What is bilirubin
Bilirubin is an orange-yellow pigment, a waste product primarily produced by the normal breakdown of heme. Heme is a component of hemoglobin (the substance that carries oxygen in your red blood cells), which is found in red blood cells (RBCs). Bilirubin is ultimately processed by the liver to allow its elimination from the body.
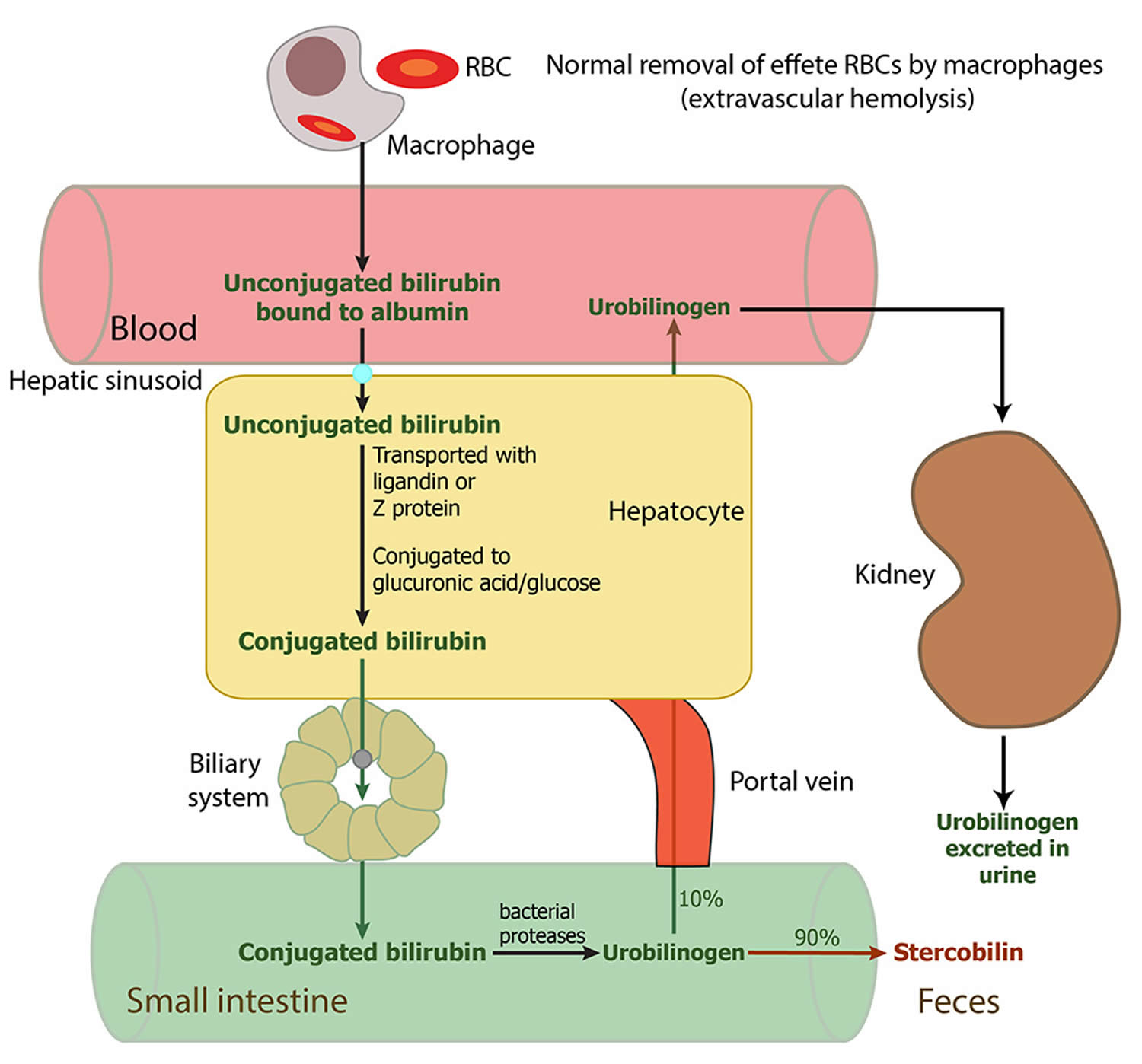
Red blood cells normally degrade after about 120 days in the blood circulation. As heme is released from hemoglobin, it is converted to bilirubin. This form of bilirubin is also called unconjugated bilirubin. Unconjugated bilirubin is carried by proteins to the liver; there, sugars are attached (conjugated) to bilirubin to form conjugated bilirubin. Conjugated bilirubin enters the bile and passes from the liver to the small intestines; there, it is further broken down by bacteria and eventually eliminated in the stool. Thus, the breakdown products of bilirubin give stool its characteristic brown color.
A small amount (approximately 250 to 350 milligrams) of bilirubin is produced daily in a normal, healthy adult. Most (85%) of bilirubin is derived from damaged or degraded red blood cells, with the remaining amount derived from the bone marrow or liver. Normally, small amounts of unconjugated bilirubin are released into the blood, but virtually no conjugated bilirubin is present. Both forms can be measured or estimated by laboratory tests, and a total bilirubin result (a sum of these) may also be reported.
Bilirubin concentrations tend to be slightly higher in males than females. African Americans routinely show lower bilirubin concentrations than non-African Americans. Strenuous exercise may increase bilirubin levels.
Drugs that can decrease total bilirubin include barbiturates, caffeine, penicillin, and high doses of salicylates. The drug atazanavir increases unconjugated (indirect) bilirubin.
If the bilirubin level increases in the blood, a person may appear jaundiced, with a yellowing of the skin and/or whites of the eyes. The pattern of bilirubin test results can give your doctor information regarding the condition that may be present. For example, unconjugated bilirubin may be increased when there is an unusual amount of red blood cell destruction (hemolysis) or when the liver is unable to process bilirubin (i.e., with liver diseases such as cirrhosis or inherited problems). Conversely, conjugated bilirubin can increase when the liver is able to process bilirubin but is not able to pass the conjugated bilirubin to the bile for removal; when this happens, the cause is often acute hepatitis or blockage of the bile ducts.
