmed/15040823[↩]
- Kraemer et al. 2002, ACSM 1998a, ACSM 1998b[↩]
- Cochrane Review 6 July 2011. – Exercise for preventing and treating osteoporosis in postmenopausal women – http://www.cochrane.org/CD000333/MUSKEL_exercise-for-preventing-and-treating-osteoporosis-in-postmenopausal-women[↩]
- Schurch MA, Rizzoli R, Slosman D, Vadas L, Vergnaud P, Bonjour JP. Protein supplements increase serum insulin-like growth factor-I levels and attenuate proximal femur bone loss in patients with recent hip fracture. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1998 May 15;128(10):801–9.[↩]
- 2015-2020 Dietary Guidelines for Americans 8th Edition. https://www.cnpp.usda.gov/dietary-guidelines[↩]
- The National Institutes of Health, Osteoporosis and Related Bone Diseases, National Resource Center. – Osteoporosis Basics – https://www.niams.nih.gov/Health_Info/Bone/Osteoporosis/osteoporosis_hoh.asp[↩]
- Bone Density Scan (DEXA or DXA). https://www.radiologyinfo.org/en/info/dexa[↩]
- National Center for Biotechnology Information, U.S. National Library of Medicine. – The Osteoporosis Pyramid for Prevention and Treatment – https://www.ncbi.nlm.nih.gov/books/NBK45501/figure/ch9.f1/?report=objectonly[↩]
- Edwards BJ, Hellstein JW, Jacobsen PL, et al: Updated recommendations for managing the care of patients receiving oral bisphosphonate therapy: An advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 139:1674–1677, 2008. https://www.ncbi.nlm.nih.gov/pubmed/19047674[↩][↩][↩]
- Langdahl BL, Teglbjærg CS, Ho PR, Chapurlat R, Czerwinski E, Kendler DL, Reginster JY, Kivitz A, Lewiecki EM, Miller PD, Bolognese MA, McClung MR, Bone HG, Ljunggren Ö, Abrahamsen B, Gruntmanis U, Yang YC, Wagman RB, Mirza F, Siddhanti S, Orwoll E. A 24-month study evaluating the efficacy and safety of denosumab for the treatment of men with low bone mineral density: results from the ADAMO trial. J Clin Endocrinol Metab. 2015 Apr;100(4):1335-42. doi: 10.1210/jc.2014-4079[↩]
- Ferrari S, Adachi JD, Lippuner K, Zapalowski C, Miller PD, Reginster JY, Törring O, Kendler DL, Daizadeh NS, Wang A, O’Malley CD, Wagman RB, Libanati C, Lewiecki EM. Further reductions in nonvertebral fracture rate with long-term denosumab treatment in the FREEDOM open-label extension and influence of hip bone mineral density after 3 years. Osteoporos Int. 2015 Dec;26(12):2763-71. doi: 10.1007/s00198-015-3179-x[↩]
- Meier C, Uebelhart B, Aubry-Rozier B, Birkhäuser M, Bischoff-Ferrari HA, Frey D, Kressig RW, Lamy O, Lippuner K, Stute P, Suhm N, Ferrari S. Osteoporosis drug treatment: duration and management after discontinuation. A position statement from the SVGO/ASCO. Swiss Med Wkly. 2017 Aug 16;147:w14484. doi: 10.4414/smw.2017.14484[↩]
- Bone HG, Wagman RB, Brandi ML, Brown JP, Chapurlat R, Cummings SR, Czerwiński E, Fahrleitner-Pammer A, Kendler DL, Lippuner K, Reginster JY, Roux C, Malouf J, Bradley MN, Daizadeh NS, Wang A, Dakin P, Pannacciulli N, Dempster DW, Papapoulos S. 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol. 2017 Jul;5(7):513-523. doi: 10.1016/S2213-8587(17)30138-9[↩][↩][↩]
- Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C; FREEDOM Trial. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009 Aug 20;361(8):756-65. doi: 10.1056/NEJMoa0809493. Epub 2009 Aug 11. Erratum in: N Engl J Med. 2009 Nov 5;361(19):1914.[↩][↩]
- Gregson CL, Armstrong DJ, Bowden J, Cooper C, Edwards J, Gittoes NJL, Harvey N, Kanis J, Leyland S, Low R, McCloskey E, Moss K, Parker J, Paskins Z, Poole K, Reid DM, Stone M, Thomson J, Vine N, Compston J. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2022 Apr 5;17(1):58. doi: 10.1007/s11657-022-01061-5. Erratum in: Arch Osteoporos. 2022 May 19;17(1):80.[↩][↩][↩][↩]
- FDA investigating risk of severe hypocalcemia in patients on dialysis receiving osteoporosis medicine Prolia (denosumab). https://www.fda.gov/drugs/drug-safety-and-availability/fda-investigating-risk-severe-hypocalcemia-patients-dialysis-receiving-osteoporosis-medicine-prolia[↩]
- Denosumab: monitoring recommended. https://www.gov.uk/drug-safety-update/denosumab-monitoring-recommended[↩]