Increased total and unconjugated bilirubin levels are relatively common in newborns in the first few days after birth. This finding is called “physiologic jaundice of the newborn” and occurs because the newborn’s liver is not mature enough to process bilirubin yet. Usually, physiologic jaundice of the newborn resolves itself within a few days. However, in hemolytic disease of the newborn, red blood cells may be destroyed because of blood incompatibilities between the baby and the mother; in these cases, treatment may be required because high levels of unconjugated bilirubin can damage the newborn’s brain.
A rare (about 1 in 10,000 births) but life-threatening congenital condition called biliary atresia can cause increased total and conjugated bilirubin levels in newborns. This condition must be quickly detected and treated, usually with surgery, to prevent serious liver damage that may require liver transplantation within the first few years of life. Some children may require liver transplantation despite early surgical treatment.
Rare inherited disorders that cause abnormal bilirubin metabolism such as Rotor, Dubin-Johnson, and Crigler-Najjar syndromes, may also cause increased levels of bilirubin.
Crigler-Najjar syndromes type I and type II, are rare genetic disorders that are caused by a low or absent activity of bilirubin UDP-glucuronyl-transferase. In Crigler-Najjar syndromes type I, the enzyme activity is totally absent, the excretion rate of bilirubin is greatly reduced and the serum concentration of unconjugated bilirubin is greatly increased. Patients with Crigler-Najjar syndromes may die in infancy owing to the development of kernicterus.
Figure 1. Bilirubin metabolism
Unconjugated bilirubin
Though unconjugated bilirubin may be toxic to brain development in newborns (up to 2-4 weeks of age), it does not pose the same threat to older children and adults. In older children and adults, the “blood-brain barrier” is more developed and prevents bilirubin from gaining access to brain cells. Nevertheless, elevated bilirubin strongly suggests that a medical condition is present that must be evaluated and treated.
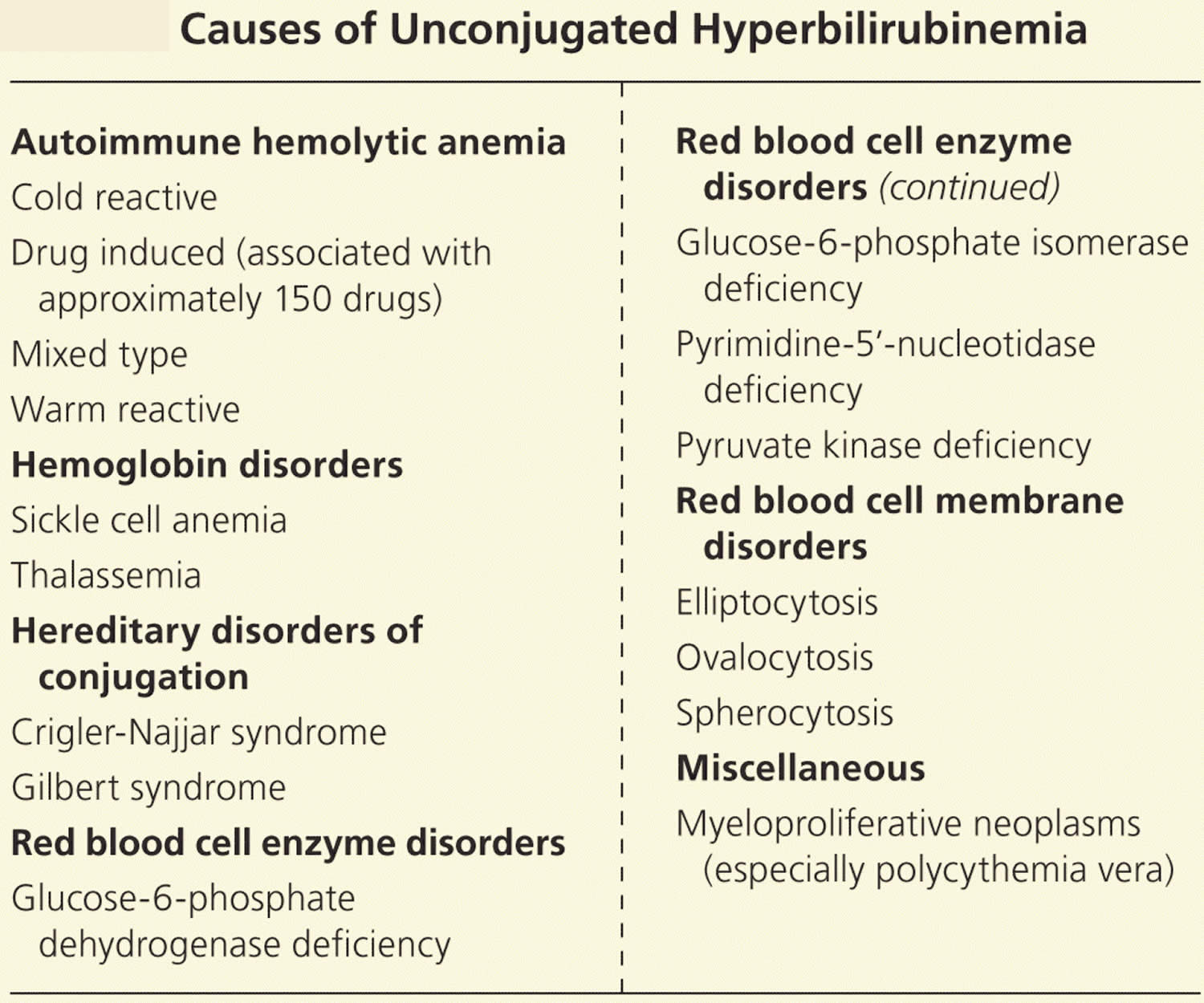
Unconjugated hyperbilirubinemia
Increased bilirubin production
Unconjugated hyperbilirubinemia is usually a result of too much bilirubin presented to the conjugating machinery (from increased red blood cell destruction). Increased red blood cell breakdown may be caused by red blood cell membrane disorders, red blood cell enzyme disorders, hemoglobin disorders (Thalassemias), autoimmune red blood cell destruction (autoimmune hemolytic anemia), or some cancers 1, 2, 3, 4. The excess turnover of red blood cells results in increased heme metabolism, producing large amounts of bilirubin that overwhelm the conjugating machinery, leading to decreased excretion and clinical jaundice.
Impaired bilirubin conjugation
Deficiencies in the same conjugating machinery may also lead to jaundice in individuals with normal red blood cell turnover. Gilbert syndrome involves a deficiency in uridine diphosphate-glucuronosyltransferase, and it affects 10% of the white population 5. This is a benign condition that may be exacerbated by physical or emotional stress such as illness, strenuous exercise, or fasting. Crigler-Najjar syndrome is a more severe variant of the same uridine diphosphate-glucuronosyltransferase enzyme deficiency 5. Patients with impaired conjugation due to low levels of the bilirubin-UGT enzyme are particularly susceptible to jaundice from medications that inhibit this enzyme, such as protease inhibitors 6. Table 1 lists the causes of unconjugated hyperbilirubinemia.
Table 1. Causes of Unconjugated Hyperbilirubinemia
Conjugated bilirubin
Conjugated bilirubin is a water-soluble form of bilirubin formed in the liver by the chemical addition of sugar molecules to unconjugated bilirubin; when present in the blood, conjugated bilirubin can become chemically bound to albumin, forming delta-bilirubin also known as biliprotein.
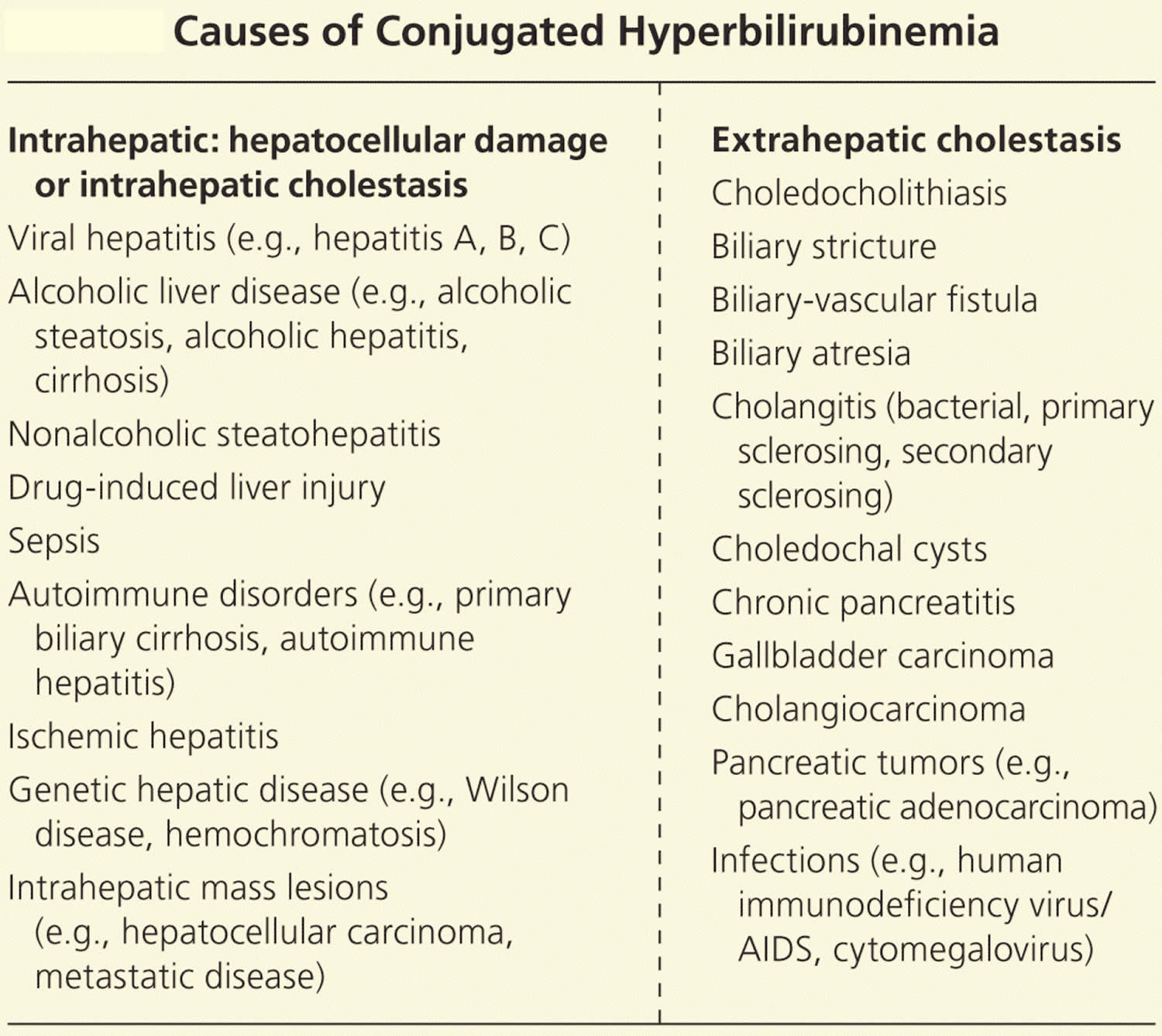
Conjugated hyperbilirubinemia
Intrahepatic disorders and intrahepatic cholestasis
The largest worldwide contributor to liver disease is viral hepatitis, mostly from hepatitis C 8. Viral hepatitis causes increased oxidative stress within liver cells (hepatocytes), leading to cell death, scarring, and diminished liver mass available for normal function 9, 10. Chronic alcohol consumption can cause various hepatic disorders, including fatty liver disease (steatosis) with minimal symptoms and often no jaundice; alcoholic hepatitis with acute onset jaundice and more severe symptoms; and cirrhosis, which is often associated with decompensation and liver failure in the setting of jaundice 11. Jaundice in persons with alcoholic liver disease can occur via multiple mechanisms, such as direct hepatocellular damage caused by ethanol metabolites or from alcohol’s effect on bile acid uptake and secretion contributing to cholestasis (reduced or stopped bile flow) 11, 12.
Approximately 30% to 40% of patients with nonalcoholic fatty liver disease (NAFLD) progress to nonalcoholic steatohepatitis (NASH), and approximately 40% to 50% of these patients develop fibrosis or cirrhosis that may lead to hyperbilirubinemia 13. Although the exact mechanism is poorly understood, liver lipid deposition may trigger inflammation and fibrosis, particularly when coupled with type 2 diabetes 13. Sepsis may also induce hyperbilirubinemia as circulating acute phase reactants and bacterial endotoxins disrupt bilirubin transport, leading to cholestasis and elevated bile salt levels 14, 15.