- Tsourdi E, Zillikens MC, Meier C, Body JJ, Gonzalez Rodriguez E, Anastasilakis AD, Abrahamsen B, McCloskey E, Hofbauer LC, Guañabens N, Obermayer-Pietsch B, Ralston SH, Eastell R, Pepe J, Palermo A, Langdahl B. Fracture risk and management of discontinuation of denosumab therapy: a systematic review and position statement by ECTS. J Clin Endocrinol Metab. 2020 Oct 26:dgaa756. doi: 10.1210/clinem/dgaa756[↩]
- Dennison EM, Cooper C, Kanis JA, Bruyère O, Silverman S, McCloskey E, Abrahamsen B, Prieto-Alhambra D, Ferrari S; IOF Epidemiology/Quality of Life Working Group. Fracture risk following intermission of osteoporosis therapy. Osteoporos Int. 2019 Sep;30(9):1733-1743. doi: 10.1007/s00198-019-05002-w[↩]
- Cummings, S.R., Ferrari, S., Eastell, R., Gilchrist, N., Jensen, J.-E.B., McClung, M., Roux, C., Törring, O., Valter, I., Wang, A.T. and Brown, J.P. (2018), Vertebral Fractures After Discontinuation of Denosumab: A Post Hoc Analysis of the Randomized Placebo-Controlled FREEDOM Trial and Its Extension. J Bone Miner Res, 33: 190-198. https://doi.org/10.1002/jbmr.3337[↩]
- Horne AM, Mihov B, Reid IR. Effect of Zoledronate on Bone Loss After Romosozumab/Denosumab: 2-Year Follow-up. Calcif Tissue Int. 2019 Jul;105(1):107-108. doi: 10.1007/s00223-019-00553-w[↩]
- Anastasilakis, A.D., Papapoulos, S.E., Polyzos, S.A., Appelman-Dijkstra, N.M. and Makras, P. (2019), Zoledronate for the Prevention of Bone Loss in Women Discontinuing Denosumab Treatment. A Prospective 2-Year Clinical Trial. J Bone Miner Res, 34: 2220-2228. https://doi.org/10.1002/jbmr.3853[↩]
- Everts-Graber, J., Reichenbach, S., Ziswiler, H.R., Studer, U. and Lehmann, T. (2020), A Single Infusion of Zoledronate in Postmenopausal Women Following Denosumab Discontinuation Results in Partial Conservation of Bone Mass Gains. J Bone Miner Res, 35: 1207-1215. https://doi.org/10.1002/jbmr.3962[↩]
- Sølling, A.S., Harsløf, T. and Langdahl, B. (2020), Treatment with Zoledronate Subsequent to Denosumab in Osteoporosis: a Randomized Trial. J Bone Miner Res, 35: 1858-1870. https://doi.org/10.1002/jbmr.4098[↩]
- Makras P, Appelman-Dijkstra NM, Papapoulos SE, van Wissen S, Winter EM, Polyzos SA, Yavropoulou MP, Anastasilakis AD. The Duration of Denosumab Treatment and the Efficacy of Zoledronate to Preserve Bone Mineral Density After Its Discontinuation. J Clin Endocrinol Metab. 2021 Sep 27;106(10):e4155-e4162. doi: 10.1210/clinem/dgab321[↩]
- Tsourdi E, Langdahl B, Cohen-Solal M, Aubry-Rozier B, Eriksen EF, Guañabens N, Obermayer-Pietsch B, Ralston SH, Eastell R, Zillikens MC. Discontinuation of Denosumab therapy for osteoporosis: A systematic review and position statement by ECTS. Bone. 2017 Dec;105:11-17. doi: 10.1016/j.bone.2017.08.003[↩]
- Kendler D, Chines A, Clark P, Ebeling PR, McClung M, Rhee Y, Huang S, Stad RK. Bone Mineral Density After Transitioning From Denosumab to Alendronate. J Clin Endocrinol Metab. 2020 Mar 1;105(3):e255–64. doi: 10.1210/clinem/dgz095[↩]
- Gallagher JC, Goldgar D. Treatment of postmenopausal osteoporosis with high doses of synthetic calcitriol. A randomized controlled study. Ann Intern Med. 1990 Nov 1;113(9):649-55. doi: 10.7326/0003-4819-113-9-649[↩]
- Zuckerman JD. Hip fracture. N Engl J Med. 1996 Jun 6;334(23):1519–25.[↩]
- Johnell O, Scheek WH, Lu Y, Reginster JY, Need AG, Seeman E. Additive effects of raloxifene and alendronate on bone density and biochemical markers of bone remodeling in postmenopausal women with osteoporosis. J Clin Endocrinol Metab. 2002 Mar;87(3):985–92.[↩]
- Evans A, Jensen M, Kip K, DeNardo AJ, Lawler GJ, Negin GA, Remley KB, Boutin SM, Dunnagan SA. Vertebral compression fractures: Pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty—retrospective report of 245 cases. Radiology. 2003 Feb;226(2):366–72.[↩][↩]
- Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001 Jul 15;26(14):1631–8.[↩][↩]
- Sinaki M, Itoi E, Wahner HW, Wollan P, Gelzcer R, Mullan BP, Collins DA, Hodgson SF. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10-year follow-up of postmenopausal women. Bone. 2002 Jun;30(6):836–41. https://www.ncbi.nlm.nih.gov/pubmed/12052450[↩]
- Bonner FJ Jr, Sinaki M, Grabois M, Shipp KM, Lane JM, Lindsay R, Gold DT, Cosman F, Bouxsein ML, Weinstein JN, et al. Health professional’s guide to rehabilitation of the patient with osteoporosis. Osteoporos Int. 2003;14(Suppl 2):S1–22. https://www.ncbi.nlm.nih.gov/pubmed/12759719[↩]
- Porter JL, Varacallo M. Osteoporosis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441901[↩]