Extrahepatic disorders
Conjugated hyperbilirubinemia may also arise from extrahepatic obstruction. Patients with biliary obstruction may present with multiple signs and symptoms, including fever, itch (pruritus), abdominal pain, weight loss, muscle wasting, dark urine, and pale stools. Choledocholithiasis or the presence of gallstones within the common bile duct, is the most common non-neoplastic cause of biliary obstruction, accounting for 14% of all new cases of jaundice 18. An estimated 20 million Americans have gallstones, and risk factors for gallstones within the common bile duct (choledocholithiasis) include female sex, older age, increasing body mass index, and rapid weight loss 19.
Gallstones may cause jaundice by obstructing the biliary tree (typically the common bile duct) or by inducing a biliary stricture 20. Less commonly, stones in the gallbladder or cystic duct may mechanically compress the common hepatic duct causing jaundice, and, rarely, stones may cause the formation of a biliary-vascular fistula with accompanying jaundice 21. Biliary stricture causing postoperative jaundice is a rare complication of cholecystectomy (0.6% of cases) 20, 22.
Jaundice may be caused by surgeries such as liver transplantation and the Whipple and Billroth procedures, which both involve the creation of a choledochojejunostomy. Chronic pancreatitis may cause biliary strictures and jaundice, as may different forms of cholangitis 22, 23. In children, biliary atresia and choledochal cysts are the main causes of extrahepatic biliary obstruction 24.
Tumors are associated with 6.2% of new-onset cases of jaundice 18. Cholangiocarcinoma may affect the proximal or distal portions of the biliary tree by causing biliary strictures. Five-year survival for persons who have resection is 20% to 40%; survival in unresectable disease is less than one year 25, 26. Primary sclerosing cholangitis confers a 1,500-fold increased risk of cholangiocarcinoma, but more than 80% of cases have no risk factors for cholangiocarcinoma 25.
Gallbladder cancer, although rare, is the most common biliary tract malignancy; risk factors include gallstones, infection (Salmonella typhi), and female sex. Median survival is six to 12 months, depending on the stage at diagnosis 27. Ampullary cancers and bile duct compression from lymphadenopathy, or external tumors such as pancreatic cancer, may also cause bile duct obstruction.
Table 2. Causes of Conjugated Hyperbilirubinemia
Normal bilirubin levels
Direct (conjugated) Bilirubin
- > or =12 months: 0.0-0.3 mg/dL (less than 5.1 µmol/L)
Reference values have not been established for patients who are <12 months of age.
Total Bilirubin
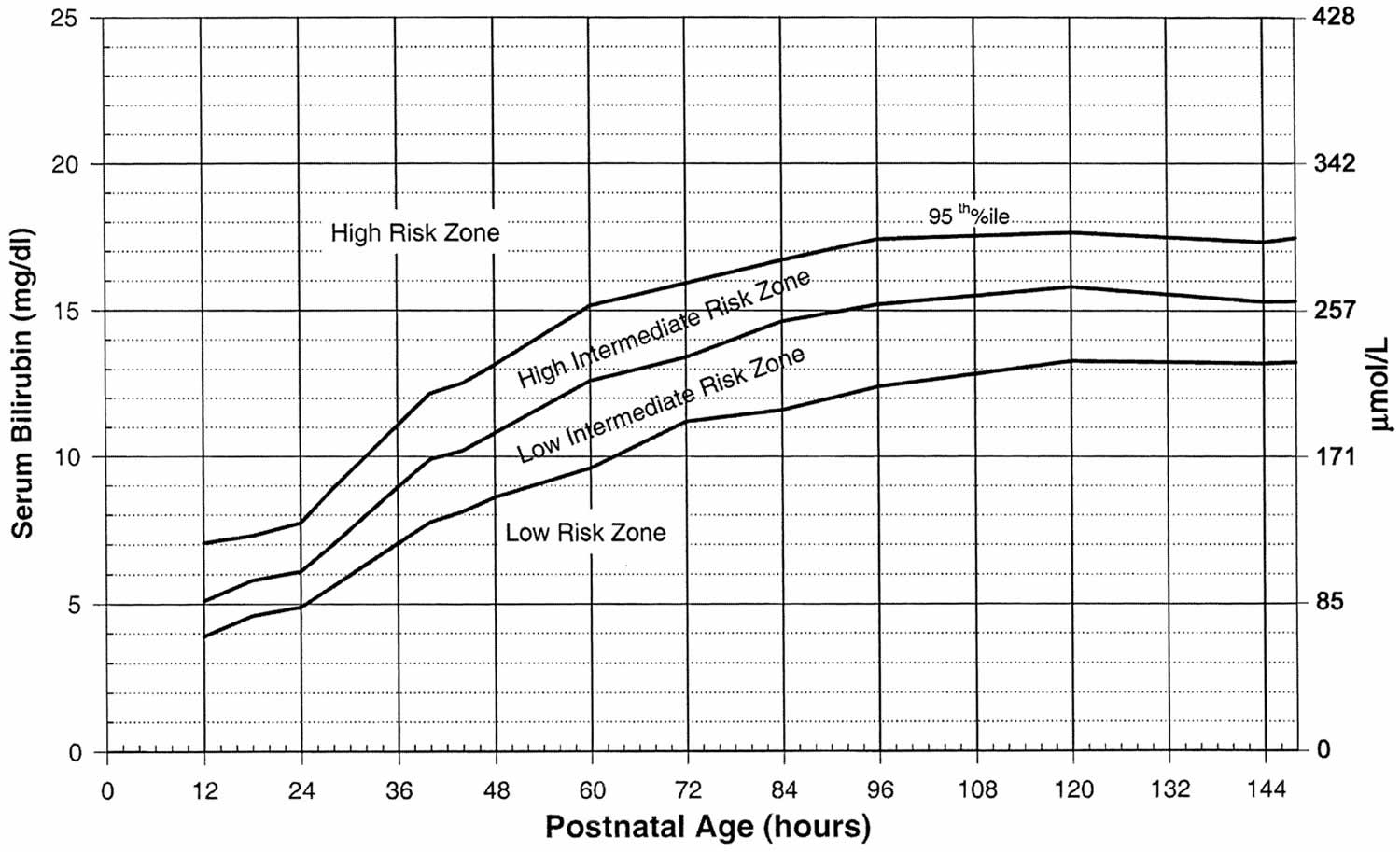
- 0-6 days: Refer to www.bilitool.org for information on age-specific (postnatal hour of life) serum bilirubin values.
- 7-14 days: <15.0 mg/dL
- 15 days to 17 years: < or =1.0 mg/dL
- > or =18 years: 0.1 to 1.2 mg/dL (1.71 to 20.5 µmol/L)
Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or may test different samples. Talk to your provider about the meaning of your specific test results.
Bilirubin in urine
Bilirubin is not normally present in the urine. However, conjugated bilirubin is water-soluble and may be eliminated from the body through the urine if it cannot pass into the bile. Measurable bilirubin in the urine usually indicates blockage of liver or bile ducts, hepatitis, or some other form of liver damage and may be detectable early in disease; for this reason, bilirubin testing is integrated into common dipstick testing used for routine urinalysis.
Are some people more at genetic risk of abnormal bilirubin levels?
Several inherited chronic conditions increase bilirubin levels in the blood and include Gilbert syndrome, Dubin-Johnson syndrome, Rotor syndrome, and Crigler-Najjar syndrome. The first three are usually mild, chronic conditions that can be aggravated under certain conditions but in general cause no significant health problems. For example, Gilbert syndrome is very common; about 1 in every 6 people has this genetic abnormality, but usually people with Gilbert syndrome do not have elevated bilirubin. Crigler-Najjar syndrome is the most serious inherited condition listed; this disorder is relatively rare, and some people with it may die.
How do you treat abnormal bilirubin levels and/or jaundice?
Treatment depends on the cause of the jaundice. In newborns, phototherapy (special light therapy), blood exchange transfusion, and/or certain drugs may be used to reduce the bilirubin level. In Gilbert, Rotor, and Dubin-Johnson syndromes, no treatment is usually necessary. Crigler-Najjar syndrome may respond to certain enzyme drug therapy or may require a liver transplant. Jaundice caused by an obstruction is often resolved by surgery. Jaundice due to cirrhosis is a result of long-term liver damage and does not respond well to any type of therapy other than liver transplantation.
Bilirubin test
Bilirubin test measures the amount of bilirubin in your blood to evaluate your liver function or to help diagnose anemias caused by red blood cell destruction (hemolytic anemia).
A bilirubin test is used to detect an elevated bilirubin level in the blood. Bilirubin test may be used to help determine the cause of jaundice and/or help diagnose conditions such as liver disease, hemolytic anemia, and blockage of the bile ducts.
Bilirubin is an orange-yellow pigment, a waste product primarily produced by the normal breakdown of heme. Heme is a component of hemoglobin, which is found in red blood cells. Bilirubin is ultimately processed by the liver to allow its elimination from the body. Any condition that accelerates the breakdown of red blood cells or affects the processing and elimination of bilirubin may cause an elevated blood level.
Two forms of bilirubin can be measured or estimated by laboratory tests:
- Unconjugated bilirubin—when heme is released from hemoglobin, it is converted to unconjugated bilirubin. It is carried by proteins to the liver. Small amounts may be present in the blood.
- Conjugated bilirubin—formed in the liver when sugars are attached (conjugated) to bilirubin. It enters the bile and passes from the liver to the small intestines and is eventually eliminated in the stool. Normally, no conjugated bilirubin is present in the blood.
Usually, a chemical test is used to first measure the total bilirubin level (unconjugated plus conjugated bilirubin). If the total bilirubin level is increased, the laboratory can use a second chemical test to detect water-soluble forms of bilirubin, called “direct” bilirubin. The direct bilirubin test provides an estimate of the amount of conjugated bilirubin present. Subtracting direct bilirubin level from the total bilirubin level helps estimate the “indirect” level of unconjugated bilirubin. The pattern of bilirubin test results can give your healthcare provider information regarding the condition that may be present.
In adults and older children, bilirubin is measured to:
- Diagnose and/or monitor diseases of the liver and bile duct (e.g., cirrhosis, hepatitis, or gallstones)
- Evaluate people with sickle cell disease or other causes of hemolytic anemia; these people may have episodes called crises when excessive red blood cell destruction increases bilirubin levels.
In newborns with jaundice, bilirubin is used to distinguish the causes of jaundice.
- In both physiologic jaundice of the newborn and hemolytic disease of the newborn, only unconjugated (indirect) bilirubin is increased.
- In much less common cases, damage to the newborn’s liver from neonatal hepatitis and biliary atresia will increase conjugated (direct) bilirubin concentrations as well, often providing the first evidence that one of these less common conditions is present.
It is important that an elevated level of bilirubin in a newborn be identified and quickly treated because excessive unconjugated bilirubin damages developing brain cells. The consequences of this damage include mental retardation, learning and developmental disabilities, hearing loss, eye movement problems, and death.
When is bilirubin test ordered?
A healthcare practitioner usually orders a bilirubin test in conjunction with other liver function tests (alkaline phosphatase [ALP], aspartate aminotransferase [AST], alanine aminotransferase [ALT]) when someone shows signs of abnormal liver function.
A bilirubin level may be ordered when a person:
- Shows evidence of jaundice
- Has a history of drinking excessive amounts of alcohol
- Has suspected drug toxicity
- Has been exposed to hepatitis-causing viruses
Other symptoms that may be present include:
- Dark, amber-colored urine
- Nausea/vomiting
- Abdominal pain and/or swelling
- Fatigue and general malaise that often accompany chronic liver disease
Measuring and monitoring bilirubin in newborns with jaundice is considered standard medical care.
Tests for bilirubin may also be ordered when someone is suspected of having (or known to have) hemolytic anemia as a cause of anemia. In this case, it is often ordered along with other tests used to evaluate hemolysis, such as complete blood count, reticulocyte count, haptoglobin, and lactate dehydrogenase (LDH).
What does high bilirubin levels mean?
Adults and children
Increased total bilirubin that is mainly unconjugated (indirect) bilirubin may be a result of:
- Hemolytic anemia or pernicious anemia
- Megaloblastic anemia
- A blood disorder called erythroblastosis fetalis
- Transfusion reaction in which red blood cells that were given in a transfusion are destroyed by the person’s immune system
- Cirrhosis (scarring of the liver)
- A relatively common inherited condition called Gilbert syndrome, due to low levels of the enzyme that produces conjugated bilirubin
If conjugated (direct) bilirubin is elevated more than unconjugated (indirect) bilirubin, there typically is a problem associated with decreased elimination of bilirubin by the liver cells. Some conditions that may cause this include:
- Viral hepatitis
- Drug reactions
- Alcoholic liver disease
Conjugated (direct) bilirubin is also elevated more than unconjugated (indirect) bilirubin when there is blockage of the bile ducts. This may occur, for example, with:
- Gallstones present in the bile ducts
- Tumors
- Scarring of the bile ducts or abnormal narrowing of the common bile duct (biliary stricture)
- Cancer of the pancreas or gallbladder cancer
In hepatobiliary diseases of various causes, bilirubin uptake, storage, and excretion are impaired to varying degrees. Thus, both conjugated and unconjugated bilirubin are retained and a wide range of abnormal serum concentrations of each form of bilirubin may be observed. Both conjugated and unconjugated bilirubins are increased in hepatitis and space-occupying lesions of the liver; and obstructive lesions such as carcinoma of the head of the pancreas, common bile duct, or ampulla of Vater.
Newborns
An elevated bilirubin level in a newborn may be temporary and resolve itself within a few days to two weeks. However, if the bilirubin level is above a critical threshold or increases rapidly, an investigation of the cause is needed so appropriate treatment can be initiated. Increased bilirubin concentrations may result from the accelerated breakdown of red blood cells due to:
- Blood type incompatibility between the mother and her newborn
- Certain congenital infections
- Lack of oxygen (hypoxia)
- Diseases that can affect the liver
In most of these conditions, only unconjugated (indirect) bilirubin is increased. An elevated conjugated (direct) bilirubin is seen in the rare conditions of biliary atresia and neonatal hepatitis. Biliary atresia requires surgical intervention to prevent liver damage.
Physiologic jaundice should resolve in 5 to 10 days in full-term infants and by 14 days in preterm infants.
Neonatal jaundice
Jaundice is one of the most common conditions requiring medical attention in newborn babies. Approximately 60% of term and 80% of preterm babies develop jaundice in the first week of life, and about 10% of breastfed babies are still jaundiced at 1 month of age 28. In most babies with jaundice there is no underlying disease, and this early jaundice (termed ‘physiological jaundice’) is generally harmless. However, there are pathological causes of jaundice in the newborn, which, although rare, need to be detected. Such pathological jaundice may co-exist with physiological jaundice.
Neonatal jaundice refers to yellow coloration of the skin and the sclera (whites of the eyes) of newborn babies that results from accumulation of bilirubin in the skin and mucous membranes. This is associated with a raised level of bilirubin in the circulation, a condition known as hyperbilirubinemia. The term “kernicterus” refers to the ‘yellow staining of the basal nuclei of the brain’ caused by bilirubin. This is seen in parts of the brain on autopsy.
Factors significantly associated with hyperbilirubinemia are gestational age < 38 weeks, visible jaundice within 24 hours of birth, mother’s intention to breastfeed exclusively and family history of neonatal jaundice requiring treatment with phototherapy.
The level of bilirubinemia that results in kernicterus in a given infant is unknown. Poor-quality studies have shown a link between kernicterus (acute and chronic brain effects of severe hyperbilirubinemia) and both high serum bilirubin levels and free bilirubin levels in all babies.
Severe jaundice requiring exchange transfusion (bilirubin > 340 micromol/liter) and early onset of jaundice (within 24 hours) are statistically significant risk factors for hearing loss 28. Deafness is a clinical manifestation of kernicterus. Hemolytic disorders such as G6PD deficiency and ABO incompatibility (ABO incompatible blood) may cause a rapid increase in bilirubin level, and these disorders have been over-represented in international kernicterus registries and population studies of significant hyperbilirubinemia. A study of low-birthweight babies found a weak association between high serum bilirubin levels (> 340 micromol/liter) and neurodevelopmental impairment, hearing impairment and psychomotor impairment.
Bilirubin encephalopathy
Bilirubin encephalopathy is a rare neurological condition that occurs in some newborns with severe jaundice. Bilirubin encephalopathy is a serious condition. Many infants with late-stage nervous system complications die.
Bilirubin encephalopathy most often develops in the first week of life, but may be seen up until the third week. Some newborns with Rh hemolytic disease are at high risk for severe jaundice that can lead to this condition. Rarely, bilirubin encephalopathy can develop in seemingly healthy babies.
Bilirubin encephalopathy symptoms
The symptoms depend on the stage of bilirubin encephalopathy. Not all babies with kernicterus on autopsy have had definite symptoms.
Early stage:
- Extreme jaundice
- Absent startle reflex
- Poor feeding or sucking
- Extreme sleepiness (lethargy) and low muscle tone (hypotonia)
Middle stage:
- High-pitched cry
- Irritability
- May have arched back with neck hyperextended backwards, high muscle tone (hypertonia)
- Poor feeding
Late stage:
- Stupor or coma
- No feeding
- Shrill cry
- Muscle rigidity, markedly arched back with neck hyperextended backwards
- Seizures
Possible complications
Complications may include:
- Permanent brain damage
- Hearing loss
- Death
Prevention
Treating jaundice or conditions that may lead to it can help prevent this problem. Infants with the first signs of jaundice have bilirubin level measured within 24 hours. If the level is high, the infant should be screened for diseases that involve the destruction of red blood cells (hemolysis).
All newborns have a follow-up appointment within 2 to 3 days after leaving the hospital. This is very important for late preterm or early term babies (born more than 2 to 3 weeks before their due date).
Treatment
Treatment depends on how old the baby is (in hours) and whether the baby has any risk factors (such as prematurity). It may include:
- Light therapy (phototherapy)
- Exchange transfusions (removing the child’s blood and replacing it with fresh donor blood or plasma)
In preterm infants, the risk of a handicap increases by 30% for each 2.9 mg/dL increase of maximal total bilirubin concentration. While central nervous system damage is rare when total serum bilirubin is less than 20 mg/dL, premature infants may be affected at lower levels. The decision to institute therapy is based on a number of factors including total serum bilirubin, age, clinical history, physical examination, and coexisting conditions. Phototherapy typically is discontinued when total serum bilirubin level reaches 14 to 15 mg/dL.
How to manage hyperbilirubinemia in newborn babies
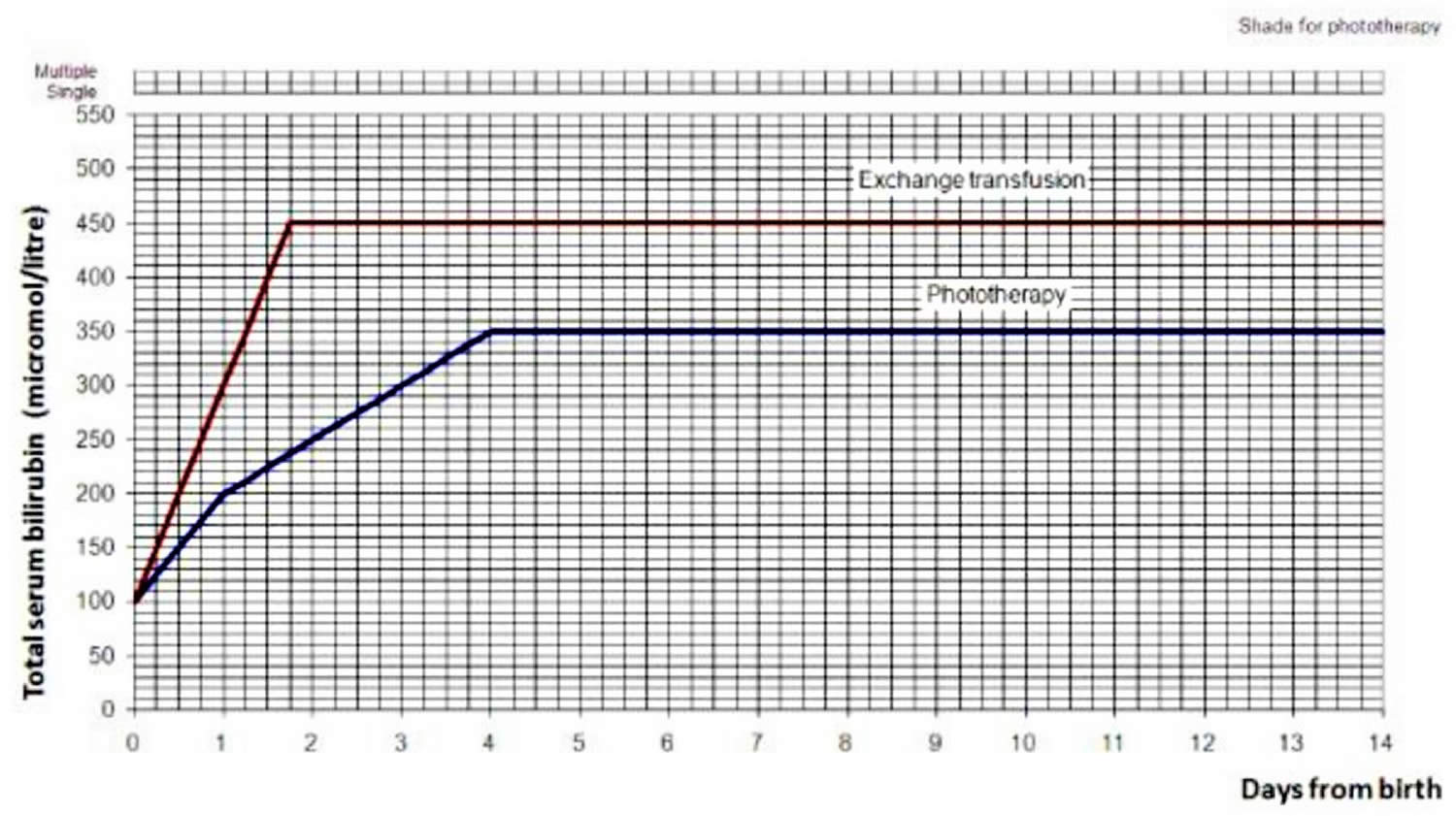
Use the bilirubin level to determine the management of hyperbilirubinemia in all babies (see threshold table (see Table 1) and treatment threshold graphs (Figures 2 and 3).
Table 3. Bilirubin threshold table for the management of babies of 38 weeks or more gestational age with hyperbilirubinemia
| Age (hours) | Bilirubin measurement (micromol/liter) | |||
|---|---|---|---|---|
| 0 | > 100 | > 100 | ||
| 6 | > 100 | > 112 | > 125 | > 150 |
| 12 | > 100 | > 125 | > 150 | > 200 |
| 18 | > 100 | > 137 | > 175 | > 250 |
| 24 | > 100 | > 150 | > 200 | > 300 |
| 30 | > 112 | > 162 | > 212 | > 350 |
| 36 | > 125 | > 175 | > 225 | > 400 |
| 42 | > 137 | > 187 | > 237 | > 450 |
| 48 | > 150 | > 200 | > 250 | > 450 |
| 54 | > 162 | > 212 | > 262 | > 450 |
| 60 | > 175 | > 225 | > 275 | > 450 |
| 66 | > 187 | > 237 | > 287 | > 450 |
| 72 | > 200 | > 250 | > 300 | > 450 |
| 78 | > 262 | > 312 | > 450 | |
| 84 | > 275 | > 325 | > 450 | |
| 90 | > 287 | > 337 | > 450 | |
| 96 | > 300 | > 350 | > 450 | |
| Action | ||||
| Repeat bilirubin measurement in 6–12 hours | Consider phototherapy and repeat bilirubin measurement in 6 hours | Start phototherapy | Perform an exchange transfusion unless the bilirubin level falls below threshold while the treatment is being prepared | |
Figure 2. Hyperbilirubinemia threshold graph for babies
[Source 29 ]Figure 3. Hyperbilirubinemia treatment threshold graph for babies with neonatal jaundice: >=38 weeks gestation
[Source 28 ]What does low bilirubin levels mean?
Low levels of bilirubin are generally not of any concern and are not monitored.
References- Gallagher PG. Abnormalities of the erythrocyte membrane. Pediatr Clin North Am. 2013 Dec;60(6):1349-62. doi: 10.1016/j.pcl.2013.09.001
- Koralkova, P., van Solinge, W.W. and van Wijk, R. (2014), Rare hereditary red blood cell enzymopathies associated with hemolytic anemia – pathophysiology, clinical aspects, and laboratory diagnosis. Int. Jnl. Lab. Hem., 36: 388-397. https://doi.org/10.1111/ijlh.12223
- Martin A, Thompson AA. Thalassemias. Pediatr Clin North Am. 2013 Dec;60(6):1383-91. doi: 10.1016/j.pcl.2013.08.008
- Bass GF, Tuscano ET, Tuscano JM. Diagnosis and classification of autoimmune hemolytic anemia. Autoimmun Rev. 2014 Apr-May;13(4-5):560-4. doi: 10.1016/j.autrev.2013.11.010
- Strassburg CP. Hyperbilirubinemia syndromes (Gilbert-Meulengracht, Crigler-Najjar, Dubin-Johnson, and Rotor syndrome). Best Pract Res Clin Gastroenterol. 2010 Oct;24(5):555-71. doi: 10.1016/j.bpg.2010.07.007
- Erlinger S, Arias IM, Dhumeaux D. Inherited disorders of bilirubin transport and conjugation: new insights into molecular mechanisms and consequences. Gastroenterology. 2014 Jun;146(7):1625-38. doi: 10.1053/j.gastro.2014.03.047
- Fargo MV, Grogan SP, Saguil A. Evaluation of Jaundice in Adults. Am Fam Physician. 2017 Feb 1;95(3):164-168. https://www.aafp.org/pubs/afp/issues/2017/0201/p164.html
- Sun S, Song Z, Cotler SJ, Cho M. Biomechanics and functionality of hepatocytes in liver cirrhosis. J Biomech. 2014 Jun 27;47(9):2205-10. doi: 10.1016/j.jbiomech.2013.10.050
- Suhail M, Abdel-Hafiz H, Ali A, Fatima K, Damanhouri GA, Azhar E, Chaudhary AG, Qadri I. Potential mechanisms of hepatitis B virus induced liver injury. World J Gastroenterol. 2014 Sep 21;20(35):12462-72. doi: 10.3748/wjg.v20.i35.12462
- Levitt DG, Levitt MD. Quantitative assessment of the multiple processes responsible for bilirubin homeostasis in health and disease. Clin Exp Gastroenterol. 2014 Sep 2;7:307-28. doi: 10.2147/CEG.S64283
- Roche SP, Kobos R. Jaundice in the adult patient. Am Fam Physician. 2004;69(2):299-304. https://www.aafp.org/pubs/afp/issues/2004/0115/p299.html
- Rocco A, Compare D, Angrisani D, Sanduzzi Zamparelli M, Nardone G. Alcoholic disease: liver and beyond. World J Gastroenterol. 2014 Oct 28;20(40):14652-9. doi: 10.3748/wjg.v20.i40.14652
- Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015 Apr;62(1 Suppl):S47-64. doi: 10.1016/j.jhep.2014.12.012
- Bauer M, Press AT, Trauner M. The liver in sepsis: patterns of response and injury. Curr Opin Crit Care. 2013 Apr;19(2):123-7. doi: 10.1097/MCC.0b013e32835eba6d
- Kosters A, Karpen SJ. The role of inflammation in cholestasis: clinical and basic aspects. Semin Liver Dis. 2010 May;30(2):186-94. doi: 10.1055/s-0030-1253227
- Chen M, Suzuki A, Borlak J, Andrade RJ, Lucena MI. Drug-induced liver injury: Interactions between drug properties and host factors. J Hepatol. 2015 Aug;63(2):503-14. doi: 10.1016/j.jhep.2015.04.016
- Wooton-Kee CR, Jain AK, Wagner M, Grusak MA, Finegold MJ, Lutsenko S, Moore DD. Elevated copper impairs hepatic nuclear receptor function in Wilson’s disease. J Clin Invest. 2015 Sep;125(9):3449-60. doi: 10.1172/JCI78991
- Vuppalanchi R, Liangpunsakul S, Chalasani N. Etiology of new-onset jaundice: how often is it caused by idiosyncratic drug-induced liver injury in the United States? Am J Gastroenterol. 2007 Mar;102(3):558-62; quiz 693. doi: 10.1111/j.1572-0241.2006.01019.x
- Cafasso DE, Smith RR. Symptomatic cholelithiasis and functional disorders of the biliary tract. Surg Clin North Am. 2014 Apr;94(2):233-56. doi: 10.1016/j.suc.2013.12.001
- Fang Y, Gurusamy KS, Wang Q, Davidson BR, Lin H, Xie X, Wang C. Pre-operative biliary drainage for obstructive jaundice. Cochrane Database Syst Rev. 2012 Sep 12;9(9):CD005444. doi: 10.1002/14651858.CD005444.pub3
- Luu MB, Deziel DJ. Unusual complications of gallstones. Surg Clin North Am. 2014 Apr;94(2):377-94. doi: 10.1016/j.suc.2014.01.002
- Winger J, Michelfelder A. Diagnostic approach to the patient with jaundice. Prim Care. 2011 Sep;38(3):469-82; viii. doi: 10.1016/j.pop.2011.05.004
- Mortelé KJ, Wiesner W, Cantisani V, Silverman SG, Ros PR. Usual and unusual causes of extrahepatic cholestasis: assessment with magnetic resonance cholangiography and fast MRI. Abdom Imaging. 2004 Jan-Feb;29(1):87-99. doi: 10.1007/s00261-003-0062-6
- Krishna RP, Lal R, Sikora SS, Yachha SK, Pal L. Unusual causes of extrahepatic biliary obstruction in children: a case series with review of literature. Pediatr Surg Int. 2008 Feb;24(2):183-90. doi: 10.1007/s00383-007-2087-3
- Dickson PV, Behrman SW. Distal cholangiocarcinoma. Surg Clin North Am. 2014 Apr;94(2):325-42. doi: 10.1016/j.suc.2013.12.004
- Brown KM, Geller DA. Proximal biliary tumors. Surg Clin North Am. 2014 Apr;94(2):311-23. doi: 10.1016/j.suc.2013.12.003
- Wernberg JA, Lucarelli DD. Gallbladder cancer. Surg Clin North Am. 2014 Apr;94(2):343-60. doi: 10.1016/j.suc.2014.01.009
- National Collaborating Centre for Women’s and Children’s Health (UK). Neonatal Jaundice. London: RCOG Press; 2010 May. (NICE Clinical Guidelines, No. 98.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK65119
- https://bilitool.org/